International Journal of Clinical Medicine
Vol.1 No.2(2010), Article ID:3262,3 pages DOI:10.4236/ijcm.2010.12015
Cervical Subcutaneous Emphysema; Sequelae from Occult Perforation of Sigmoid Diverticulum
![]()
Department of Elderly Medicine, Royal Bournemouth Hospital, Bournemouth, UK.
Email: mochoudhury@doctors.org.uk
Received September 1st, 2010; revised September 15th, 2010; accepted September 19th, 2010.
Keywords: Subcutaneous, Emphysema, Perforation, Diverticulum
ABSTRACT
Background: An elderly lady presented with dyspnoea due to congestive cardiac failure. She was subsequently noted to have cervical subcutaneous emphysema. Post mortem identified an occult perforation of a sigmoid diverticulum. Cervical subcutaneous emphysema is a recognised complication of gastrointestinal perforation; however, it is normally associated with upper gastrointestinal pathology, procedure related or sequel of existing disease. Summary: A perforated sigmoid diverticulum is a very rare cause of cervical subcutaneous emphysema. In this patient, signs and symptoms of peritonism were also late in onset and the location of the perforation was not found despite high resolution imaging being used.
1. Case Report
A 76-year-old woman was admitted with dyspnoea and orthopnoea. She felt generally unwell but denied any other specific symptoms. Her medical history consisted of non-insulin-dependent diabetes, osteoporosis, depression, alcohol abuse and a hiatus hernia. Medications included risedronate, gliclazide, metformin, allopurinol, ramipril, quinine sulphate, Adcal-D3 and simvastatin. She was an ex-smoker, lived in a residential home and was mobile with a frame.
On initial examination, she was apyrexial and comfortable whilst at rest. She was tachycardia with a heart rate of 110 beats per minute and a blood pressure of 110/51 mmHg. There was bilateral pitting oedema up to the knees. Pulse oximetry recorded an oxygen saturation of 92% whilst on air and auscultation of the lungs revealed bilateral basal crackles. Her abdomen was soft, non tender and bowel sounds were present and normal. Admission bloods showed mild renal impairment, a mildly elevated alkaline phosphatase, iron-deficiency anaemia and a neutrophilia. An arterial blood sample taken whilst breathing air demonstrated hypoxia with a PaO2 of 8.14 kPa. On the admission chest radiograph, there was a raised left hemidiaphragm but no other abnormalities were noted. A mid-stream urine sample, collected four days prior to admission, had grown an enterococcus species sensitive to trimethoprim. On the basis of the clinical findings and initial investigations, she was commenced on trimethoprim and intravenous furosemide for a urinary tract infection and congestive cardiac failure respectively.
On the second day of admission, she was no longer dyspnoeic and felt better. She continued to do well and, therefore on the fourth day an endoscopy was arranged to investigate the iron-deficiency anaemia. However, this was cancelled as the patient was found to have cervical subcutaneous emphysema (see figure 1). The endoscopist suggested that she might have a perforated viscus and an abdominal film and repeat chest radiograph were requested. The patient continued to feel well and denied

Figure 1. The picture illustrates the extensive cervical and anterior chest wall subcutaneous emphysema.
any chest pain, dysphagia or abdominal discomfort. Apart from constipation there were no other abdominal symptoms or signs. Intravenous cefuroxime and metronidazole were commenced for a presumed perforated viscus.
A contrast CT of the chest (see figure 2) and abdomen demonstrated extensive cervical subcutaneous emphysema, pneumomediastinum, retroperitoneal gas and a small amount of intraperitoneal gas. Diverticular disease in the jejunum, duodenum and sigmoid colon were also noted; however, a perforation site could not be identified.
2. Differential Diagnosis
Despite the lack of symptoms and clinical signs, the differential diagnosis included a spontaneous oesophageal perforation, retroperitoneal diverticular perforation and bronchial disruption.
3. Outcome
Due to the patient's co-morbidities the surgical team felt explorative laparoscopy was not indicated. Interestingly, it was the ninth day of her admission when she first complained of abdominal discomfort; however, examination of her abdomen remained unremarkable.
A non-ionic swallow demonstrated a normal upper gastrointestinal tract without any evidence of perforation. From the fourteenth day onwards, the patient started to deteriorate and now complained of severe dull aching in the left flank. On examination she was pyrexial, tachycardic with a heart rate of 110 beats per minute and her blood pressure was 108/66 mmHg. There was pitting oedema up to the abdomen and the lung bases were dull to percussion.
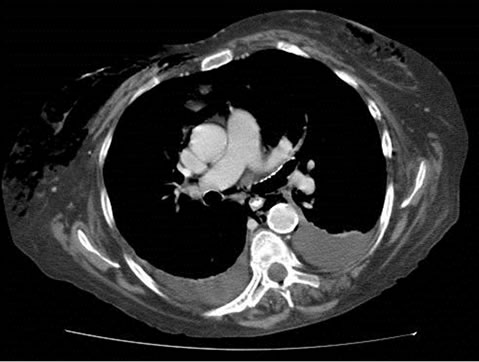
Figure 2. This CT image demonstrates extensive surgical emphysema in the root of the neck extending down into the anterior chest wall. A pneumomediastinum is also apparent.
She was tender in the left iliac fossa but there were no signs of peritonism. The urethral catheter was noted to be draining faeculant matter and its position was confirmed as being correct. The patient deteriorated and died on the eighteenth day of her admission. Subsequent post mortem revealed a perforated diverticulum within the sigmoid colon. Faecal-purulent material was spread widely throughout the peritoneal cavity. Furthermore, she had a bladder fistula, which was in continuity with the perforated bowel. The official cause of death was recorded as intraperitoneal sepsis secondary to a ruptured colonic diverticulum.
4. Discussion and Learning Points
Cervical subcutaneous emphysema is an extremely rare complication of colonic perforation. More commonly it results from bronchopulmonary disruption, gas forming infections and pathology of the upper gastrointestinal tract, such as a perforated gastric ulcer or a ruptured oesophagus. Indeed in our case an oesophageal rupture was considered but was subsequently excluded after a normal non-ionic swallow. The anatomical site of a bowel perforation usually determines the location of any subsequent subcutaneous emphysema. It follows that colonic perforation or colonic surgery usually results in subcutaneous emphysema of the anterior abdominal wall. Colonic and rectal perforations have also been documented to cause subcutaneous emphysema of the scrotum, perineum and upper thighs [1].
Using Medline as a search-engine with English language being the only limiting criteria, there was only seven other case reports of cervical subcutaneous emphysema linked to colonic perforation [2-8]. Of these, three cases were associated with spontaneous rupture of a colonic diverticulum. The other cases were related to perforating sigmoid cancers and colonoscopic perforation.
Our case is especially interesting as the patient had a relative lack of abdominal signs and symptoms despite widespread faecal-purulent material within the peritoneal cavity. Indeed, although the patient was constipated she continued to pass flatus suggesting continued peristalsis.
It has been postulated that continued peristalsis and constipation may contribute to a large pressure gradient between the bowel lumen and retroperitoneum, which forces the gas into the retroperitoneal space and onwards towards the neck [2]. The same forces could drive free gas through the diaphragmatic hiati into the mediastinum and onwards.
Retroperitoneal perforations of the colon are associated with fewer abdominal signs and symptoms than intraperitoneal perforations. However, in our case the abdominal CT demonstrated free gas within the peritoneal cavity as well as retroperitoneum thus indicating retroperitoneal and intraperitoneal perforation. The case was made all the more intriguing as high resolution CT scanning failed to identify the site of perforation.
In conclusion, cervical subcutaneous emphysema of gastrointestinal origin is most likely to occur from oesophageal or peptic ulcer perforation. However, in the absence of symptoms the clinician should also raise the possibility of occult colonic perforation.
REFERENCES
- N. S. Saldua, T. A. Fellars and D. C. Covey, “Case Report: Bowel Perforation Presenting as Subcutaneous Emphysema of the Thigh,” Clinical Orthopaedics and Related Research, Vol. 468, No. 2, February 2010, pp. 619-623.
- I. Hunt, F. Van Gelderen and R. Irwin, “Subcutaneous Emphysema of the Neck and Colonic Perforation,” Emergency Medicine Journal, Vol. 19, No. 5, September 2002, p. 465.
- S. Basu and D. Corless, “Cervical Surgical Emphysema: a Rare Presentation of a Sigmoid Colon Retroperitoneal Diverticular Perforation,” International Journal of Clinical Practice, Vol. 56, No. 3, April 2002, p. 222.
- M. S. Cappel and M. Mark, “Acute Colonic Diverticular Perforation Presenting as a Left Ear Pain and Facial Swelling Due to Cervical Subcutaneous Emphysema in a Patient Administered Corticosteroids,” The American Journal of Gastroenterol, Vol. 87, No. 7, July 1992, pp. 899-902.
- S. D. Fitzgerald, A. Denk, M. Flynn, W. E. Longo and A. M. Venava III, “Pneumopericardium and Subcutaneous Emphysema of the Neck. An Unusual Manifestation of Colonoscopic Perforation,” Surgical Endoscopy, Vol. 6, No. 3, May-June 1992, pp. 141-143.
- M. Krasheninnikoff and B. R. Duus, “Mediastinal and Subcutaneous Cervical Emphysema Caused by a Perforating Sigmoid Cancer,” Acta Chirurgica Scandinavica, Vol. 154, No. 9, September 1988, pp. 541-542.
- G. B. Schmidt, M. W. Bronkhorst, H. H. Hartgrink and L. H. Bouwman, “Subcutaneous cervical emphysema and pneumomediastinum Due to a lower gastrointestinal tract perforation,” World Journal of Gastroenterology, Vol. 14, No. 24, June 2008, pp. 3922-3923.
- T. Hur, Y. Chen, G. H. Shu, J. M. Chang and K. C. Cheng, “Spontaneous cervical subcutaneous and mediastinal emphysema secondary to occult sigmoid diverticulitis,” European Respiratory Journal, Vol. 8, No. 12, December 1995, pp. 2188-2190.

