Open Journal of Urology
Vol. 2 No. 2 (2012) , Article ID: 19130 , 2 pages DOI:10.4236/oju.2012.22015
Thrombocytosis Accompanying Renal Abscess: A Case Report and Review of the Literature
1Department of Urology, Alanya Research and Practice Center, Başkent University, Ankara, Turkey
2Department of Cardiology, Alanya Research and Practice Center, Başkent University, Ankara, Turkey
Email: drburakhoscan@yahoo.com
Received March 8, 2012; revised March 22, 2012; accepted April 5, 2012
Keywords: Renal Abscess; Thrombocytosis; Urinary Tract Infection
ABSTRACT
Reactive thrombocytosis can be seen in patients with various kinds of infections, including upper urinary tract infection. Thrombocytosis in patients with upper urinary tract infection is a response of the bone marrow to the infection and is therefore classified as secondary thrombocytosis. We report a case of thrombocytosis accompanying renal abscess. In this case report, we present that thrombocytosis in a patient with upper urinary tract infection is not a random condition and is associated with renal abscess which is a complication of disease.
1. Introduction
Thrombocytosis in patients with upper urinary tract infection is a response of the bone marrow to the infection and is therefore classified as secondary thrombocytosis [1]. Bleeding, malignancy, and chronic inflammation and also other types of infections are known to be associated with secondary thrombocytosis [2]. In a recent study, it was reported that thrombocytosis accompanying urinary tract may be a marker for urinary obstruction or abscess [3]. Complete blood count is generally ordered in most of the patients with urinary tract infection and information about the patient’s platelet count is made available without extra cost. The evidence of thrombocytosis in a patient with urinary tract infection is rather unexpected and generally ignored. Because some patients with upper urinary tract infection develop thrombocytosis, but most patients do not, Gofrit et al. suggested that thrombocytosis in a patient with upper urinary tract infection has a clinical significance and the platelet count may be used as a marker for complications in patients with urinary tract infection [3]. We report a case in which thrombocytosis is a marker of renal abscess.
2. Case Report
A 20-years old female patient admitted to our Urology Department from Emergency unit with right flank pain. In medical history of the patient, it was noted that treatment with antibiotics (ciprofloxacin 500 mg tablet twice a day) given at another hospital for urinary tract infection ten days before. The patient told that symptoms such as fever and dysuria improved with treatment but right flank pain continued. In physical examination there was right costovertebral tenderness. In complete blood count, number of leukocytes was 11.3 × 109/l, haemoglobin level was 11.2 g/dl and number of thrombocytes was 844 × 109/l. In urinary analysis, there were 11 leukocytes and 1 erythrocyte per high power field. When the complete blood count repeated, number of thrombocytes was 826 × 109/l. Ultrasonography of urinary system was normal. In computed tomography, findings consistent with right pyelonephritis and accompanying perirenal and pararenal abscess observed.
Patient hospitalized and treatment with cephtriaxone 1 g i.v. twice a day and paracetamol tablet 3 × 1/po started. Urine culture remained sterile. This was probably related to antibiotics given before. All symptoms improved with treatment and patient discharged from hospital after 3 days. After 10 days, number of leukocytes was 6.82 × 109/l, haemoglobin level was 11.6 g/dl and number of thrombocytes was 355 × 109/l in complete blood count. In computed tomography performed at that time, there was moderate to marked improvement according to previous tomographic findings. The laboratory and computed tomographic findings of the patient before and after treatment are summarized in Table 1. The computed tomography repeated after 3 months and the findings were totally normal.
3. Discussion
Thrombocytosis in patients with upper urinary tract infection is classified as secondary thrombocytosis [1].
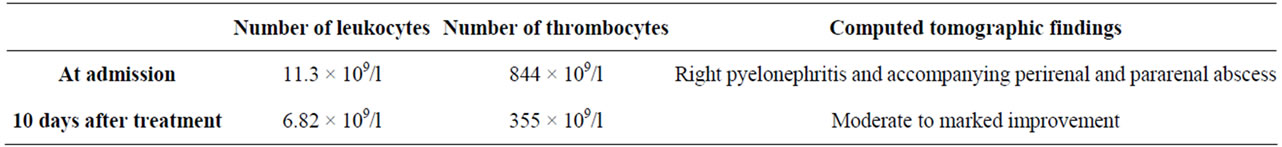
Table 1. The laboratory and computed tomographic findings of the patient before and after treatment.
Secondary thrombocytosis is related to cytokine production during bleeding, infection, malignancy, and chronic inflammation. Acute infections are commonly not associated with thrombocytosis. Production of thrombocytes is inhibited during acute infection by mediators such as bacterial lipopolysaccharide, tumor necrosis factor α, and transforming growth factor β [4]. Thrombocytosis is observed generally several days after the onset of the clinical disease, in particular when the infection has become subacute [3]. In children with urinary tract infection, thrombocytosis typically occurs on days 9 and 14 after disease onset [5]. The peak of infection-associated thrombocytosis in adults is generally 10 days after the clinical onset [6].
At a recent study, it is shown that thrombocytosis is a sign of an infection that failed to clear out and was complicated by obstruction or abscess [3]. In that study, the sensitivity of thrombocytosis for detection of kidney obstruction or abscess in patients with upper urinary tract infection was 76%, the specificity was 77%, and the positive and negative predictive values were 71% and 82%, respectively [3]. In another study by same group, it was reported that postoperative thrombocytosis may be a marker for complications after urologic surgery [7].
In this case report, it is also reported that thrombocytosis in a patient with upper urinary tract infection is not a random phenomenon and it may be a marker of kidney abscess which is a complication of disease. The finding of thrombocytosis in a patient with upper urinary tract infection should be taken into consideration and alert us to actively search for the complications of disease such as urinary obstruction and renal abscess. Cross-sectional imaging studies (abdominal ultrasonography or computed tomography) should then be performed in such patients.
REFERENCES
- A. I. Schafer, “Thrombocytosis,” New England Journal of Medicine, Vol. 350, No. 12, 2004, pp. 1211-1219. doi:10.1056/NEJMra035363
- M. Griesshammer, M. Bangerter, T. Sauer, R. Wennauer, L. Bergmann and H. Heimpel, “Aetiology and Clinical Significance of Thrombocytosis: Analysis of 732 Patients with an Elevated Platelet Count,” Journal of Internal Medicine, Vol. 245, No. 3, 1999, pp. 295-300. doi:10.1046/j.1365-2796.1999.00452.x
- O. N. Gofrit, A. Shapiro, D. Rund, A. G. Verstandig, E. H. Landau, R. Katz, et al., “Thrombocytosis Accompanying Urinary Tract Infection Suggests Obstruction or Abscess,” American Journal of Emergency Medicine, Vol. 24, No. 1, 2006, pp. 118-121. doi:10.1016/j.ajem.2005.05.007
- M. H. Klinger and W. Jelkmann, “Role of Blood Platelets in Infection and Inflammation,” Journal of Interferon & Cytokine Research, Vol. 22, No. 9, 2002, pp. 913-922. doi:10.1089/10799900260286623
- A. Garoufi, K. Voutsioti, H. Tsapra, T. Karpathios and P. M. Zeis, “Reactive Thrombocytosis in Children with Upper Urinary Tract Infections,” Acta Paediatrica, Vol. 90, No. 4, 2001, pp. 448-449. doi:10.1111/j.1651-2227.2001.tb00448.x
- G. Robbins and D. L. Barnard, “Thrombocytosis and Microthrombocytosis: A Clinical Evaluation of 372 Cases,” Acta Haematologica, Vol. 70, No. 3, 1983, pp. 175-182. doi:10.1159/000206719
- O. N. Gofrit, A. Shapiro, D. Rund, E. H. Landau, R. Katz, O. Z. Shenfeld, et al., “Postoperative Thrombocytosis as a Marker for Complications after Urologic Surgery,” Scandinavian Journal of Urology and Nephrology, Vol. 40, No. 2, 2006, pp. 161-165. doi:10.1080/00365590500498166

