A. T ro edhan et al. / Open Journal of Stomatology 1 (2011) 179-184
184
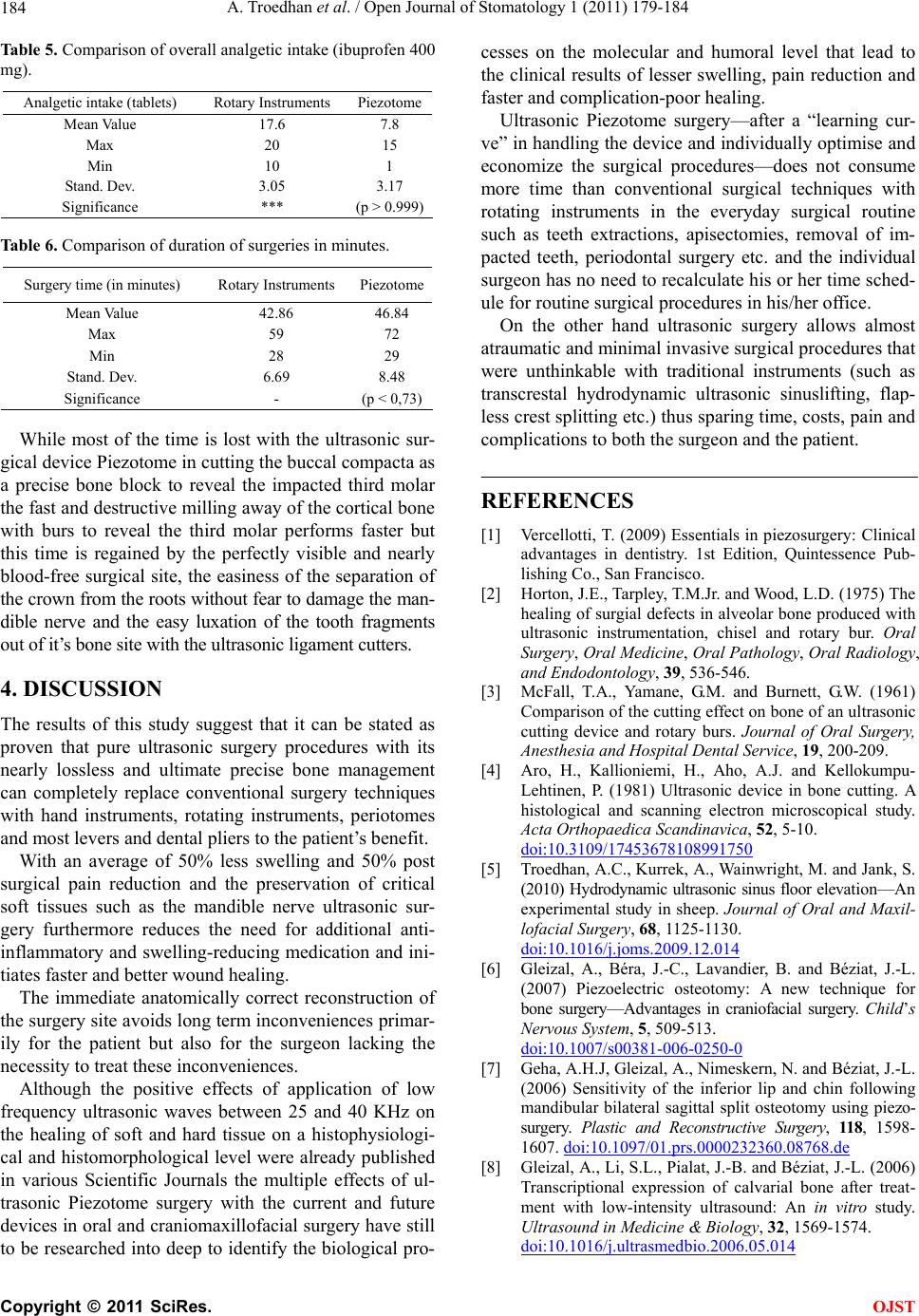
Table 5. Comparison of overall analgetic intake (ibuprofen 400
mg).
Analgetic intake (tablets) Rotary Instruments Piezotome
Mean Value 17.6 7.8
Max 20 15
Min 10 1
Stand. D e v. 3.05 3.17
Significance *** (p > 0.999)
Table 6. Comparison of duration of surgeries in minutes.
Surgery time (in minutes) Rotary Instruments Piezotome
Mean Value 42.86 46.84
Max 59 72
Min 28 29
Stand. D e v. 6.69 8.48
Significance - (p < 0,73)
While most of the time is lost with the ultrasonic sur-
gical device Piezotome in cutting the buccal compacta as
a precise bone block to reveal the impacted third molar
the fast and destructive milling away of th e cortical bone
with burs to reveal the third molar performs faster but
this time is regained by the perfectly visible and nearly
blood-free surgical site, the easiness of the separation of
the crown from the roots without fear to damage the man-
dible nerve and the easy luxation of the tooth fragments
out of it’s bone site with the ultrasonic ligament cutters.
4. DISCUSSION
The results of this study suggest that it can be stated as
proven that pure ultrasonic surgery procedures with its
nearly lossless and ultimate precise bone management
can completely replace conventional surgery techniques
with hand instruments, rotating instruments, periotomes
and most levers and dental pliers to the patient’s benefit.
With an average of 50% less swelling and 50% post
surgical pain reduction and the preservation of critical
soft tissues such as the mandible nerve ultrasonic sur-
gery furthermore reduces the need for additional anti-
inflammatory and swelling-reducing medication and ini-
tiates faster and better wound healing.
The immediate anatomically correct reconstruction of
the surgery site avoids long term inconveniences primar-
ily for the patient but also for the surgeon lacking the
necessity to treat these inconvenien ces.
Although the positive effects of application of low
frequency ultrasonic waves between 25 and 40 KHz on
the healing of soft and hard tissue on a histophysiologi-
cal and histomorphological level were already published
in various Scientific Journals the multiple effects of ul-
trasonic Piezotome surgery with the current and future
devices in oral and craniomax illofacial surgery have still
to be rese arched into d eep to identify the bio logical pro-
cesses on the molecular and humoral level that lead to
the clinical results of lesser swelling, pain reduction and
faster and complication -poor healing.
Ultrasonic Piezotome surgery—after a “learning cur-
ve” in handling the device and individually optimise and
economize the surgical procedures—does not consume
more time than conventional surgical techniques with
rotating instruments in the everyday surgical routine
such as teeth extractions, apisectomies, removal of im-
pacted teeth, periodontal surgery etc. and the individual
surgeon has no need to recalculate his or her time sched-
ule for routine surgical procedures in his/he r office.
On the other hand ultrasonic surgery allows almost
atraumatic and minimal invasive surgical procedures that
were unthinkable with traditional instruments (such as
transcrestal hydrodynamic ultrasonic sinuslifting, flap-
less crest splitting etc.) thus sp aring time, costs, pain and
complications to both the surgeon and the patient.
REFERENCES
[1] Vercellotti, T. (2009) Essentials in piezosurgery: Clinical
advantages in dentistry. 1st Edition, Quintessence Pub-
lishing Co., San Francisco.
[2] Horton, J.E., Tarpley, T.M.Jr. and Wood, L.D. (1975) The
healing of surgial defects in alveolar bone produced with
ultrasonic instrumentation, chisel and rotary bur. Oral
Surgery, Oral Medicine, Oral Pathology, Oral Radiology,
and Endodontology, 39, 536-546.
[3] McFall, T.A., Yamane, G.M. and Burnett, G.W. (1961)
Comparison of the cutting effect on bone of an ultrasonic
cutting device and rotary burs. Journal of Oral Surgery,
Anesthesia and Hospital Dental Service, 19, 200-209.
[4] Aro, H., Kallioniemi, H., Aho, A.J. and Kellokumpu-
Lehtinen, P. (1981) Ultrasonic device in bone cutting. A
histological and scanning electron microscopical study.
Acta Orthopaedica Scandinavica, 52, 5-10.
doi:10.3109/17453678108991750
[5] Troedhan, A.C., Kurrek, A., Wa inwright, M. and Jank, S.
(2010) Hydrodynamic ultrasonic sinus floor elevation—An
experimental study in sheep. Journal of Oral and Maxil-
lofacial Surgery, 68, 1125-1130.
doi:10.1016/j.joms.2009.12.014
[6] Gleizal, A., Béra, J.-C., Lavandier, B. and Béziat, J.-L.
(2007) Piezoelectric osteotomy: A new technique for
bone surgery—Advantages in craniofacial surgery. Child’s
Nervous System, 5, 509-513.
doi:10.1007/s00381-006-0250-0
[7] Geha, A.H.J, Gleizal, A., Nimeskern, N. and Béziat, J.-L.
(2006) Sensitivity of the inferior lip and chin following
mandibular bilateral sagittal split osteotomy using piezo-
surgery. Plastic and Reconstructive Surgery, 118, 1598-
1607. doi:10.1097/01.prs.0000232360.08768.de
[8] Gleizal, A., Li, S.L., Pialat, J.-B. and Béziat, J.-L. (2006)
Transcriptional expression of calvarial bone after treat-
ment with low-intensity ultrasound: An in vitro study.
Ultrasound in Medicine & Biology, 32, 1569-1574.
doi:10.1016/j.ultrasmedbio.2006.05.014
C
opyright © 2011 SciRes. OJST