B. Pokhis et al. / HEALTH 1 (2009) 188-191
SciRes Copyright © 2009 Openly accessible at http://www.scirp.org/journal/HEALTH/
190
at the operation day scheduled, equally distributed in the
four groups. In one patient in the fentanyl 10 sec group the
syringe with the study medication was dislocated during
the injection. Therefore the patient was excluded from
evaluation. Thus, enrolment, allocation and follow up of
the patients were highly conformable to the study proto-
col.
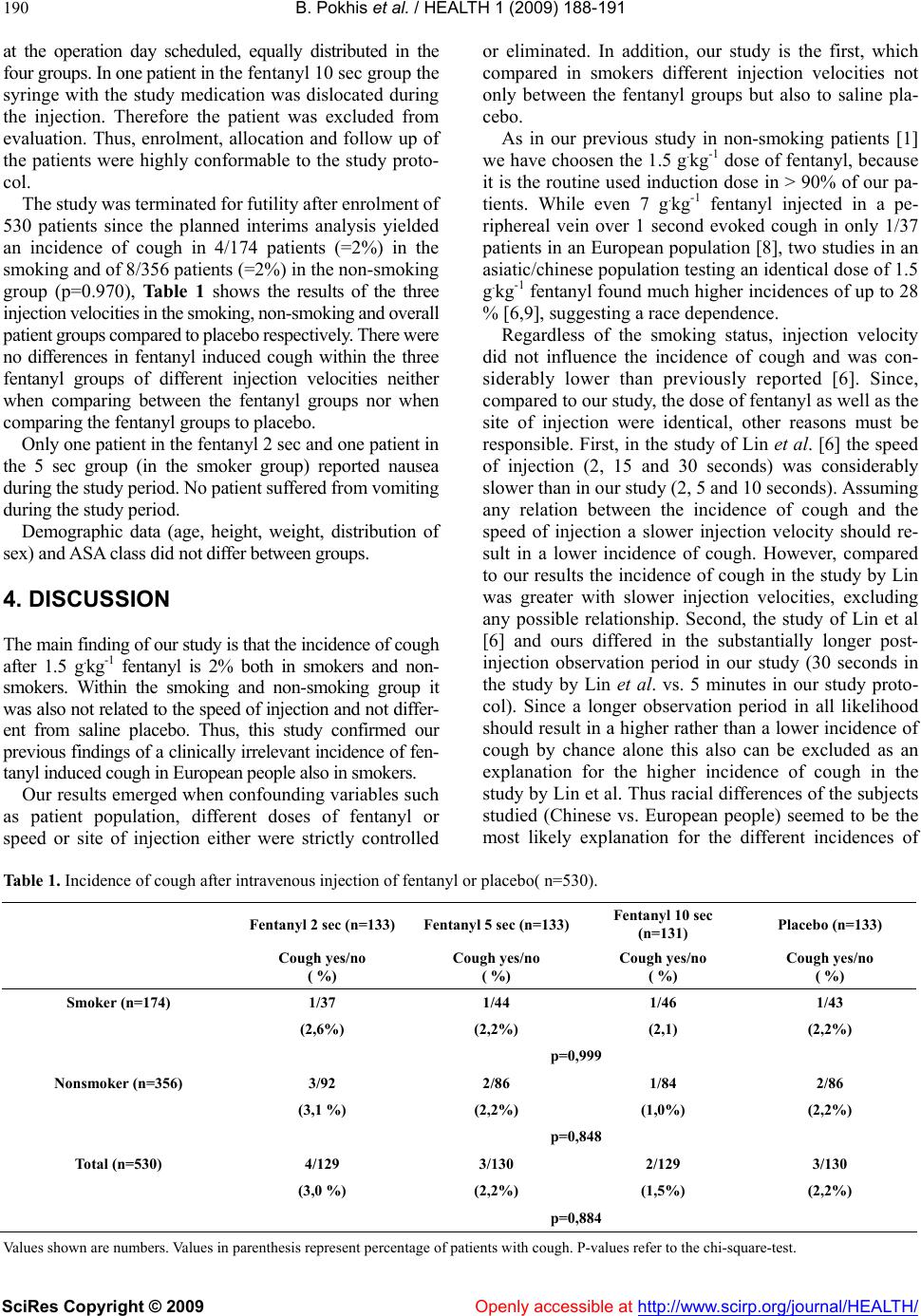
The study was terminated for futility after enrolment of
530 patients since the planned interims analysis yielded
an incidence of cough in 4/174 patients (=2%) in the
smoking and of 8/356 patients (=2%) in the non-smoking
group (p=0.970), Table 1 shows the results of the three
injection velocities in the smoking, non-smoking and overall
patient groups compared to placebo respectively. There were
no differences in fentanyl induced cough within the three
fentanyl groups of different injection velocities neither
when comparing between the fentanyl groups nor when
comparing the fentanyl groups to placebo.
Only one patient in the fentanyl 2 sec and one patient in
the 5 sec group (in the smoker group) reported nausea
during the study period. No patient suffered from vomiting
during the study period.
Demographic data (age, height, weight, distribution of
sex) and ASA class did not differ between groups.
4. DISCUSSION
The main finding of our study is that the incidence of cough
after 1.5 g.kg-1 fentanyl is 2% both in smokers and non-
smokers. Within the smoking and non-smoking group it
was also not related to the speed of injection and not differ-
ent from saline placebo. Thus, this study confirmed our
previous findings of a clinically irrelevant incidence of fen-
tanyl induced cough in European people also in smokers.
Our results emerged when confounding variables such
as patient population, different doses of fentanyl or
speed or site of injection either were strictly controlled
or eliminated. In addition, our study is the first, which
compared in smokers different injection velocities not
only between the fentanyl groups but also to saline pla-
cebo.
As in our previous study in non-smoking patients [1]
we have choosen the 1.5 g.kg-1 dose of fentanyl, because
it is the routine used induction dose in > 90% of our pa-
tients. While even 7 g.kg-1 fentanyl injected in a pe-
riphereal vein over 1 second evoked cough in only 1/37
patients in an European population [8], two studies in an
asiatic/chinese population testing an identical dose of 1.5
g.kg-1 fentanyl found much higher incidences of up to 28
% [6,9], suggesting a race dependence.
Regardless of the smoking status, injection velocity
did not influence the incidence of cough and was con-
siderably lower than previously reported [6]. Since,
compared to our study, the dose of fentanyl as well as the
site of injection were identical, other reasons must be
responsible. First, in the study of Lin et al. [6] the speed
of injection (2, 15 and 30 seconds) was considerably
slower than in our study (2, 5 and 10 seconds). Assuming
any relation between the incidence of cough and the
speed of injection a slower injection velocity should re-
sult in a lower incidence of cough. However, compared
to our results the incidence of cough in the study by Lin
was greater with slower injection velocities, excluding
any possible relationship. Second, the study of Lin et al
[6] and ours differed in the substantially longer post-
injection observation period in our study (30 seconds in
the study by Lin et al. vs. 5 minutes in our study proto-
col). Since a longer observation period in all likelihood
should result in a higher rather than a lower incidence of
cough by chance alone this also can be excluded as an
explanation for the higher incidence of cough in the
study by Lin et al. Thus racial differences of the subjects
studied (Chinese vs. European people) seemed to be the
most likely explanation for the different incidences of
Table 1. Incidence of cough after intravenous injection of fentanyl or placebo( n=530).
Fentanyl 2 sec (n=133)Fentanyl 5 sec (n=133)Fentanyl 10 sec
(n=131) Placebo (n=133)
Cough yes/no
( %)
Cough yes/no
( %)
Cough yes/no
( %)
Cough yes/no
( %)
Smoker (n=174) 1/37 1/44 1/46 1/43
(2,6%) (2,2%) (2,1) (2 ,2%)
p=0,999
Nonsmoker (n=356) 3/92 2/86 1/84 2/86
(3,1 %) (2,2%) (1,0%) (2,2 %)
p=0,848
Total (n=530) 4/129 3/130 2/129 3/130
(3,0 %) (2,2%) (1,5%) (2,2 %)
p=0,884
Values shown are numbers. Values in parenthesis represent percentage of patients with cough. P-values refer to the chi-square-test.