Health
Vol.6 No.16(2014), Article
ID:49552,10
pages
DOI:10.4236/health.2014.616249
Altered Pulmonary Function among the Transport Workers in Dhaka City
Mustafa Mahfuz1*, Tahmeed Ahmed1, Sk. Akhtar Ahmad2, Manzurul Haque Khan2
1Centre for Nutrition and Food Security, International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh
2Department of Occupational and Environmental Health, National Institute of Preventive and Social Medicine (NIPSOM), Dhaka, Bangladesh
Email: *mustafa@icddrb.org
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 2 July 2014; revised 15 August 2014; accepted 1 September 2014
ABSTRACT
Motor vehicular exhaust is threatening to human health in Dhaka city. To find out the extent of respiratory problem among a particular cadre of transport workers, the human hauler helpers (HHH) of Dhaka city, we conducted a cross sectional study from March 2006 to June 2006. We enrolled 108 HHH from Mirpur to Mohakhali and Gabtoli to Mohakhali routes and collected data using a pre tested questionnaire including interview and physical examination. The pulmonary functions of the participants were measured with electronic spirometer. Among the participants with current respiratory problems 69% complained of gradual increase in respiratory problems and 38% gave history of feeling better on weekly holidays. Occurrence of hoarseness of voice (90%) and wheeze (71%) was extremely high among the helpers followed by cough (50%) and nasal irritation (50%). Spirometry showed 41.7% had obstructive and 4.6% had combined features of pulmonary impairment. Logistic regression analysis showed that respondents who worked 24 months or more were 6.9 times more likely to develop respiratory problem than the less exposed group (OR 6.9; 95% CI 3.42, 8.41). This study provides new information on respiratory health of a specific group of transport workers in Dhaka city which warrants further evaluation with a representing sample covering other areas of Dhaka city among all transport workers.
Keywords:Motor Vehicle, Air Pollution, Human Hauler, Spirometry, Helper, Dhaka

1. Introduction
Respiratory diseases among the city dwellers are a common problem throughout the world [1] . Air pollution is one of the major contributors of respiratory problems and the main source of air pollution is due to suspended particles from the motor exhaust [2] . Dhaka, the capital of Bangladesh is one of the most populous cities of the world [3] . Respiratory problem following air pollution in Dhaka is serious due to increasing population and associated motorization [4] . One of the main reasons of respiratory problems in Dhaka is the smoke emitted from the automobiles [5] . Initial estimate reveals that motor vehicles of Dhaka city annually emit 3700 tons of particulate matters, 8550 tons of nitrogen gases and 50,700 tons of carbon di-oxide [5] which is much higher than the acceptable level [4] .
Motor engine exhaust emissions contain hundreds of chemical compounds, which are emitted partly in the gaseous phase and partly in the particulate phase of the exhaust [6] . The vehicles emit primary pollutants like carbon monoxide, hydrocarbon, oxides of nitrogen and sulfur and particulate including smoke [7] -[9] . In addition to these pollutants, secondary pollutants result in the atmosphere through chemical reaction among the vehicle emission and the normal atmosphere constituents [6] . Evidences suggested that these substances have strong role in developing systemic and inflammatory changes in respiratory system [6] . Individuals who were exposed for a longer duration might develop irritation of the nose and throat, cough, chest tightness, wheezing and shortness of breath [10] -[12] . Moreover, exposure to outdoor air pollutants with predominant particulate matter from vehicular exhaust has been associated with exacerbation of airway oxidative stress, bronchial reactivity and inflammation in the lungs, which may aggravate chronic respiratory symptoms and increase the frequency or intensity of asthma attacks [6] [13] -[15] . Therefore, people like drivers and transport workers are always at high risk due to their occupational exposure in these highly pollutant environment [13] [16] -[18] .
There are different types of motor vehicles in Dhaka city. Human haulers are one of them. After banning of two stroke engines from Dhaka and withdrawal of rickshaws from main roads their number increased in last two or three years. Although for the last few years more than 1000 city buses playing the major role of urban transport system, still human haulers are playing an important role as one of the most convenient transport for the lower middle class [19] . According to Bangladesh road transport authority (BRTA) there were 809 registered human haulers in Dhaka in the year 2004 [19] . In some routes like Mirpur to Mohakhali, human haulers are the major means of public transport, as there are limited bus services connecting these roads. The passengers enter into this van shaped vehicle from back and the helper of this vehicle stands on the rear most part of it, standing on a footplate and keeping balance by holding the vehicle with one hand. The distinguishing feature of the human hauler is that its exhaust pipe lies near the footrest where the helper stands. The human hauler helpers (HHH) take breath in ambient air of the busiest roads of Dhaka and also inhale exhaust from the older and intensively used engines of their own vehicles. According to the motor vehicle ordinance, 1983 (15a) “helper-cumcleaner”, in relation to a transport vehicle, means a person engaged to assist the driver or the conductor in performing his functions and also to clean a motor vehicle [20] . HHHs are the assistants of the drivers. They deal with passengers, manage their accommodation in the vehicle, collect fairs and also direct the driver from back. These helpers are the typical transport workers of Dhaka city, representing 9.3 percent of the total working age population in the city [21] . There are limited evidence related to level of air pollutants from vehicular exhaust and how much Dhaka city dwellers are exposed to them [22] -[24] . However, we found no data on respiratory morbidities among drivers or transport workers of Dhaka city in Pub Med database. Therefore, we conducted this cross sectional study to find out the extent of respiratory problem, among the HHH of Dhaka city.
2. Materials and Methods
2.1. Study Design
It was a cross-sectional study among the HHH of the two major routes of Dhaka city in between March, 2006 to June, 2006.
2.2. Study Population
All helpers of human haulers of Dhaka city, who had worked in this position for at least 6 months, were our study population. Exclusion criteria include working less than 6 months as transport worker, suffering from acute respiratory infection at the time of data collection (pneumonia, acute bronchitis, fever with cough and cold) and did not provide consent to participate in the study. Due to convenience and budgetary constrains two routes namely Mirpur to Mohakhali and Gabtoli to Mohakhali had been selected purposively. According to “Human Hauler Owner’s Association of Mirpur” a total of 180 human haulers used to ply on these two routes and a total of 210 individuals were employed as helpers of those Human haulers in 2005.
2.3. Sample size
For determination of sample size the formula 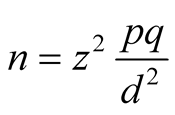 was used.
was used.
Here n = sample size.
z = standard normal deviation usually set at 95% CI which is 1.96.
p = the anticipated population proportion having respiratory problem.
q =1 − p = 0.5.
d = degree of error = 10% or 0.1.
Thus the estimates sample size of 96 would be sufficient for the purpose of the study. Considering possible incompleteness of interviews and withdrawal from participation in the study the sample size was inflated to include a total of 108 participants.
2.4. Sampling Technique
All HHH in Mirpur to Mohakhali and Gabtoli to Mohakhali route who had worked in the current position for at least 6 months were initially invited to attend at a temporary office at Mirpur, Dhaka. The purpose of the study, the procedures involved and the requisites to be participant of the study was explained to them and their consent to participate was sought. It can be noted that from all available helpers, as per inclusion and exclusion criteria, only those respondents who provided consent to participate in the study were considered eligible. A list was prepared for 180 eligible helpers who provided consent to participate in the study. From the list 108 HHHs was selected by simple random sampling (SRS). Although 7 participants did not wish to participate in the study after SRS, therefore, we had randomly chosen the next participants through SRS.
2.5. Data Collection Tools
A structured questionnaire and a check list were used as research instrument. The checklist was used for recording findings of clinical and spirometric examination. Respiratory questionnaire was adapted from American Thoracic Society [25] . Anthropometries of the HHH were performed by standard weight and height scale using WHO guideline [26] . The questionnaire was pre tested, evaluated & revised before data collection. All selected HHHs were interviewed using the structured questionnaire to elicit socio-demographic, occupational and respiratory problem related information.
2.6. Spirometry
Spirometry is a medical screening test that measures various aspects of breathing and lung function. It is performed by using a spirometer, a special device that registers the amount of air a subject inhales or exhales and the rate at which the air is moved into or out of the lungs [2] . We performed spirometry using AT-6 Schiller AG Spirometer NR. (Schiller health care Ltd, Switzerland).Three measurements obtained through spirometry are particularly useful: forced vital capacity (FVC), forced expiratory volume at one second (FEV1), and the ratio of the FEV1 to the FVC [27] [28] . Computerized spirometers frequently print out six or more measures of flow or volume. However, for most purposes, the FVC and FEV1 suffice. The FVC is the total volume of air exhaled after a Forced Expiratory Maneuver. The ratio of the FEV1 to the FVC is obtained by dividing the FEV1 by the FVC. A person with a low FVC may have a restrictive disease while a low FEV1/FVC ratio may indicate an obstructive disease [27] [28] . For diagnosis of obstructive, restrictive or combined respiratory impairments reduced values of FVC, FEV1 and FEV1/FVC are the primary criteria set by the National Institute for Health and Clinical Excellence (NICE) [29] .
Spirometry measurements are related to age, gender, height and ethnicity [30] . The American Thoracic Society (ATS) recommend the use of the third National Health and Nutrition Examination Survey (NHANES III) reference developed by National Institute for Occupational Safety and Health (NIOSH) of Centers for Disease Control and Prevention [31] . This data set has been widely used for its generalisability as well as covering both children and older people ranging from 8 years to 80 years. The major limitations are this NHANES III reference only applicable for white, black and Hispanic people and the lack of a single reference across all ages [32] . The reference values calculated for pulmonary functions for Asian Indians living in United States could be more appropriately represent people of Bangladesh where the mean (±sd) predicted values for FVC is 4.68 ± 0.66 L and FEV1 is 3.65 ± 0.63 L for male population [33] .
2.7. Methods of Data Collection
The interview of the respondents was carried out in a temporary office at Mirpur-1 bus stop, Dhaka. On completion of the interview, clinical examination was undertaken and the findings were recorded on the checklist. The interview and clinical examination of the 108 study participants was completed over a period of 6 days. On completion interview and clinical examination the participants were sent to a diagnostic center for spirometric assessment according to the convenience of the study participants. The spirometric assessments of the participants were completed over a period of 10 days. Staff at the diagnostic center conducted the pulmonary function tests using an electronic spirometer. Prior to each test the device was checked and height and weight of the subjects were taken using standard weight and height scale and the readings were recorded in spirometer. After sufficient explanation on the method, the subjects were repeatedly tested, with a short interval, until more than three forced expiratory curves that were reproducible had been obtained. A nose clip was applied to each subject, and subjects were in the seating position during the tests.
2.8. Data Analysis
Collected data was checked, edited and entered in SPSS 11.5 for analysis. Descriptive analysis was performed by using percentages and mean ± standard deviation for categorical and quantitative variables, respectively. Chi-square test was done for univariate relationship between two categorical variables and t-test and analysis of variance (ANOVA) were done for computing differences between continuous variables and exposure categories. Finally binary logistic regression was also carried out to test the association between respiratory problems and its associated factors. Variables those were significant or nearly significant in univariate analyses were considered in the logistic regression model. Statistical significance was defined as p < 0.05.
Written informed consents were obtained from each participant before data collection. This study was performed in partial fulfillment for the requirements of the “Master of Public Health degree” carried out at the National Institute of Preventive and Social Medicine (NIPSOM), Dhaka for the session: 2005-06 and accepted by the faculty of Post Graduate Medical Science and Research, Dhaka University.
3. Results
There were 108 male respondents with mean age of 18.39 ± 3.48 years. Majority of them belonged to 15 - 19 years age group with 7.4% less than 15 years old. The average monthly income was USD 21.25 as per 2005 currency conversion. Half of the respondents were illiterate and nearly half of them had primary level of education. About three-fourth of the respondents had no history of previous employment in any motor vehicle. Their working hours ranged from 12 to 16 hours per day and 38% of them had no weekly holidays (Table 1).
About 75% of the respondents did not reported to have any respiratory problem in the preceding year while 44.4% had current respiratory problems. Among the respondents with current respiratory problems, 68.7% complained of increasing respiratory problems day by day and 33.3% gave history of feeling better on weekly holidays. Regarding different symptoms of current respiratory problems 50% of respondents had nasal irritation, 89.6% had hoarseness of voice, 50.0% had cough when did not catch cold, 25% brought up phlegm when did not catch cold. Moreover, 70.8% of respondents had wheeze, 37.5% complaint of tightness of chest and 25% experienced shortness of breath during hurrying or walking up. Half of them were smokers and 8.3% used mask in the working place (Table 2).
Regarding lung function tests, the mean values of forced vital capacity (FVC), forced expiratory volume in one second (FEV1), percentage of FEV1 (FEV1%) and peak expiratory flow rate (PEFR) were 3.92 ± 0.44 litre, 2.68 ± 0.71 litre, 68.94 ± 17.46 and 6.85 ± 1.09 litre/sec, respectively (Table 3). Spirometry results also showed that 53.7% of respondents had normal pulmonary function, 41.7% had obstructive impairment and only 4.6% had combined feature of pulmonary impairment. No restrictive type pulmonary impairment was observed (Table 4).
Table 1. Socio-economic status information of the study participants.
*Smoker means he who smokes cigarette or any tobacco preparation for the last six months or more
*Respiratory problems means any respondent suffering from nasal irritation and or hoarseness of voice and or cough when the study subject does not catch a cold and or bringing up phlegm when the subject does not catch a cold and or having a wheezy or whistling chest and or dyspnoea.
Table 3. Lung function parameters among the study participants.
aForced vital capacity (FVC): The maximal volume of air which can be exhaled forcefully after maximal inspiration is called forced vital capacity. bForced expiratory volume in one second (FEV1): Vital capacity is timed that means the percentage of vital capacity that is expired in 1st, 2nd and 3rd sec are determined. Normally FEV is 83% - 84% in 1st second, 93% in 2nd second and 97% in 3rd second. The volume of air that is expired at one second is called force expiratory volume at one second (FEV1). cPeak expiratory flow rate (PEFR): PEFR is defined as the maximum flow rate maintained for at least 10 milliseconds during a forced expiration from full inspiration.
Table 4. Distribution of pulmonary status according to spirometric finding.
Obstructive: FEV1 reduced, FVC reduced or normal, and FEV1/FVC reduced; Restrictive: FEV1 reduced or normal, FVC reduced, and FEV1/FVC normal or increased; Combined: FEV1, FVC, and FEV1/FVCall reduced (Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. http://www.goldcopd.org).
Bivariate analyses showed that different lung function parameters like FEV1, FEV1% & PEFR were significantly lower in smokers and respondents with longer duration of employment (p < 0.05) when compared to smokers and shorter durations of employment, respectively. Additionally, pulmonary impairment was more common amongst those having longer duration of employment (p < 0.05) (Table 5 & Table 6).
Finally, after adjusting age, smoking history and different duration of employment, binary logistic regression analysis showed that duration of employment more than 24 months (OR 6.89; 95% CI 3.42, 8.41) and smoking (OR 3.62; 95% CI 1.87, 4.67) were independently associated with respiratory problems of the HHH. Separate logistic regression analyses also observed that smoking was also associated with nasal irritations, hoarseness of voice, cough and bringing up phlegm and duration of employment 12 - 17 months was independently associated with the hoarseness of voice, chest tightness, cough and shortness of breath during hurrying or walking up (Table 7).
4. Discussion
We found that half of selected the transport workers of Dhaka city had altered pulmonary function with majority of them with obstructive variety of pulmonary impairment. The pulmonary impairment was more common among helpers having longer duration of employment.
This is striking that 7.4% of the HHH were less than 15 years old. However, this statistic was in concordance with National Child Labour Survey 2002 conducted by Bangladesh Bureau of Statistics where 12.6% of children aged below 14 years were included in the work force [34] . About three-fourth of the study population had no history of previous employment as a helper. This could probably be attributable to the low mean age (18.39 years) of the respondents. The difference between current and previous years reported respiratory problems was also possibly due to duration of exposure and their age. Among the helpers with current respiratory problems, around 70% of them complained of gradual increase in respiratory problems and one-third of them gave history of feeling better on weekly holidays. It was probable that on weekends the respondents were not exposed to human hauler exhaust and thus felt better.
The HHH presented their current respiratory problems in the form of different combination of symptoms. Exposure to motor exhaust particularly with SPM has been associated with irritation of nasal mucous membrane and other nasal problems [35] [36] . It can also be noted that cough and mucous secretion are coordinated neuronal reflexes that protect the respiratory tract from noxious exogenous substances such as motor exhaust lead to a state of chronic distress with hyper secretion, chronic cough, and shortness of breath [37] .
Table 5. Distribution of lung function parameters according to smoking habit.
Table 6. Distribution of lung function parameters according to duration of employment.
Table 7. Results of regression analyses showing independent predictors of respiratory problems.
Comparison groups: *no smoking; †duration of employment 6 - 11 months.
Spirometry showed that half of the respondents had normal lung function, 42% had obstructive feature and 5% had combined feature of pulmonary impairment, but there were no restrictive impairments. As the restrictive varieties are commonly found in conditions like fibrosis, silicosis, and also in old age groups, absence of restrictive variety for the current study was natural [38] . In individuals who suffer from air flow obstruction, forceful exhalation causes airways to close prematurely because of the increased intra thoracic pressure produced during the procedure. This phenomenon of “air trapping” results from dynamic compression due to increased resistance of intra thoracic airways and loss of elastic recoil. So, FEV1 decreases [38] . Airflow limitation is caused by diseases like asthma, chronic bronchitis, emphysema and also due to exposure to vehicular emissions. But in some cases FEV1 and FVC both reduces, so combined restrictive and obstructive features also co-exists [7] . The current results supported this phenomenon. Impaired pulmonary status was found to be most prevalent amongst those less than 20 years of age (37.5%). However, no association between age and pulmonary status was detected.
Regarding smoking habit, 49.1% helpers were smokers. Most of the parameters including FEV1, PEFR, and over-all pulmonary impairment were found to be significantly lower among the helpers who had the habit of smoking (p < 0.05). Smoking is a well-known factor for obstructive changes by causing irritation of the respiratory mucosa resulting in hypertrophy of mucosal epithelial cells. This cause increased secretion of mucous leading to formation of mucous plugs; these mucous plugs obstruct the outflow of inhaled air resulting in development of obstructive features [39] . Previous studies also observed that smoking implied additional risk of obstructive pulmonary diseases among vulnerable groups like transport workers [40] .
We observed significant reduction of FVC%, FEV1 & PEFR in relation to duration of employment. But no relationship was observed between duration of employment and FVC. It can be mentioned that generally FVC reduced in restrictive type of lung diseases and pulmonary impairment following exposure to motor vehicular exhaust is of obstructive variety [37] . So it was not unlikely that FVC was not reduced among helpers with longer duration of employment.
A recent cross sectional study found that age, sex, smoking habit and socio-economic status are independent risk factors for chronic obstructive pulmonary disorder (COPD) among the Dhaka city dwellers [41] . Although this study was done among general population of all age groups, not among the high risk people like transport workers. The oldest HHH in our study was only 30 years old, most likely therefore, we did not observe any association with age. Finally, taking the regression results into account, it can be assumed that smoking and duration of employment were independently associated with respiratory problems among the HHH. However, the exposure to motor exhaust takes some time (18 - 24 months) to develop respiratory problems among the exposed group.
Limitations
This study had several limitations. As the study was carried out in a selected area of Dhaka city the findings might not be representative for all transport workers. There were no control groups and finally, we could not measure the personal exposure level of vehicular exhaust in this study.
5. Conclusion
This study provides new information on respiratory health of a specific cadre of transport workers in Dhaka city. A further study covering human hauler helpers and other transport workers of different cities of the country needs to be undertaken for validating the findings of this study. Moreover, awareness building programs targeting owners, driver and helpers of transport workers on effect of motor exhaust on respiratory health and risk of development of respiratory problems among smokers needs to be organized.
Acknowledgements
We acknowledge the priceless support given by all who participated in this study, especially the study participants, Modern diagnostic center, Dhaka, Department of Environment (DOE) and AQMP project, DOE, Department of occupational and environmental health, NIPSOM, Dhaka and the core donors of icddr,b.
Funding
This research received no specific grant from any funding agency.
References
- Chauhan, A.J. and Johnston, S.L. (2003) Air Pollution and Infection in Respiratory Illness. British Medical Bulletin, 68, 95-112. http://dx.doi.org/10.1093/bmb/ldg022
- Bartra, J., Mullol, J., del Cuvillo, A., Dávila, I., Ferrer, M., et al. (2007) Air Pollution and Allergens. Journal of Investigational Allergology and Clinical Immunology, 17, 3-8.
- Dhaka Population. World Population Statistics. http://www.worldpopulationstatistics.com/dhaka-population/
- Rehana, A. and Derek, L. (2002) Better Air Quality in Asian and Pacific Rim Cities. Paper Presented at Better Air Quality Workshop 2002 by Air Quality Management Project, Bangladesh; 16-18 December 2002, Wan Chai, Hong Kong.
- Xie, J., Brandon, C.J. and Shaj, J.J. (1998) Fighting Urban Transport Air Pollution for Local and Global Good. Paper Presented at the Consultative Meeting on Integrated Approach to Vehicular Air Pollution Control in Dhaka Held by World Bank and Department of Environment of Bangladesh, 26-27 April 1998.
- Groneberg-Kloft, B., Kraus, T., Van Mark, A., Wagner, U. and Fischer, A. (2006) Analyzing the Causes of Chronic Cough: Relation to Diesel Exhaust, Ozone, Nitrogen Oxides, Sulphur Oxides and Other Environmental Factors. Journal of Occupational Medicine and Toxicology, 1, 6. http://dx.doi.org/10.1186/1745-6673-1-6
- World Health Organization (2006) WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide: Global Update 2005. Summary of Risk Assessment. World Health Organization, Geneva.
- Riechelmann, H., Rettinger, G., Weschta, M., Keck, T. and Deutschle, T. (2003) Effects of Low-Toxicity Particulate Matter on Human Nasal Function. Journal of Occupational & Environmental Medicine, 45, 54-60. http://dx.doi.org/10.1097/00043764-200301000-00013
- World Health Organization (1988) Air Quality Criteria and Guides for Urban Air Pollutants. World Health Organization Technical Report Series, No. 507, Geneva, 5-25.
- Pravati, P., John, R.A., Dutta, T.K., et al. (2010) Pulmonary Function Test in Traffic Police Personnel in Pondicherry. Indian Journal of Physiology and Pharmacology, 54, 329-336.
- Happo, M.S., Salonen, R.O., Halinen, A.I., et al. (2010) Inflammation and Tissue Damage in Mouse Lung by Single and Repeated Dosing of Urban Air Coarse and Fine Particles Collected from Six European Cities. Inhalation Toxicology, 22, 402-412. http://dx.doi.org/10.3109/08958370903527908
- Budinger, G.R., Mc Kell, J., Urich. D., et al. (2011) Particulate Matter-Induced Lung Inflammation Increases Systemic Levels of PAI-1 and Activates Coagulation through Distinct Mechanisms. PLoS ONE, 6, e18525.http://dx.doi.org/10.1371/journal.pone.0018525
- Ekpenyong, C.E., Ettebong, E.O., Akpan, E.E., Samson, T.K. and Daniel, N.E. (2012) Urban City Transportation Mode and Respiratory Health Effect of Air Pollution: A Cross-Sectional Study among Transit and Non-Transit Workers in Nigeria. BMJ Open, 2, e001253. http://dx.doi.org/10.1136/bmjopen-2012-001253
- Foster, W.M., Brown, R.H., Macri, K., et al. (2000) Bronchial Reactivity of Health Subjects: 18-20h Post-Exposure to Ozone. Journal of Applied Physiology, 89, 1804-1810.
- Wong, C.M., Thach, T.Q., Chau, P.Y., et al. (2010) Part 4: Interaction between Air Pollution and Respiratory Viruses: Time-Series Study of Daily Mortality and Hospital Admissions in Hong Kong. Research Report (Health Effects Institute), 154, 283-362.
- Chai, Z.F., Qian, Q.F., Feng, X.Q., et al. (2004) Study of Occupational Health Impact of Atmospheric Pollution on Exposed Workers at an Iron and Steel Complex by Using Neutron Activation Analysis of Scalp Hair. Journal of Radioanalytical and Nuclear Chemistry, 259, 153-156. http://dx.doi.org/10.1023/B:JRNC.0000015821.47501.bd
- Nku, C.O., Peters, E.J., Eshiet, A.I., et al. (2005) Lung Function, Oxygen Saturation and Symptoms among Street Sweepers in Calabar-Nigeria. Nigerian Journal of Physiological Sciences, 20, 79-84.
- Kennedy, S.M., Chambers, R., Du, W., et al. (2007) Environmental and Occupational Exposure: Do They Affect Chronic Obstructive Pulmonary Disease Differently in Women and Men? Proceedings of the American Thoracic Society, 4, 692-694. http://dx.doi.org/10.1513/pats.200707-094SD
- Bangladesh Road Transport Authority(2013) URL:http://www.brta.gov.bd/.
- Motor Vehicles Ordinance, 1983 (Government of the People’s Republic of Bangladesh), s. 76A(1)(b)-(c).
- The World Bank (2007) Improving Living Conditions for the Urban Poor Bangladesh Development Series. Paper No. 17, The World Bank Office, Dhaka.
- Wadud, Z. and Khan, T. (2013) Air Quality and Climate Impacts Due to CNG Conversion of Motor Vehicles in Dhaka, Bangladesh. Environmental Science Technology, 47, 13907-13916. http://dx.doi.org/10.1021/es402338b
- Begum, B.A., Biswas, S.K. and Hopke, P.K. (2006) Impact of Banning of Two-Stroke Engines on Airborne Particulate Matter Concentrations in Dhaka, Bangladesh. Journal of the Air Waste Management Association, 56, 85-89. http://dx.doi.org/10.1080/10473289.2006.10464430
- Hussam, A., Alauddin, M., Khan, A.H., Chowdhury, D., Bibi, H., Bhattacharjee, M. and Sultana, S. (2002) Solid Phase Microextraction: Measurement of Volatile Organic Compounds (VOCs) in Dhaka City Air Pollution. Journal of Environmental Science and Health. Part A, Toxic/Hazardous Substances & Environmental Engineering, 37, 1223-1239.
- American Thoracic Society (1978) Recommended Respiratory Disease Questionnaires for Use with Adults and Children in Epidemiological Research. http://www-archive.thoracic.org/sections/publications/statements/pages/archive/rrdquacer.html
- WHO (1995) Physical Status: The Use and Interpretation of Anthropometry: Report of a WHO Expert Committee. World Health Organization, Geneva.
- NIOSH (2003) Spirometry Training Guide. Division of Respiratory Disease Studies. The National Institute for Occupational Safety and Health, West Virginia.
- Crapo, R.O., Morris, A.H., Clayton, P.D., et al. (1982) Lung Volumes in Health Non-Smoking Adults. Bulletin Européen de Physiopathologie Respiratoire, 18, 419-425.
- The National Collaborating Centre for Chronic Conditions (2004) Chronic Obstructive Pulmonary Disease. National Clinical Guideline on Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care. Thorax, 59, 1-232.
- Stanojevic, S., Wade, A. and Stock, J. (2010) Reference Values for Lung Function: Past, Present and Future. European Respiratory Journal, 36, 12-19. http://dx.doi.org/10.1183/09031936.00143209
- Hankinson, J.L., Odencrantz, J.R. and Fedan, K.B. (1999) Spirometric Reference Values from a Sample of the General US Population. American Journal of Respiratory and Critical Care Medicine, 159, 179-187. http://dx.doi.org/10.1164/ajrccm.159.1.9712108
- Miller, M.R., Hankinson, J., Brusaco, V., Burgos, F., Casburi, R., Coates, A., et al. (2005) Standardisation of Spirometry. European Respiratory Journal, 26, 319-338. http://dx.doi.org/10.1183/09031936.05.00034805
- Ashok, F.A., Copur, A.S., Javeri, A., Jere, S. and Cohen, M.E. (2004) Reference Values for Pulmonary Function in Asian Indians Living in the United States. Chest, 126, 1225-1233. http://dx.doi.org/10.1378/chest.126.4.1225
- Bangladesh Bureau of Statistics (2002) National Child Labour Survey.
- World Health Organization (1996) Diesel Fuel and Exhaust Emissions: Environmental Health Criteria 171. WHO, Geneva.
- Riechelmann, H., Rettinger, G., Weschta, M., Keck, T. and Deutschle, T. (2003) Effects of Low-Toxicity Particulate Matter on Human Nasal Function. Journal of Occupational & Environmental Medicine, 45, 54-60. http://dx.doi.org/10.1097/00043764-200301000-00013
- Saldiva, P.H.N., Pope 3rd, C.A., Schwartz, J., Dockery, D.W., Lichtenfels, A.J., Salge, J.M., et al. (1995) Air Pollution and Mortality in Elderly People: A Time-Series Study in Sao Paulo, Brazil. Archives of Environmental Health, 50, 159-163. http://dx.doi.org/10.1080/00039896.1995.9940893
- William, N.R. (1998) Environmental and Occupational Medicine. 3rd Edition, Lippincott-Raven, New York, 245, 247-252, 261-262.
- Waldron, H.A. (1994) Occupational Health Practice. 3rd Edition, Butterworths, London, 217-233.
- Mannino, D.M. and Buist, A.S. (2007) Global Burden of COPD Risk Factors, Prevalence and Future Trend. The Lancet, 370, 765-773. http://dx.doi.org/10.1016/S0140-6736(07)61380-4
- Islam, M.S., Hossain, M.M., Pasha, M.M., Azad, A.K. and Murshed, K.M. (2013) Prevalence and Risk Factors of Chronic Obstructive Pulmonary Disease (COPD) in Dhaka City Population. Mymensingh Medical Journal, 22, 547-551.
NOTES

*Corresponding author.


