Health
Vol. 4 No. 6 (2012) , Article ID: 19713 , 8 pages DOI:10.4236/health.2012.46056
Educational interventions aimed at improving the oral health conditions of workers: A critical review
![]()
Faculty of Denstrity, Federal University of Bahia, Salvador, Brazil; *Corresponding Author: luisacte@yahoo.com.br
Received 26 March 2012; revised 17 April 2012; accepted 30 April 2012
Keywords: Occupational Health; Oral Health; Dental Health Education
ABSTRACT
The aim of this research was to identify studies describing the educational and/or health-promoting interventions and strategies used in various programs of oral healthcare conducted in populations of industrial workers. A review of the Science, MEDLINE, LILACS and SCIELO databases was performed for the period between 1980 and 2009. The criteria for a publication to be included were: 1) the population had to consist of adult workers; and 2) the educational and/or health-promoting interventions had to have been described. A great variety of educational strategies was found, ranging from individual counseling to small-group discussions and instructions on oral hygiene with supervised tooth brushing. The presence of plaque and gingivitis were the most commonly used indicators of the effect of these interventions. Cost evaluation was also an important topic. In general, the indicators analyzed reflected positive results that included a reduction in the indicators themselves (plaque and gingivitis) and in the cost of the programs, suggesting a certain effect of the educational programs developed. Nevertheless, differences in forms of exposure according to the type of occupation are not discussed and neither are specific social determinants such as income and education level. The quality of the studies is limited, which reduces the robustness of the evidence on the effect of educational programs on the work population. Studies should be carried out using mixed approaches to evaluate the efficacy of these programs and propose improvements.
1. INTRODUCTION
Studies have shown the poor efficacy of the hegemonic model of restorative surgery in oral healthcare. This is a healthcare model that involves high costs, poor results and a minimal epidemiological impact. Nevertheless, it is the model practiced by a large percentage of dentists in both the public and private sectors [1].
The consequences of the practice of this dental care model in the adult population are that in the majority of cases the treatment offered is confined to managing damage that has already been done, whereas no significant effect is found on the patient’s oral health condition [2,3].
This model has contributed to the current state of oral health found in the workers investigated in some studies, with concordant results of similar mean DMFT (decayed missing filled teeth) values and an increase in the missing component as the age of the individual increases. Furthermore, the percentages of individuals using or needing to use a prosthesis are significant and remain similar throughout all the studies, as are the percentages of periodontal abnormalities [4-7].
Another factor that aggravates the oral health status of workers is the difficulty they experience in obtaining dental care, since going for treatment requires authorization from their employer. On the other hand, oral health conditions may vary in accordance with the job performed by the worker within the organization. In an attempt to avoid taking time off work, those further down the hierarchical ladder may put off going to the dentist for as long as possible, thus resulting in more severe damage to their dental health.
Furthermore, adult workers are exposed both to the risks commonly associated with oral health problems and to hazards present in the work environment. The association between these risk factors and the occurrence of oral alterations has already been identified in some specific areas such as the food and drink industry [8-10] and the chemical products industry [4,11-13].
With the objective of improving oral health conditions and reducing absenteeism, some companies have implemented dental healthcare services. Motta and Toledo [14] and Ahlberg et al. [1,15,16] evaluated dental programs developed in companies and reported similar findings of a reduction in illness due to oral problems and stabilization of the need for surgical restorative work, with a reduction in situations of urgency and absenteeism due to dental problems.
However, structural weaknesses were found in these programs, since their development is still based on the hegemonic restorative surgery model, with priority given to the treatment of problems/damage that already exist. With this in mind, some studies have emphasized the importance of implementing systematic, continuous actions of promotion and education [17] in dental care with the objective of changing habits and behavior and encouraging workers to adopt healthier lifestyles that would lead to an improvement in oral health indicators [18-20].
Changing the habits and behavior of individuals is known to be a difficult task and to do so requires healthcare professionals with skills and abilities in the use of strategies capable of sensitizing subjects to the construction of shared knowledge, despite recognizing the limitations of implementing these educational practices. Kay and Locker [17] conducted a systematic review and reported that educational initiatives may result in improvements in oral health-related knowledge and objective measures of oral health status such as a reduction in plaque of around 37%. However, these actions are less effective in achieving changes in attitudes over the long term.
Occupational oral healthcare programs, linked to programs of general health and occupational safety and embedded within these programs, could focus on educational, preventive and healthcare proposals to implement actions within the work environment according to the epidemiological profile of the specific group within the company and the type of exposure to which they are submitted [14,19]. They should also use individual and community educational tools that would reduce risks and damage by empowering workers [20]. Few studies have been conducted to analyze programs of occupational dental care that focus particularly on the development of educational initiatives to improve oral health conditions in workers.
Therefore, the objective of the present study was to identify the interventions and strategies used in various programs of occupational dental healthcare, thus providing additional information for healthcare professionals in the development of initiatives of this kind.
2. METHODOLOGY
This study was conducted by performing a search of the Web of Science, MEDLINE, LILACS and SCIELO databases for the period ranging from 1980 to 2009 using the following key-words in English: occupational health; oral health; and dental health education.
A publication was only included in the present review if it fulfilled the following criteria: 1) the study population consisted of adult workers; and 2) the educational and/or health-promoting interventions carried out during the study were described. Based on this search procedure, 17 potentially eligible articles were identified for the study. Following analysis of the titles and abstracts of the articles, those that appeared to fulfill the inclusion criteria were selected and these papers were read in their entirety, after which a final definition was made regarding which papers were to be included in the study. After reading these papers, only five were found to comply with the criteria established for inclusion in this review.
3. RESULTS
Two of the studies selected for inclusion were conducted in Denmark, while the remaining three were carried out in Japan. Two of the papers referred to quasiexperimental studies [21,22], while one was an experimental study with no control group [23] and the remaining two were experimental studies conducted with control groups [24,25]. The number of participants in these studies differed greatly, ranging from a minimum of 68 to a maximum of 1998 workers (Table 1). Women formed the majority of the sample population in only one of the studies [23], with a higher proportion of men to women in all the others.
The present findings showed that there was a great variety in the type of educational strategies implemented, ranging from individual counseling to the formation of small groups and guidance on oral hygiene within the work environment. Contrary to the studies conducted in Japan, emphasis in the Danish studies was predominantly on group strategies. In two of the studies analyzed, individual reports on oral health status were provided as part of the activities conducted.
Significant differences were found between the period during which the programs were carried out and the duration of the studies. However, in the studies conducted by Morishita et al. [21] and Peterson et al. [24] these variables were identical. It is important to emphasize that in the studies in which duration was longer, cost evaluation was performed [22,25].
With respect to the indicators of effect used in the studies, similarities were found between the studies conducted by Peterson et al. [23] and Schou et al. [24], in which the same factors such as the presence of plaque and gingivitis were evaluated, albeit using different indexes. Nevertheless, it is reasonable to conclude that the reduction in plaque in the intervention group ranged from 20% to 64.6%, whereas gingivitis decreased by a factor that varied from 47.1% to 69.5%. This reveals a significant heterogeneity of effects, which may indicate different contexts in the implementation of these programs.
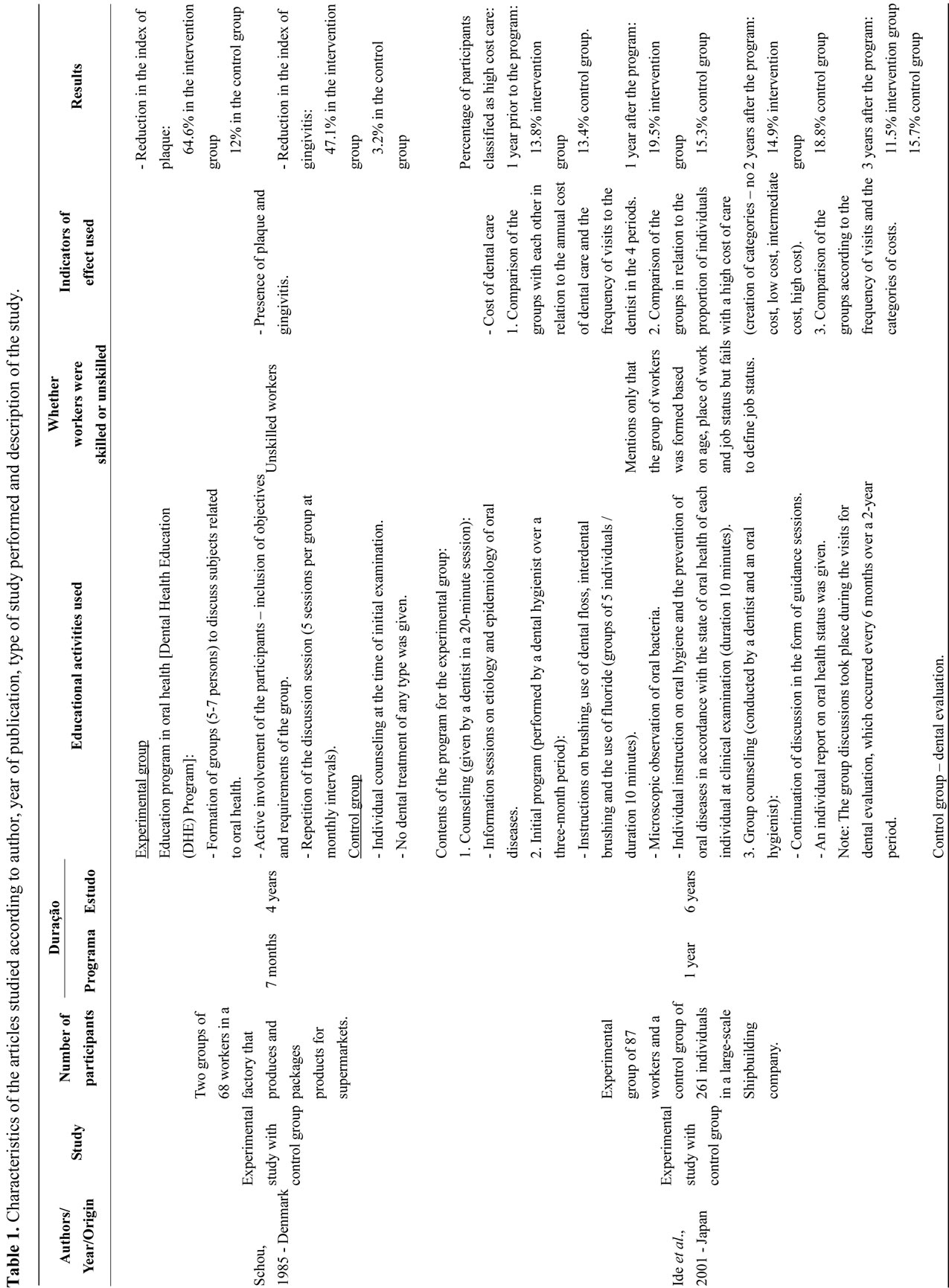
Morishita et al. [21] and Peterson et al. [23] evaluated dental conditions; however, the former group evaluated the tooth itself, whereas the other group of investigators evaluated the surfaces of the tooth. Despite these differences, results from these studies are in agreement with respect to the periodontal and dental conditions found. Ichihashi et al. [22] and Ide et al., [25] who focused on the field of health economics, did not use the same indicators of effect, since their studies evaluated different costs (the cost of dental care alone or cost-benefits, respectively).
The study conducted by Shou [24] showed a significant reduction in the indicators analyzed, principally when compared to the control group. Similar results were also found in the studies carried out by Morishita et al. [21] and Peterson et al. [23]; however, since there was no control group, it was impossible to make inter-group comparisons. Of the two papers in which cost analysis was performed, one reported a reduction in dental carerelated costs during the study follow-up [25], while the other reported greater cost-benefits when a mean of 2 - 4 visits was made to the dentist [22].
Only the study conducted by Petersen et al. [23] took the dangers of the work environment into consideration in defining educational topics and strategies, and included the participation of safety committees in formulating educational and preventive programs and evaluating exposure to sugar dust and the development of dental problems.
4. DISCUSSION
The results of this study show that educational interventions among individuals in the workplace led to a reduction in plaque that ranged from 20% to 64.6% and a reduction in gingivitis that ranged from 47.1% to 69.5%. The study also revealed the large heterogeneity of effects, which may indicate different contexts in the implementation of these programs.
This review found few papers in which educational programs for workers were described or evaluated. This may be associated with a lack of programs of this nature aimed at this segment of the population.
The scarcity of programs aimed at implementing educational interventions in the work environment may be associated with difficulties in putting the planned activities into practice. This may occur as a result of demands imposed by the employer related to not wanting to lose production time, which could have a detrimental effect on the company’s productivity, or as a consequence of the difficulties encountered by the healthcare teams themselves in implementing the programs.
The predominance of men in the studies may be justified by the greater insertion of men in the industrial sector since many activities require physical strength or involve manual labor. The only study in which there was a higher proportion of women compared to men was conducted in two chocolate factories in which the type of activity explains the predominance of women [23].
The publications selected resulted from studies conducted in two countries (Denmark and Japan), possibly as a consequence of the greater value attributed to the development of educational programs within the work environment in these countries. Another relevant subject for debate is the greater economic and social development in these countries, which may have an effect on their endeavors to reduce health-related costs through educational initiatives within the work environment or indeed on the development of this field of study.
In view of the need to reduce these expenses, cost analysis studies are being developed [26-28], which are vital in the area of occupational oral healthcare, since they provide data on the effect of these programs and sensitize employers regarding the need to implement educational programs aimed at preventing oral health damage that is severe but not life-threatening.
With respect to educational activities, three of the studies involved group actions as well as individual actions. Collective activities allow the construction of shared knowledge, taking into consideration the degree of enlightenment, culture and values of the participants, thus potentiating the actions developed and increasing their effect. Furthermore, studies show that the individual must be actively involved for educational actions to successfully contribute towards changing habits and behaviors. The World Health Organization’s Ottawa Charter for Health Promotion stresses the importance of empowerment, which consists of enabling individuals and groups to act in improving their own quality of life and health, and emphasizes greater community participation in the process [29]. Thus, educational programs should consist of participative educational actions that include the active involvement of subjects and that meet the requirements and expectations of the groups involved. Taking these questions into consideration, the study conducted by Petersen et al. [23] made progress by involving the subjects, seeking to empower the individual and forming multipliers within the company itself, which probably strengthened the educational actions.
Another relevant question deals with the social aspects that may either protect health or provoke disease and that should be encompassed within a multiplicity of determinants, particularly social determinants of health such as education level, income, type of occupation (skilled or unskilled) and the position the individual holds within the hierarchy of the company. Despite the relevance of these aspects, no discussion was found in any of the papers evaluated on the social determinants of health, with these questions being mentioned only superficially. Schou [24] simply described the criteria used in the selection of the workers (unskilled, paired according to gender, age and socioeconomic status). The study conducted by Ide et al. [25] mentions having selected workers based on their age, place of work and job status, but fails to define job status. In the discussion, the authors state that the use of healthcare services is related to age, gender, income, education and geographical region of the country.
Since the objective of these studies was to evaluate occupational oral health, programs would be expected to consider questions related to the risks present in the work environment and the occurrence of oral problems. However, only one study evaluated this association and included the participation of safety committees to define topics to be discussed with the workers, reflecting integration between oral health and occupational safety [23].
5. CONCLUSIONS
The results of this study reflect the limited advances that have been made in the field of occupational health and, as part of this field, in dentistry within the work environment, although the relevance of taking occupational issues into consideration in healthcare programs is recognized. Another relevant question to be discussed is the implementation of these programs in companies, which is related to the degree to which the planned proposal was accomplished. In the case of the papers selected for inclusion in the present study, the variation in the implementation of the programs, understood here as the successful implementation of an intervention, may have affected the results. The difficulties in developing occupational healthcare actions are already known and may have contributed to the fact that the programs achieved poorer levels of implementation, hence less favorable results. In other words, even though the programs obtained significant results, these results could have been better if implementation had been more successful [29].
This study also shows that the subjects involved in the programs (the company, the workers and the oral healthcare team) contribute independently towards implementing the interventions. This can be seen in the study conducted by Petersen et al. [23] that counted on the active participation of the safety committee, which may have contributed positively towards implementation of the program. Furthermore, knowledge by the subjects of the actual objectives of the program renders better results [30].
The principal limitation of the present study lies in the difficulty in selecting studies in which priority was given to the educational component, since this is normally a component of larger healthcare programs, which limited the scope of analysis.
This study also found little evidence of the effect of educational programs on the working population. These findings suggest that further studies should be conducted using mixed approaches, i.e. both quantitative and qualitative methodology to evaluate the efficacy of these programs and propose improvements.
![]()
![]()
REFERENCES
- Ahlberg, J., Tuominen, R. and Murtomaa, H. (1997) A 5-year retrospective analysis of employer-provided dental care for Finnish male industrial workers. Community Dentistry and Oral Epidemiology, 25, 419-422. doi:10.1111/j.1600-0528.1997.tb01732.x
- Lacerda, J.T., Simionato, E.M., Peres, K.G., et al. (2004) Dental pain as reason for visiting a dentist in a Brazilian adult population. Revista de Saúde Pública, 38, 453-458. doi:10.1590/S0034-89102004000300017
- Silva, D.D., Sousa Mda, L. and Wada, R.S. (2004) Oral health in adults and the elderly in Rio Claro, São Paulo, Brazil. Cadernos de Saúde Pública, 20, 626-631. doi:10.1590/S0102-311X2004000200033
- Petersen, P.E. and Gormsen, C. (1991) Oral conditions among German battery factory workers. Community Dentistry and Oral Epidemiology, 19, 104-106. doi:10.1111/j.1600-0528.1991.tb00121.x
- Petersen, P.E. and Tanase, M. (1997) Oral health status of an industrial population in Romania. International Dental Journal, 47, 194-198. doi:10.1111/j.1875-595X.1997.tb00449.x
- Tomita, N.E., Chinellato, L.E. and Lauris, J.R. (2005) Oral health of building construction workers: An epidemiological approach. Journal of Applied Oral Science, 13, 24- 27. doi:10.1590/S1678-77572005000100006
- Pinto, V.G. and Lima, M.O.P. (2006) Estudo epidemiológico de saúde bucal em trabalhadores da indústria: Brasil 2002-2003. http://bvsms.saude.gov.br/bvs/publicacoes/Estudo_Saude_Bucal_completo.pdf
- Petersen, P.E. (1983) Dental health among workers at a Danish chocolate factory. Community Dentistry and Oral Epidemiology, 11, 337-341. doi:10.1111/j.1600-0528.1983.tb01388.x
- Masalin, K., Murtomaa, H. and Meurman, J.H. (1990) Oral health of workers in the modern Finnish confectionery industry. Community Dentistry and Oral Epidemiology, 18, 126-130. doi:10.1111/j.1600-0528.1990.tb00036.x
- Masalin, K.E., Murtomaa, H.T. and Sipilä, K.P. (1994) Dental caries risk in relation to dietary habits and dental services in two industrial populations. Journal of Public Health Dentistry, 54, 160-166. doi:10.1111/j.1752-7325.1994.tb01208.x
- Amin, W.M., Al-Omoush, S.A. and Hattab, F.N. (2001) Oral health status of workers exposed to acid fumes in phosphate and battery industries in Jordan. International Dental Journal, 51, 169-174. doi:10.1002/j.1875-595X.2001.tb00835.x
- Vianna, M.I., Santana, V.S. and Loomis, D. (2004) Occupational exposures to acid mists and gases and ulcerative lesions of the oral mucosa. American Journal of Industrial Medicine, 45, 238-245. doi:10.1002/ajim.10343
- Almeida, T.F., Vianna, M.I., Santana, V.S., et al. (2008) Occupational exposure to acid mists and periodontal attachment loss. Cadernos de Saúde Pública, 24, 495-502. doi:10.1590/S0102-311X2008000300003
- Motta, R. and Toledo, V.L. (1984) Avaliação de resultados de plano odontológico implantado em indústria mecânica. Revista Brasileira de Saúde Ocupacional, 46, 64-71.
- Ahlberg, J., Tuominen, R. and Murtomaa, H. (1996) Subsidized dental care improves caries status in male industrial workers. Community Dentistry and Oral Epidemiology, 24, 249-252. doi:10.1111/j.1600-0528.1996.tb00854.x
- Ahlberg, J., Tuominen, R. and Murtomaa, H. (1996) Oral mucosal changes and associated factors among male industrial workers with or without access to subsidized dental care. Acta Odontologica Scandinavica, 54, 217- 222. doi:10.3109/00016359609003527
- Kay, E.J. and Locker, D. (1996) Is dental health education effective? A systematic review of current evidence. Community Dentistry and Oral Epidemiology, 24, 231-235. doi:10.1111/j.1600-0528.1996.tb00850.x
- Schou, L. (1985) Active-involvement principle in dental health education. Community Dentistry and Oral Epidemiology, 13, 128-132. doi:10.1111/j.1600-0528.1985.tb00426.x
- Cangussu, M.C.T., Magnavita, R. and Rocha, M.C.B.S. (2001) Educação e construção da cidadania em um programa de saúde bucal em Salvador—BA. Brazilian Association for Preventive Dentistry, 4, 15-20.
- Alves, V.S. (2005) Um modelo de educação em saúde para o Programa Saúde da Família: Pela integralidade da atenção e reorientação do modelo assistencial. Interface—Comunicação, Saúde, Educação, 9, 39-52. doi:10.1590/S1414-32832005000100004
- Morishita, M., Sakemi, M., Tsutsumi, M., et al. (2003) Effectiveness of an oral health promotion programme at the workplace. Journal of Oral Rehabilitation, 30, 414- 417. doi:10.1046/j.1365-2842.2003.01047.x
- Ichihashi, T., Muto, T. and Shibuya, K. (2007) Costbenefit analysis of a worksite oral-health promotion program. Industrial Health, 45, 32-36. doi:10.2486/indhealth.45.32
- Petersen, P.E. (1989) Evaluation of a dental preventive program for Danish chocolate workers. Community Dentistry and Oral Epidemiology, 17, 53-59. doi:10.1111/j.1600-0528.1989.tb00587.x
- Schou, L. (1989) Oral health promotion at worksites. International Dental Journal, 39, 122-128.
- Ide, R., Mizoue, T., Tsukiyama, Y., et al. (2001) Evaluation of oral health promotion in the workplace: The effects on dental care costs and frequency of dental visits. Community Dentistry and Oral Epidemiology, 29, 213- 219. doi:10.1034/j.1600-0528.2001.290307.x
- Silva, L.K. (2003) Technology assessment and cost-effectiveness analysis in health care: The adoption of technologies and the development of clinical guidelines for the Brazilian national system. Ciência & Saúde Coletiva, 8, 501-520. doi:10.1590/S1413-81232003000200014
- Sancho, L.G. and Dain, S. (2008) Cost-effectiveness analysis of renal replacement therapies: How should we design research on these interventions in Brazil? Cadernos de Saúde Pública, 24, 1279-1290. doi:10.1590/S0102-311X2008000600009
- Leal, R.M. and Matos, J.B.B. (2009) Health insurance plans: An analysis of care costs and their components. Revista de Administração de Empresas, 49, 447-458.
- Chaves, S.C.L., Santana, V.S., De Leão, I.C., et al. (2009) Determinants in an occupational health and safety program implementation. Revista Panamericana de Salud Pública, 25, 204-212. doi:10.1590/S1020-49892009000300003
- Organización Mundial de la Salud (1996) Carta de Ottawa para la promoción de la salud. OPAS, Washington, 367-372.

