Open Journal of Organ Transplant Surgery
Vol. 2 No. 4 (2012) , Article ID: 24315 , 4 pages DOI:10.4236/ojots.2012.24013
Laparoendoscopic Single Site Donor Nephrectomy: The Preliminary Experience
Department of Surgery/Renal Transplantation Unit, The Queen Elizabeth Hospital, Woodville, Australia
Email: mohanrao@bigpond.net.au
Received September 25, 2012; revised October 27, 2012; accepted November 6, 2012
Keywords: LESS; Donor Nephrectomy
ABSTRACT
Methods: In our endeavour to give patients visibly scarless surgery we have raised the bar to the next level in laparoscopic donor nephrectomy. We have moved from standard laparoscopy to LESS Laparoendoscopic single site donor nephrectomy. 1997 we introduced laparoscopic donor nephrectomy in Australia. In September 2008 we did our first LESS donor nephrectomy. September 2008 to October 2009, 6 laparoscopic donor nephrectomies were performed using a single port. Two types of devices have been used R-port and SILS™ Port. The device was inserted through an intra umbilical incision using open technique. Surgical technique was similar to the laparoscopic method and standard rigid and roticulator laparoscopic instruments were used. Results: All were completed with no major complications. In 3 an additional 5 mm port was added to reduce the dissection time. Average operating time was 4.4 hours, warm ischemia time was an average of 7.16 minutes and post surgery hospital stay was an average of 1.41 days. All grafts functioned immediately after transplantation. Conclusion: Initial experience with this technique is promising. It is too early to draw any conclusions on its benefits to the donor in terms of reduced morbidity. However the donors appreciated the cosmesis. It is yet another learning curve for the transplant surgeon.
1. Introduction
Laparoscopic donor nephrectomy has now become the Gold standard since its introduction in this country in 1997 [1]. It has decreased the morbidity and the hospital stay. Two hundred and ninety donor nephrectomies have been performed in our unit so far with no major complications, re admissions or re explorations and a 1.5% rate of conversion to open. Modifications to the technique have been made to make it suitable to every donor with the complete elimination of the open donor nephrectomy in our practice. Reducing the number of ports and clustering them has led us to try single port devices.
Currently two new laparoscopic methods—NOTES and Single Port Laparoscopic Surgery are gaining the attention of laparoscopic/endoscopic surgeons. Obviously removing a large organ like the kidney is presently not feasible with NOTES, however it has been delivered through the vagina [2] (after conventional laparoscopic dissection) thus eliminating the delivery incision scar.
Rane and his colleagues performed single port nephrectomy in 2007 [3] and by Raman et al. in the same year [4]. First single port live donor nephrectomy (SPLDN) was done by Gill et al. in 2007 [5] and few teams have been trialling this procedure. Single Port Laparoscopic Surgery and Single Incision Laparoscopic Surgery are being assessed in few select institutions (Cleveland Clinic, Cleveland and Drexel University, Philadelphia) in US. Nomenclature is not standard and different names have been used—Single Port Access (SPA) Surgery, Single Incision Laparoscopic Surgery (SILS), One Port Umbilical Surgery (OPUS), Natural Orifice Trans umbilical Surgery (NOTUS) and Embryonic Natural Orifice Translumenal Endoscopic Surgery E-NOTES) and they vary from each other slightly. At a recent meeting, LESS [6] (Laparoendoscopic Single Site Surgery) has been proposed to include all such procedures. The common objective is to reduce the number of ports and the length of the incisions.
In an effort to further improve the benefits of current laparoscopic method to the donor we have been trialling this procedure at The Queen Elizabeth Hospital in South Australia. This paper describes the surgical technique and clinical outcomes in the first 6 donors who have undergone this procedure at our centre.
2. Methods
The initial lead up to the laparoscopic donor surgery has been described [1]. Under general anaesthesia the donor was placed in a modified right/left lateral decubitus position with the kidney bridge. Patient was secured in position on the operative table with the help of the bean bag to which suction was applied. The single incision port was inserted through the umbilicus by an open Hasson technique. We have used two proprietary, multilumen, single-trocar systems—R-port (Advanced Surgical Concepts, Dublin, Ireland) and SILS™ Port (Covidien, USA). The R-port consists of a fascial retractor containing an inner and an outer ring with an intervening plastic sleeve, and three ports—one 12 mm and two 5 mm ports. SILS port is a flexible port which can be inserted through a single abdominal incision and it accommodates one 12 mm and two 5 mm cannulae. Either device was introduced by Hasson technique through a 3 cm intra umbilical vertical incision which was deepened through the midline facia to gain access to the peritoneal cavity (Figures 1 and 2).
Conventional instruments were used along with roticulator instruments (Roticulator™ Endo Grasp™ 5 mm Covidien); however the Roticulator instruments (Figure 3) were not strong enough to aid in the dissection. SILS port is designed for one 10 - 12 mm and two 5 mm ports but we have been able introduce 15 mm port (for specimen retrieval bag, Endo Catch™ II 15 mm Specimen Pouch Covidien) and place an additional 5 mm port through the gas inlet channel after its removal. We have used the same surgical technique as in our laparoscopic donor nephrectomy [7]. Kidney was placed in the specimen retrieval bag before the renal vessels were divided. The retrieval bag with the kidney was pulled out through the umbilical wound, after the delivery wound was vertically elongated to allow the kidney to slip out in a horizontal angle. The skin incision made is just adequate where as the Linea alba incision may be a little longer. After the vascular stumps were inspected the port site was closed. Close proximity of the instruments leads to clashing and this could be overcome to an extent with instruments of varying lengths and articulating or flexible instruments. However we have used both the conventional rigid instruments as well as articulating instruments.
3. Results
All procedures were completed with no major complications. In 3 cases an additional 5 mm port was added to hasten the dissection. There were 4 female donors and two males and their age varied between 25 to 68 years. Their body mass index was between 22 and 28.7. We have used the R-port on 4 occasions and SILS port in two. Five left and one right kidney was procured. Four kidneys had single artery while two had two each. One kidney had two renal veins. Operating time was 4 - 5 hours. Estimated blood loss was 20 - 800 ml. Warm ischaemia period was between 4 to 10 minutes. Warm ischaemia was longer in three—in two there was instrument problem (longer stapler cartridge change over time) and in another an additional vein was identified after the division of the artery and the main vein and it required stapling and division. The kidney delivery skin incision length was between 3 to 5 cm. We followed the same post operative management as for laparoscopic donor nephrectomy

Figure 1. Shows the R-port being used at the umbilicus in LESS donor nephrectomy.

Figure 2. Shows the SILS port being used at the umbilicus in LESS donor nephrectomy.
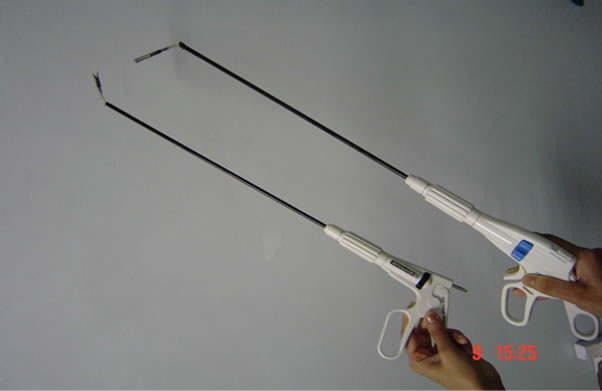
Figure 3. Shows a roticulator instrument used in LESS donor nephrectomy.
[7]. Post surgical hospital stay varied between 24 to 36 hours. The data of our 6 patients who underwent LESS donor nephrectomy are shown in Table 1.
We encountered intra operative complications in two— one had significant blood loss (800ml), when a thin branch was torn from the renal vein with no hemodynamic changes or requirement for blood transfusion. In another there was a parenchymal tear 1.5 cm long and 0.5 cm deep near the renal hilum not involving the vessels. In retrospect it was caused by the less than generous delivery skin incision. All kidneys functioned immediately after transplantation. There were two recipients who were desensitized using our protocol of Rituximab and plasmapheresis, One of them had low platelet count (1.86 × 105/L) and prolonged INR (1.5) at the time of surgery resulting in bleeding (general ooze) during the immediate post operative period with slower drop in serum creatinine. Recipients post transplant serum creatinine at one month ranged from 75 to 146 µmol/L.
4. Discussion
The landscape of minimally invasive surgery is in a state of constant evolution. Since the year 2000 there has been an increase in the number of live donor renal transplants and the total transplant activity in Australia. Increasing waiting times for deceased donor transplants and introduction of laparoscopic donor nephrectomy have contributed to this increased activity. Ratner et al. [8] performed the first laparoscopic donor nephrectomy in 1995 and it was introduced in Australia by our unit in 1997 [1]. This procedure has now become the gold standard and has replaced the open technique of donor nephrectomy in most centres. However it is a challenging technique, which requires good laparoscopic surgical expertise.
Efforts are presently focused on further reducing incisional morbidity while improving the cosmetic result. Some of these techniques are clustering of ports, SILS (single incision laparoscopic surgery) and Natural orifice translumenal endoscopic surgery (NOTES)—a recent innovation, implies intra-abdominal surgery via natural orifices (vagina, mouth/stomach, rectum) [6]. In a similar manner the umbilicus is an embryonic (E) natural orifice which, since it is a scar itself, conceals the intra-abdominal entry point for surgical procedures. In November 2007 E-NOTES (embryonic natural orifice transumbilical endoscopic surgery) was used to perform a single port transumbilical donor nephrectomy [5]. Laparoscopic nephrectomy is considered as a challenging procedure and Single port method increases the complexity of this procedure further.
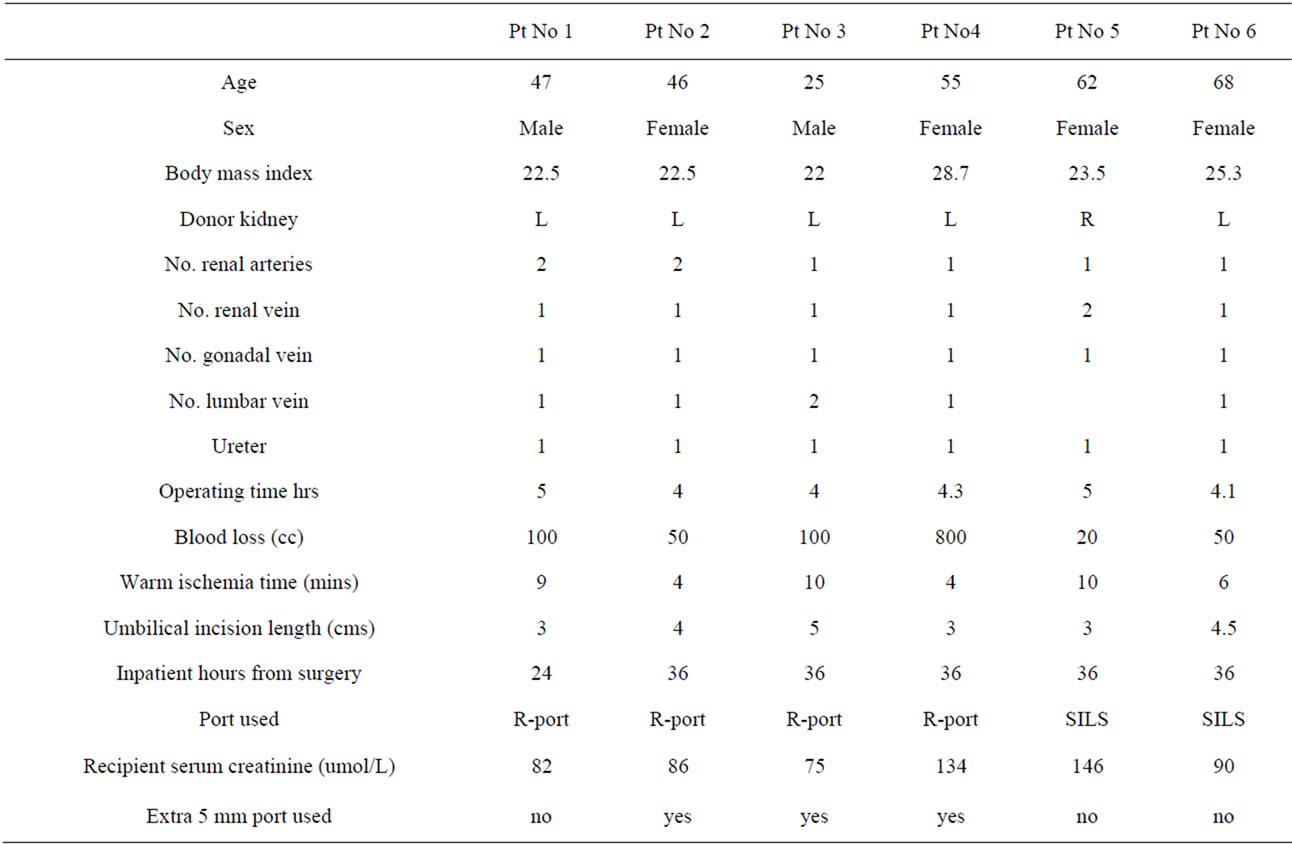
Table 1. Results of patients who have undergone LESS donor nephrectomy.
Traditional use of multiple ports to provide good triangulation is not possible with the Single port method. Clashing of instruments is a major problem and it can be overcome by using instruments of varying lengths and the new generation of currently available flexible instruments. Roticular instruments (Roticulator™ Endo Grasp™ 5 mm Covidien) though helpful were not designed to lift the kidney to facilitate the dissection of its vessels. It is a new learning curve to master this method. There may be a need to have an additional 5 mm port or a needlescope especially during the early experience as we and others [5,9,10] have done. With experience the need for this additional port/needle scope diminishes. Among the 2 LESS platforms that we have used we felt that the SILS™ Port (Covidien, USA) was better suited for conventional laparoscopic instruments. We believe it is ideal to choose thin patients, left kidney with normal anatomy for this procedure initially.
From our limited initial experience single port donor nephrectomy is technically feasible and safety needs to be confirmed by further experience. Operating time (4.44 ± 0.47 vs. 3.60 ± 0.99 hours) was longer compared to our conventional laparoscopic donor nephrectomy series reflecting our learning curve, but had no effect on the immediate graft function. The warm ischaemia times (7.2 ± 2.85 vs. 4.64 ± 1.71 minutes) were also longer. In three cases warm ischaemia was longer due to stated reasons and it has reflected on the whole group due to the limited numbers. Endo GIA stapler cartridge changing time varies with the experience of the instrument nurse and in larger training institutions the performance levels vary. Care should be given to make adequate skin incision to deliver the kidney as it is easy to misjudge the width of the kidney, a kidney which is coming up in a transverse lie, canal get easily damaged. In our series we had one kidney with a parenchymal tear 1.5 cm long and 0.5 cm deep near the renal hilum not involving the vessels. The post surgery hospital stay was a mean of 1.83 ± 0.4 days. Worldwide experience with this technique for donor nephrectomy is limited [9,11]. Laparoscopic method of donor nephrectomy has reduced the postoperative morbidity and hospital stay. It is difficult to show whether reducing the number of ports and shortening the delivery incision will further improve the benefits, till we gain more experience and the numbers to adequately assess this procedure. There is a need for randomized studies to assess its potential advantages both in terms of morbidity and cosmesis. There is also the possibility that this technically more difficult method may not be widely accepted if there are no demonstrable advantages.
5. Conclusion
Limitations of this study include small number and a retrospective study. Renal donors are highly motivated and may accept any method but some donors will definitely appreciate a shorter and less noticeable scar and lesser morbidity. If it is proven to reduce the postoperative morbidity and enable donors to return to work early, it has the potential to replace the current laparoscopic method in some select units, just as it replaced the open method for donor nephrectomy.
REFERENCES
- C. Hensman, G. Lionel, P. Hewett and M. M. Rao, “Laparoscopic Live Donor Nephrectomy: The Preliminary Experience,” Aust. N.Z. J. Surg, Vol. 69, 1999, pp. 365-368. doi:10.1046/j.1440-1622.1999.01574.x
- Healthy Kidney Removed Through Donor’s Vagina, “Science Daily (Feb. 4, 2009),” 2009. http://www.sciencedaily.com/releases/2009/02/090202175325.htm
- A. Rane, et al., “Single-Port-Access Nephrectomy and Other Laparoscopic Urologic Procedures Using a Novel Laparoscopic Port (R-Port),” Urology, Vol. 72, No. 2, 2008, pp. 260-263. doi:10.1016/j.urology.2008.01.078
- J. D. Raman, et al., “Single-Incision Laparoscopic Surgery: Initial Urological Experience and Comparison with Natural-Orifice Translumenal Endoscopic Surgery,” BJU International, Vol. 101, No. 12, 2008, pp. 1493-1496. doi:10.1111/j.1464-410X.2008.07586.x
- I. S. Gill, et al., “Single Port Transumbilical (E-NOTES) Donor Nephrectomy,” The Journal of Urology, Vol. 180, 2008, pp. 637-641. doi:10.1016/j.juro.2008.04.028
- J. Marescaux, B. Dallemagne, S. Perretta, A. Wattiez, D. Mutter and D. Coumaros, “Surgery without Scars: Report of Translumenal Cholecystectomy in a Human Being,” Archives of Surgery, Vol. 142, 2007, p. 823. doi:10.1001/archsurg.142.9.823
- M. M. Rao and C. H. Russell, “Laparoscopic Live Donor Nephrectomy,” ANZ Journal of Surgery, Vol. 75, 2005, pp. 6-9. doi:10.1111/j.1445-2197.2005.03288.x
- L. E. Ratner, L. J. Ciseck, R. G. Moore, F. G. Cigarroa, H. S. Kaufman and L. Kavoussi, “Laparoscopic Live Donor Nephrectomy,” Transplantation, Vol. 60, 1995, pp. 1047-1049.
- A. Kurien, S. Rajapurkar, L. Sinha, et al., “Standard Laparoscopic Donor Nephrectomy versus Laparoendoscopic Single-Site Donor Nephrectomy: A Randomised Comparative Study,” Journal of Endourology, Vol. 25, 2011, pp. 365-370. doi:10.1089/end.2010.0250
- Laparoendoscopic Single Site, “(LESS) versus Standard Laparoscopic Left Donor Nephrectomy: Matched-Pair Comparison,” European Urology, Vol. 57, 2009, pp. 95-101. doi:10.1016/j.eururo.2009.07.023
- I. S. Gill, “Laparoendoscopic Single-Site Surgery: Initial Hundred Patients,” Urology, Vol. 74, No. 4, 2009, pp. 805-812. doi:10.1016/j.urology.2009.02.083

