Health
Vol.10 No.04(2018), Article ID:84131,9 pages
10.4236/health.2018.104037
Sparing Treatment of Thoracic and Abdominal Aortic Aneurysms
V. P. Krylov, D. E. Shevtsov, G. A. Popel, A. S. Zhigalkovich, V. N. Gaiduk, L. I. Reut, A. L. Smolyakov, L. G. Shestakova, N. V. Mankevich
Belarusian Association of Physicians Republican Research and Practical Centre “Cardiology”, Minsk, Belarus

Copyright © 2018 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: March 21, 2018; Accepted: April 25, 2018; Published: April 28, 2018
ABSTRACT
A comparison of results of sparing treatment obtained at 2, 4 and 6 years of follow-up in subjects with descending aortic atherosclerotic aneurysms (DAAs), and during the period between 1.5 and 8.9 years in subjects with dissecting thoracoabdominal aortic aneurysms (DTAAs) has been made. All subjects received conservative treatment to maintain optimal levels of BP, cholesterol and LDL cholesterol, as well as to reduce oxidative and inflammatory processes in aorta, strengthen aortic walls and stabilize the course of the disease. Rapid negative changes (diameter increased by more than 5 mm within a 6-month period) and the absence of contraindications for surgery prompted us to perform open or endovascular aortic repair. Available data suggest that both DAAs and TAAs are comorbidities, which at any time can abruptly terminate patient’s life, and operative treatment guarantees no safety from ruptures. When using sparing treatment of DAA, survival rates were 90.1% at 2 years, 76.8% at 4 years, and 59.4% at 6 years, with uniform survival increment mainly due to comorbidity. Survival rate seen in TAA group (81.8%) was more acceptable due to a younger age of patients.
Keywords:
Atherosclerotic and Dissecting Aneurysms, Inflammation, Surgical and Medical Treatment, Long-Term Results

1. Introduction
The only reliable treatment modality used to treat DAA and TAA has been so far an operative intervention. This is explained by a lack of investigations to study the etiopathogenesis of the disease and small experience in medical correction of those conditions. Still, the number of indications for surgical treatment for these patients is beginning to narrow. Improvements that have been achieved in the open surgery, wide spread of puncture methods of stent-graft implantation, medication regimens using symptomatic and etiopathogenetic principles allowed for a critical assessment of the results. They showed that none of the existing methods is superior when it comes to DAA and TAA treatment.
Moreover, it is becoming clear that atherosclerosis per se is not probably the primary cause of the development and progression of the disease. The underlying conditions may involve molecular and genetic defects and connective tissue dysfunctions due to which atherosclerosis and progressive inflammatory process form a local aortic wall incompetence. Multiple investigations suggest that at very early stages, they have much in common concerning mechanisms involved and serve as allies, whereas later each of them, having established its own way to enable the pathologic process, becomes a competitor [1] [2] .
Further investigations are needed to deepen our understanding of the field, but it is getting more obvious that current surgical methods to treat DAA do not fully correspond to the pathogenesis of the disease and are not always justified [3] [4] .
In this regard, EVAR 1 publications about DAA treatment in subjects at age 60 or above, with TAA diameter of more than 5.5 cm over a 4-year follow-up period, are of great interest. All-cause mortality after endovascular surgery and open repair was not significantly different. The EVAR-2 data showed that the number of deaths due to aneurysm rupture in groups of conservative treatment was consistent with the number of ruptures and post-operation mortality rate seen in the group of endovascular treatment [5] [6] [7] .
Scientific community is trying to understand the reason for such a high mortality in DAA. Deaths occur as a result of ruptured aneurysm, concomitant polyorgan insufficiency, and excessive indications for treatment [8] [9] . It is noteworthy that in most cases, no signs of fatal outcomes can be identified.
Almost 2% of patients die with acute DAA within 1 hour, and 17% die within 2 years [10] . Scarce reports exist discussing follow-ups of these individuals. Thus, available data [11] [12] show a 5-year mortality in subjects who survived the acute phase not exceeding 10% - 15%.
Some success has been attained in treatment of inflammatory process and regulations of indications to treat DAA and dissecting aneurysms (ADs), and this has produced some positive results [10] . In recent years, increasingly more publications on medications aimed at both symptomatic DAA treatment, and aortic wall strengthening have appeared. However, from our perspective, these works describing algorithms of medical treatment are restricted to a mispresentation of DAA etiopathogenesis [2] [13] [14] .
Objective of the study: was to investigate the dynamics of the disease in patients with DAA at 2, 4 and 6 years and in patients with ADs at 1.5 - 8.9 years.
2. Materials and Methods
Patient Characteristics
Databases of Vascular Surgery department of RRPC “Cardiology” contained data on 300 patients with descending aortic aneurysms (thoracic aortic aneurysms (TAAs) and abdominal aortic aneurisms (AAAs)) and aortic dissections referred to the Centre over the past 9 years with subacute and chronic condition.
Patients with DAAs were studied during a 2-, 4- and 6-year period, and 33 out- and in-patients with aortic dissections were studied during the period between 1.5 and 9 years (Table 1).
Only patients with thoracic and/or abdominal atherosclerotic aortic aneurysms were examined during a 2-, 4- and 6-year period, and 33 subjects with dissecting AAs subjected to atherosclerosis with DeBakey type 1 and 3b who were treated in in- and outpatient settings over a period between 1.5 and 9 years (average 4.75 years) (Table 1).
None of the parameters in DAA groups reached statistical significance, and it allowed us to equally analyze changes in both patients’ state and course of the disease. Individuals with ADs had similar parameters including baseline aneurysm maximum diameters compared to those with DAAs. At the same time, they were evidently younger (р < 0.001).
3. Methods
1) Clinical investigations involving CTA, aortic angiography, coronary angiography, and US.
2) Surgical treatment: aortic iliofemoral bifurcation prosthesis, aortic arch replacement and endovascular grafting.
3) Medical therapy to strengthen aortic wall: continuous combination of ACEI with amlodipine, b-blockers, statins. Courses of macrolide antibiotics (roxithromycin, azithromycin) if signs of inflammatory process are present (as evidenced by CRP), and symptomatic treatment.
Table 1. Key characteristics of study groups.
4) Statistical methods. Calculation of probability and reliability, and estimates thereof for bio-data analysis [15] .
4. Results
Sparing treatment efficacy assessment was performed in groups receiving aorta-strengthening medical therapy to prevent its ongoing transformation, with operative treatment typically offered in cases of explicit threat of aneurysm rupture. Follow-up control of these groups was made every 3 to 6 months documenting general condition, aneurysm size, BP, lipid spectrum, inflammatory markers, and signs of complications or comorbidities.
Conservative treatment to attain and maintain optimal BP, target cholesterol and LDL, as well as to reduce oxidative and inflammatory processes in aorta, strengthen its walls and stabilize the progression of the disease was permanent in all subjects including post-operation period. If negative trends (aortic diameter increased by more than 5 mm within 6 months) were present and there were no contraindications for surgery, we performed open repair surgery or endovascular aortic repair.
Table 2 contains data on key parameters presenting the course of DAA and treatment outcomes.
Within 6 years, 39 out of 96 subjects with DAA died which accounted for 40.62%. Over a 2-year follow-up period (4 to 6 years), no patients received operative treatment and there were no cases of aortic ruptures in operated subjects. In non-operated individuals, rupture occurred every 2 years in two patients, which accounted for only 8.3%. As a percentage, aneurysm rupture in the period between 2 and 4 years among operated and non-operated individuals was absolutely similar (8.3% vs. 8%, respectively), while during 4 to 6-year period, it was almost similar (8.3% vs. 11.1%). Thus, within 6 years, aneurysm rupture was registered in 10 subjects, and two died due to post-operative complications, and
Table 2. Comparison of mortality rates in patients with DAA based on the follow-up period, i.e. 2, 4, 6 years, and patients with AD within 4.75 ± 0.47 years resulted from sparing treatment modality to treat aortic aneurysms.
surgery-related mortality increased up to 16.7%.
The primary cause of death throughout the follow-up period, however, was comorbidity (CVDs, cancer, diabetes mellitus, renal and other polyorgan insufficiency) which resulted in 27 (28.1%) deaths of patients with DAA. None of those patients could have been operated. Physical status of all patients suggested the risk of surgery that exceeded the risk of conservative treatment. Significant mortality differences due to comorbidities among conservative and surgical treatment modalities (31.9% vs. 16.7%, respectively) might be explained by younger age and better somatic viability of operated subjects. The survival was as well influenced by this factor; within 6 years, it was 59.6% in conservative treatment group, and 66.7% in surgical treatment group.
Throughout the follow-up period, the group of conservative treatment annually includes 5 to 6 patients who die, and these subjects are typically older and more physically weak. Similar trend is observed among operated individuals. Survival rates are progressively reduced in both groups, with a slightly more prominent escalation among conservatively treated subjects.
Of 33 subjects with AD, 10 (10.3%) were operated, with four of them receiving ascending aortic replacement, two receiving open abdominal aortic repair, and 4 implanted with a stent-graft. The remaining 23 patients (69.7%) were treated conservatively.
During that period, six patients (18.1%) died. One patient was operated and received a stent-graft, but after four years, aneurysm rupture occurred at its distal edge. In the group of conservative treatment, five (15.2%) patients died; 2 due to aneurysm rupture (6%). Thus, as a percentage, mortality rate due to ruptured aneurysm in operated individuals turned out to be higher than in non-operated (10% vs. 8.7%, respectively).
The main cause of death in three (9.1%) patients includes comorbidity (stroke, short-term lower extremity gangrene during 8 months of follow-up). Survival throughout the group (operated and non-operated-27 patients) was 81.8%.
5. Discussion
Major events in DAA and AD were reported at the beginning of the treatment when the threat of aneurysm rupture, technical feasibility of stent-graft implantation and the absence of contraindications for open aortic repair had been thoroughly assessed. A group of patients was selected in which the sole option was medical correction to strengthen aneurysm walls, treat inflammatory process and maintain BP within 132/78 mm・Hg. Generally, it was used in all the individuals, but the rest had an alternative-surgical treatment.
However, the proven procedure of DAA patient management is more often than not intervened by a crucial factor that can change patients’ fate at the very beginning. That is compliance! Lack of compliance brings doctors’ efforts to naught. Ruptured aneurysms are strongly related with carelessness of treatment and physical stresses in the first several years, as aneurysm wall has not fully restored. Therefore, the intensity of aortic ruptures tended to decline overtime. During the past 3 years, no cases of ruptured aneurysms were registered in operated patients, with only two cases reported in the sixth year of follow-up among non-operated subjects of older age. Similar was true for AD group.
However, the real problem afflicting patients suffering aneurysms, which uniformly boosted death rates with age was comorbidity. Thus, over 4, 5 and 6 years, 1, 2 and 4 patients (4.2%, 8.3%, and 16.7%, respectively) died. The similar trend was seen among non-operated, but was more prominent, i.e. 12, 18, and 23 (16%, 24.7%, 31.9%) subjects.
It might seem that the situation with conservative treatment of DAA is poorer than with operative (Table 2) treatment, but two operation-related fatal outcomes (8.3%) in the second and third follow-up year nullified the results. Therefore, among the survivors, there were no significant differences between those operated and non-operated. Given that the open aortic surgery is performed only to prevent rupture, it becomes clear that the aim is hard to achieve. In this regard, surgical approach to treat DAA shall not to be considered the best possible treatment modality.
In patients with AD, given their much younger age, no peculiar presentation of comorbidity was evident. Six patients died in this group, with three of them due to ruptured aneurysm (one following stent-graft implantation) and three due to concomitant conditions.
6. Conclusions
Our data suggest that DAA belongs to a nosology of comorbid disorders, which can abruptly terminate a person’s life. Cardiovascular diseases, diabetes mellitus, cancer, polyorgan insufficiency prevail, and aneurysm rupture is just a part of it. Operative treatment guarantees no safety from rupture or other cause of death. Data from multi-centered trials support these findings [5] [6] . At least, the ruptured aneurysm is not a leading factor contributing to fatal outcomes, and the threat of rupture can be mostly managed medically. Such decision provides ground for an in-depth search for an underlying condition and change of basic approaches to treat aortic aneurysms [16] [17] [18] [19] .
Aortic aneurysms must be treated with caution, as there is a wide variety of factors responsible for a fatal outcome. The acute and chronic patients require intensive medical therapy based on etiopathogenesis with a special focus on inflammatory process signs.
Groups of AD patients showed changes consistent with those registered in DAA group with some definable patterns characteristic for a younger age including fewer comorbidities. High CRP was another peculiar finding. Yet, some other factor seems to be mainly responsible for ruptured aneurysms, which is non-compliance. Non-compliance was responsible for ruptured aneurysms both in DAAs, and in ADs.
No doubt that the severe hypertension and aortic stiffness coupled with excessive static and emotional stress contribute to the development of AD and DAA. It is noteworthy that these conditions are common among most people, while dissected and ruptured aortas are still quite rare. Then there must be some other factors involved in the condition. One of them is evident―inflammatory process. Nevertheless, since some patients’ CRP remain very low, one can assume the presence of some defect in aortic wall, congenital or acquired, with structural changes of collagen and elastin (for example, flattened wave elastin fibers [20] ).
Our experience of treating patients who survived acute AD episode suggests that the dissection is not as dramatic as it might be depicted in literature [11] [12] , with a 5-year survival amounting to 10% - 15% in the natural course of the disease. Our study shows general survival to be 81.9% provided a properly selected etiopathogenetic therapeutic strategy.
Acute period of dissecting aneurysm, timely diagnosis and awareness of the presence of severe pains remains a challenge when it comes to a decision-making, but using proper diagnosis and intensive treatment to control BP we can halt dissection which influenced by pathogenetically justified therapy, may later on lead patients into a chronic phase. Operations to treat thoracoabdominal lesions are challenging due to a practical impossibility of their complete repair, which is always potentially associated with fatal outcome.
Thus, when using DAA sparing treatment strategy, 2, 4 and 6-year survival rates were 90.1%, 76.8% and 59.4%, respectively, with uniform mortality increment mainly due to present comorbidity. Survival in AD group (81.8%) turned out to be more acceptable due to a younger age of individuals (Graph 1).
When assessing these results, it should be borne in mind, however, that there is a natural population decline. Based on statistical yearbook data, decline over the past 6 years for these age groups was more than 2% annually in Minsk. It is
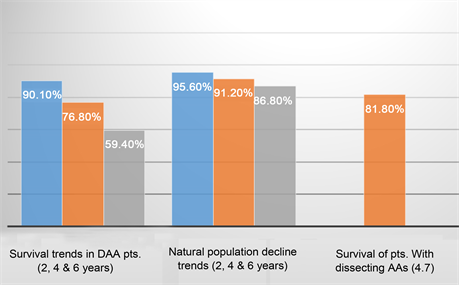
Graph 1. Survival seen in patients with DAA and dissecting AA at 2, 4 and 6 years of follow-up.
more than 12% - 13% at 6 years. Therefore, the year-by-year dynamics of survival from DAA makes it feasible to use sparing treatment strategy with emphasis on gerontology, i.e. operations shall be performed only if there is a potential of aneurysm rupture and inefficiency of conservative treatment.
Complications of treatment, which resulted in death, were observed only in operated patients. Conservatively treated individuals demonstrated no complications. Still, it is noteworthy that early detection of comorbidity and efforts in symptomatic treatment thereof are of paramount importance for longer and productive life.
Cite this paper
Krylov, V.P., Shevtsov, D.E., Popel, G.A., Zhigalkovich, A.S., Gaiduk, V.N., Reut, L.I., Smolyakov, A.L., Shestakova, L.G. and Mankevich, N.V. (2018) Sparing Treatment of Thoracic and Abdominal Aortic Aneurysms. Health, 10, 458-466. https://doi.org/10.4236/health.2018.104037
References
- 1. Nagornev, V.A. (1996) Cytokines, Immune Inflammation and Atherosclerosis. Uspekhi sovremennoy biologii, 2, 320-331. (In Russian)
- 2. Titov, V.N. (1999) Atherosclerosis and Inflammations: Specificity of Atherosclerosis as an Inflammatory Process. Russian Journal of Cardiology, 1999, 5. (In Russian)
- 3. Belov, Y.V. (2010) Our Failures and the Ways to Improve In-Hospital Mortality in Operative Treatment of Thoracoabdominal Aortic Aneurysms. Angiology and Vascular Surgery, 1, 105-112. (In Russian)
- 4. Bokeria, L.А. (2010) Surgery to Treat Thoracic and Thoracoabdominal Aortic Segments: Doctor’s Manual. A.N. Bakoulev Scientific Center for Cardiovascular Surgery, Moscow, 394.
- 5. EVAR Trial Participants (2005) Endovascular Aneurysm Repair versus Open Repair in Patients with Abdominal Aortic Aneurysm (EVAR Trial 1): Randomized Controlled Trial. Lancet, 365, 2179-2186. https://doi.org/10.1016/S0140-6736(05)66627-5
- 6. EVAR Trial Participants (2005) Endovascular Aneurysm Repair and Outcome in Patients Unfit for Open Repair of Abdominal Aortic Aneurysm (EVAR Trial 2): Randomized Controlled Trial. Lancet, 365, 2187-2192. https://doi.org/10.1016/S0140-6736(05)66628-7
- 7. EVAR Trial Participants (2004) Comparison of Endovascular Aneurysm Repair with Open Repair in Patients with Abdominal Aortic Aneurysm (EVAR Trial 1), 30-day Operative Mortality Results: Randomized Controlled Trial. Lancet, 364, 843-848. https://doi.org/10.1016/S0140-6736(04)16979-1
- 8. Gayduk, V.N., et al. (2014) Optimization of Management of Patients with Chronic Atherosclerotic Descending Aortic Aneurysm. Meditsina, 3, 20-26.
- 9. Mankevich, N.V., et al. (2015) Predictors of Progression of Atherosclerotic Descending Aortic Aneurysms and the Correction. Kardiologiya v Belarusi, 5, 63-73.
- 10. Barbukhatti, K.O. (2014) Kuban Registry of Type A Acute Aortic Dissections (KUBRADA). Kardiologiya I serdechnososudistaya khirurgiia, 6, 38-41.
- 11. Abugov, S.A., et al. (2013). Stenting of Thoracic Aortic Aneurysms in for De Bakey Type III Aortic Dissection. Khirurgiia, 2013, 67-72
- 12. Pape, L.A., et al. (2015) Presentation, Diagnosis, and Outcomes of Acute Aortic Dissection. 17-Year Trends from the International Registry of Acute Aortic Dissection. Journal of the American College of Cardiology, 66, 350-358. https://doi.org/10.1016/j.jacc.2015.05.029
- 13. Krylov, V.P., et al. (2014) Can We Change a Look at Atherosclerotic Aortic Aneurism Treatment? Health, 6, 1345-1351. https://doi.org/10.4236/health.2014.612165
- 14. Nikonenko, А.А. (2013) The Role of Cyclophiline A in Pathogenesis of Abdominal Aortic Aneurysm. Kardiologiya I serdechnososudistaya khirurgiia, 6, 39-42.
- 15. Plavinsky, S.L. (2005) Planning, Processing and Presentation of Data Obtained from Biomedical Trials Using SAS System, Biostatistica. SPb MAPO, 559
- 16. Trisvetova, E.L. (2015) Diagnosis and Treatment of Congenital and Multifactorial Disorders of Connective Tissues. National Clinical Guidelines. Minsk.
- 17. Mikhaylov, D.V., et al. (2012) Perspectives of Preventive Treatment of Aneurysms of Major Vessels. Kardiologiya I serdechnososudistaya khirurgiia, 4, 51-56.
- 18. Vammen, S., et al. (2001) Randomized Double Blind Controlled Trial of Roxithromycin for Prevention of Abdominal Aortic Aneurysm Expansion. British Journal of Surgery, 88, 1066-1072.
- 19. King, V.L., et al. (2006) Selective Cyclooxygenase-2 Inhibition with Celecoxibdescreases Angiotensin 11 Induced Abdominal Aortic Aneurysm Formation in Mice. Arteriosclerosis, Thrombosis, and Vascular Biology, 26, 1137-1143. https://doi.org/10.1161/01.ATV.0000216119.79008.ac
- 20. Yuzefovich, N.А., et al. (2007) Morphometric Study to Assess Structural Components of Aortic Tunica Media Normal and Aneurysm-Surrounding Area. Meditsina, 4, 36-41.


