Open Journal of Modern Neurosurgery
Vol.4 No.3(2014), Article ID:48541,8 pages
DOI:10.4236/ojmn.2014.43027
Posterior Atlantoaxial Fusion Using C1 Lateral Mass and C2 Pedicle by Polyaxial Screw in Atlantoaxial Instability
O. Rezaee1, R. Salar1*, R. Jabari1, A. Shams Akhtari2, M. Taghizadeh2
1Neurosugery Department, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2Emergency Department, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Email: *amin.may1981@gmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 30 May 2014; revised 31 June 2014; accepted 29 July 2014
ABSTRACT
Objective: The aim of this study is to evaluate clinical and radiological outcomes in subjects of atlantoaxial instability which were operated using C1 lateral mass and C2 pedicle screw (Harmes technique). Materials and Methods: Twenty patients with atlantoaxial instability were scheduled at our clinic for atlantoaxial fusion using polyaxial C1 lateral mass and C2 pedicle screw between January 2008 and March 2014. Results: Trauma was the most common cause of atlantoaxial instability, seen in 18 (90%) patients. Modes of trauma were road traffic accident (75%) and falling (15%). Osteoarthritis was observed in 10% of cases. Patients were followed up with radiographs and clinical examinations. Satisfactory screw placement and reduction were achieved in all patients with the average union time of 3.5 months. There were no implant failures, nonunions, vertebral artery injuries or C2 nerve root injuries. Only, surgical site infections occur in 20% of cases that are improved with medical treatment. Conclusions: C1 lateral mass and C2 pedicle polyaxial screw fixation is an effective technique for the fusion of the atlantoaxial complex. It provides the highest fusion rates without any risk of vertebral injury.
Keywords: Atlantoaxial Instability, Polyaxial Screw, C1 Lateral Mass, C2 Pedicle, Fusion

1. Introduction
Atlantoaxial is characterized by a high degree of mobility and little intrinsic bony stability. Atlantoaxial instability is caused by excessive movement at the junction between the atlas (C1) and axis (C2) as a result of either a bony or ligamentous abnormality [1] [2] . The causes of atlantoaxial instability are numerous and include congenital malformations, trauma, neoplasm and inflammatory diseases and it is usually treated by reduction and stabilization of the C1-C2 joint [1] [3] . There are several surgical management techniques used to manage C1-C2 instability. Since the first description of the sublaminar wiring technique by Gallie in 1939, various modifications of the techniques had been suggested by Brooks-Jenkins, Sonntag and Goel-Laheri [2] [4] -[8] . Unfortunately, studies have shown that the non-union rates for these techniques are as high as 80% (range, 3% - 80%) [9] . Although these techniques had been developed and modified to achieve the better result of stabilization of atlantoaxial complex, the operations are still challenging due to devastating complications or technical difficulties. Interspinous fusion at C1-2 with sublaminar cables or interlaminar clamps cannot be performed if the posterior elements of C-1 or C-2 are absent or disrupted. Also, atlantoaxial transarticular screws cannot be placed successfully in the presence of a medially located VA, irreducible subluxation, severe cervicothoracic kyphosis, or destruction of the C-2 pars interarticularis [1] . In these cases constructs incorporating C-1 lateral mass screws may be used to achieve fixation. In 2001, Harms and Melcher further popularized the technique of posterior C1-C2 fusion with C1 lateral mass screw and C2 pedicle screw [10] [11] . The advantages of this new technique are more rigid fixation at C1 than those of most other options, favorable for inclusion into current instrumented constructs, safer trajectory of the screws, potential for post instrumentation reduction and avoidance of damage to the C1-C2 facet joint and potentially allow sparing of motion segments [2] [10] . Also, the risk of vertebral artery injury is lower and posterior reduction and fixation of C1 and C2 can be achieved [1] . In this study, we describe our clinical experience using the C1 lateral mass screw and C2 pedicle screw technique for posterior C1-C2 fusion.
2. Materials and Methods
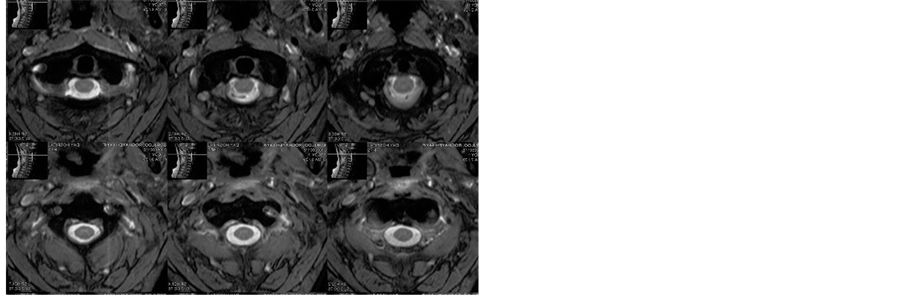
Twenty patients with atlantoaxial instability (Figures 1-3) were scheduled at our clinic for atlantoaxial fusion using polyaxial C1 lateral mass and C2 pedicle screws between January 2008 and March 2014. All aspects of our research was assessed and approved by Research Ethics Committee of Shahid Beheshti University. Neurological outcome graded using Frankel classification was assessed for all patients pre and post-operatively (Grade A: no function, Grade B: sensory only, Grade C: some sensory and motor preservation, Grade D: useful motor function, Grade E: normal function) [12] . Radiological assessment of union using plain radiographs, Computed Tomography (CT) scan and Magnetic Resonance Imaging (MRI) was done in all the cases pre and post-operatively. Also, all objects underwent pain assessment using Visual Analog Scale (VAS) preand post-operatively. This assessment tool was used for visualizing the patients’ pain among the study population in both preoperative and post-operative scenario. It consists of 10 point scale of 0 to 10, where “0” stands for no pain and “10” stands for unbearable/worst pain [13] . Statistical analysis was performed with paired-samples t-test from SPSS 21.0 for Windows statistical software (Chicago, IL, USA).
3. Operative Technique
Under general anesthesia, the patient was positioned prone using a Mayfield head holder. The neck was kept neutral with the head in the “military tuck” position. The arms were tucked in at the sides and the shoulders retracted caudally using tape. A midline incision was made, extending from the inion to C-3 if atlantoaxial fixation was planned. The incision was extended inferiorly as indicated by the planned procedure. A bilateral subperiosteal dissection of the paraspinal musculature was performed to expose the lateral margins of the facet joints at the C2-3. Dissection was continued laterally over the posterior arch of C-1, exposing the VA in the vertebral groove on the C-1 arch. Bipolar cautery and hemostatic agents such as gelfoam and fibrillar collagen were used to control bleeding from the perivertebral venous plexus. The C-2 nerve root was identified and mobilized inferiorly. The lateral mass of C-1 inferior to the C-1 arch was exposed. The medial wall of the lateral mass was identified using a forward-angle curette to identify the medial limit of screw placement (Figure 4, Figure 5). The medial aspect of the transverse foramen could also be identified and serves as the lateral limit for screw placement (Figure 6, Figure 10). The entry point for screw placement was identified 3 to 5 mm lateral to the medial wall of the lateral mass, at the junction of the lateral mass and inferior aspect of the C-1 arch. The superior aspect of the anterior tubercle was targeted with a mediolateral angle of 16 degrees conversion and craniocaudal angle of 20 degrees cephalad (Figure 7). The entry point might be varied depending on the distance of C-1 and C-2 was preserved. Otherwise, lateralarthrodesis was performed by carefully decorticating the exposed
 (a)
(a) (b)
(b) (c)
(c)
Figure 1. Preoperative right (a) and left (c) lateral, and AP (b) X-rays of a subject with atlantoaxial instability.
surfaces of the C1-2 joints by using a high-speed drill (Figure 8, Figure 9) and then packing cancellous iliac crest autograft over these joints. A hemovac drain was placed prior to wound closure.
4. Results
Twenty patients with atlantoaxial instability were studied. Of them 16 were males (80%) and 4 (20%) were females. The mean age at the time of surgery was 34.67 ± 11.50 years (range 16 - 65 years). Trauma was the most common cause of atlantoaxial instability, seen in 18 (90%) patients. Modes of trauma were road traffic accident (75%) and falling (15%). Osteoarthritis was observed in 10% of cases. Patients were followed up with radiographs and clinical examinations. Satisfactory screw placement and reduction were achieved in all patients with the average union time of 3.5 months (Figure 10). Neurological deficit was present in 17 subjects (85%). After the operation, all of these 17 patients had improvement in Frankel grade. Frankel scale assessment showed that 9 patients of grade D improved to grade E, 8 of grade C improved to grade E and 3 of grade E had no improvement in their neurological status at the final follow up. The mean of VAS pain scores decreased from 8.1 ± 1.3 preoperatively to 0.4 ± 1.1 postoperatively (p < 0.001). There were implant failures, nonunions, vertebral artery injuries or C2 nerve root injuries. Only, surgical site infections occur in 20% of cases that improved with medical treatment.
5. Discussion
The atlantoaxial complex, bearing the weight of the head and the atlantoaxial joint, generates most of the rotation of the head and neck [14] . Because of the high mobility of the C1-2 motion segment, fusion rates at this level have been substantially lower than those at the subaxial spine. The aim of treatment of atlantoaxial instability is to achieve a solid fusion between C1 and C2, virtually eliminating any motion between them [15] . This is expected to relieve the neck pain and avoid the risk of further neurological deficit.
Atlantoaxial fusion was first described by Mixter and Osgood in 1910 using braided sutures. The use of posterior cervical wiring of the lamina of C1 and C2 dates to 1939 in a report by Gallie [5] . The Gallie technique, although rather simple to perform, does not provide sufficient stability of the fixation site [5] [16] . Brooks and Jenkins further offered an alternative method of posterior C1-C2 laminar wiring in 1978 [16] . They described double graft compression between the lamina of the atlas and axis with a sublaminar wire [7] [14] . Brooks posterior fixation of the atlantoaxial vertebrae is more complicated, but it yields a more stable repair compared to the Gallie technique [17] . The posterior wiring techniques popularized by Gallieand Brooks and Jenkins had been the most common means of stabilization in the past [5] [16] . Although the posterior wiring procedure is easy
 (a)
(a)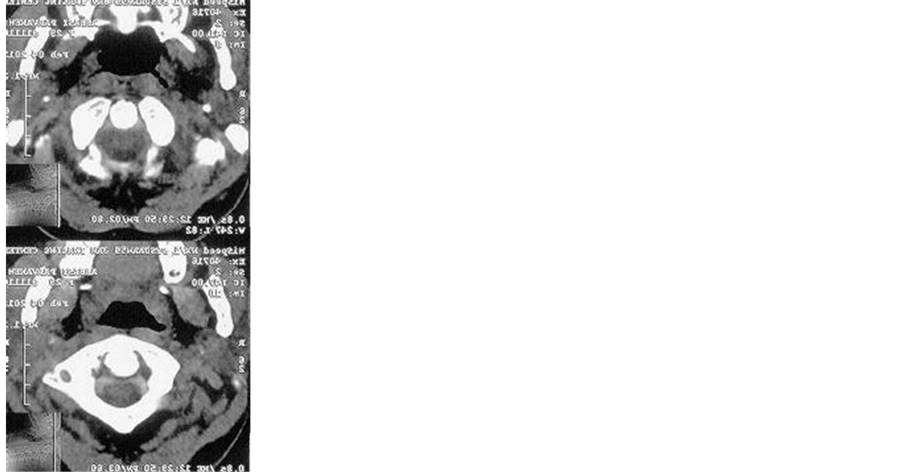 (b)
(b)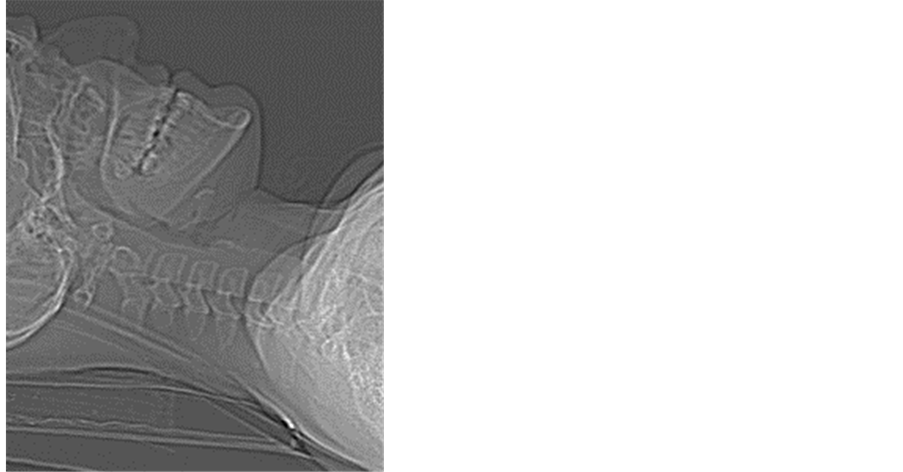 (c)
(c)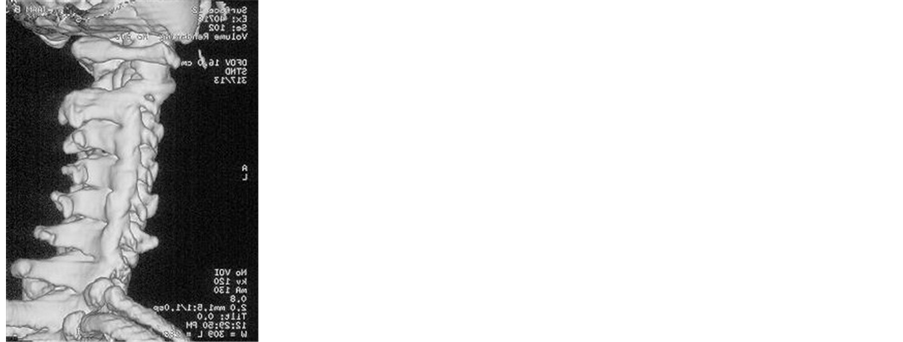 (d)
(d)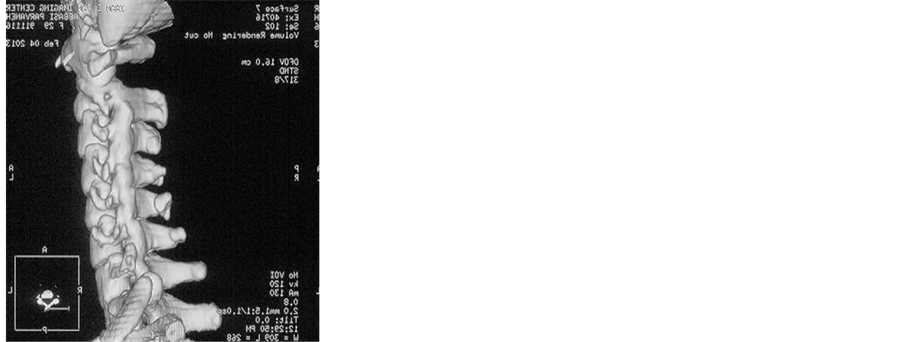 (e)
(e)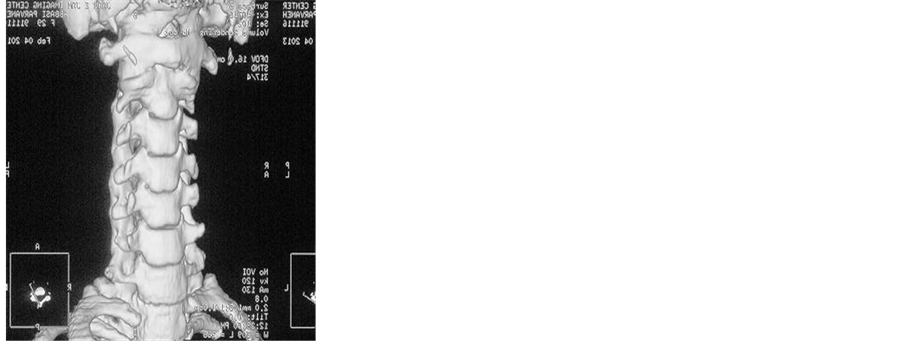 (f)
(f)
Figure 2. Preoperative scout view (a), axial (b), sagittal (c) and 3D (d), (e), (f) CT images showing C1-C2 instability.
 (a)
(a) (b)
(b)
Figure 3. Preoperative sagittal (a) and axial (b) MRI images showing spinal cord compression.

Figure 4. Photograph of a spine and VA model demonstrating the entry point for a C1 lateral mass screw.

Figure 5. Intraoperative picture of entry point for a C1 lateral mass screw.
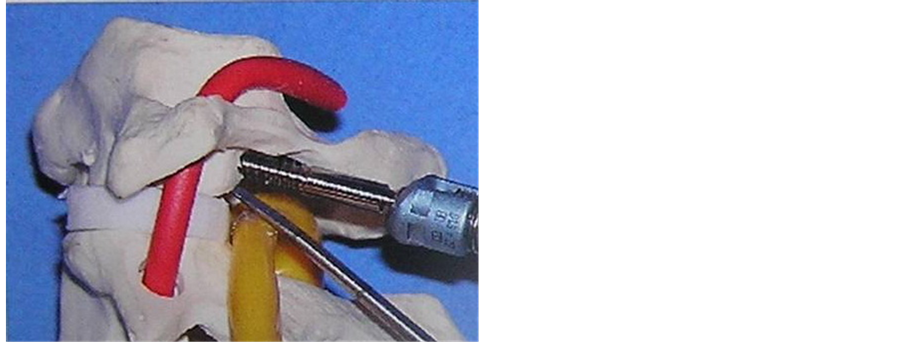
Figure 6. Photograph of screw placement.
to accomplish, this technique carries possible risk of dural or neuronal injury during procedure and the halo vest immobilization is required to accomplish successful bone fusion [2] .
Screw fixation techniques were developed after wiring techniques. Grob and Magerl introduced the transarticular technique, a technically difficult procedure, with the added risk of inadvertent injury to the vertebral artery not inherent in wiring techniques [18] . This technique requires meticulous preoperative planning and precise operative techniques are mandatory to achieve successful result and to avoid vertebral artery injury [2] .

Figure 7. The superior aspect of the anterior tubercle was targeted with a mediolateral angle of 16 degrees conversion and craniocaudal angle of 20 degrees cephalad.

Figure 8. Photograph of drilling screw hole.

Figure 9. Intraoperative picture of drilling screw hole.
Posterior screw fixation utilizing C1-C2 transarticular screws and C1 lateral mass screws with C2 pars screws were the final two alternative methods of posterior C1-C2 fixation. The C1 lateral mass screw with C2 pedicle screw construct was initially created with plates and screws by Goel et al. in the 1980’s and then subsequently popularized by Harms and Melcher in 2001 [6] [19] . Harms and Melcher reported a 100% fusion rate using C1 lateral mass and C2 pedicle screw. The complications reported in his study were deep wound infection, which occurred in 2.7% of cases. No vertebral artery injury or neurological complications were reported. Other studies also reported significant rates of perforation during C1 lateral mass and C2 pedicle screw insertion. Kwan et al. reported that the union rate of Harm’s technique was 100% with an average union time of 5.3 months (range from 3 to 8 months) in their patients. Also, the patients achieved an average of one Frankel grade neurological
Figure 10. Intraoperative picture of screw placement.
improvement postoperatively [7] . Yoon et al. have achieved excellent bone fusion using C1 lateral mass screw and C2 pedicle screw with polyaxial screw comparing with the result of other methods without any complications related to this procedure [2] . However, Gunnarsson et al. reported 12% incidence of temporary C2 neuralgia and 4.0% incidence of medial breach of the C1 lateral mass although this did not lead to any neurological events [10] .
In this study, we presented twenty patients with atlantoaxial instability treated by Harm’s technique. Excellent outcome was observed in terms of fusion rate, which was 100%. All the twenty follow up cases achieved union with the average union time of 3.5 months. In Harm’s technique, wire does not need to support or stabilize C1-C2 segment itself, unlikely in Gallie, Brook, or Sonntag’s technique. Because the C1-C2 segment is firmly stabilized with C1 lateral mass and C2 pedicle screw, the miniplate only needs to provide strength enough to stabilize autograft bone between the interlaminarspace until successful bone fusion is accomplished [2] . Also, use of this technique led to significant improvement in neurological recovery in 85% of cases that presented with neurological deficit preoperatively. After the operation, all of these 17 patients had improvement in Frankel grade. Frankel scale assessment showed that 9 patients of grade D improved to grade E, 8 of grade C improved to grade E and 3 of grade E had no improvement in their neurological status. This could be due to the superiority of this method in terms of reduction of the C1-C2 subluxation that therefore leads to improved indirect decompression of the spinal cord. Patients often complain postoperative neck pain after surgery and VAS is a well-recognized outcome tool to assess the severity of pain [13] . In this study, the mean of VAS pain scores decreased from 8.1 ± 1.3 preoperatively to 0.4 ± 1.1 postoperatively (p < 0.001). No surgical site infections, implant failures, nonunions, vertebral artery injuries or C2 nerve root injuries were observed.
6. Conclusion
Despite of our small patient population, we conclude that C1 lateral mass and C2 pedicle polyaxial screw fixation is an effective technique for the fusion of the atlantoaxial complex. It provides the highest fusion rates without any risk of vertebral injury.
References
- Califianeller, T., Yilmaz, C., Ozdmer, O. and Caner, H. (2008) Posterior Atlanto Lateral Mass Fixation Technique with Polyaxial Screw and Rod Fixation System. Turkish Neurosurgery, 18, 142-148.
- Yoon, S.M., Baek, J.W. and Kim, D.H. (2012) Posterior Atlantoaxial Fusion with C1 Lateral Mass Screw and C2 Pedicle Screw Supplemented with Miniplate Fixation for Interlaminar Fusion: A Preliminary Report. Journal of Korean Neurosurgical Society, 52, 120-125. http://dx.doi.org/10.3340/jkns.2012.52.2.120
- Bahadur, R., Goyal, T., Dhatt, S.S. and Tripathy, S.K. (2010) Transarticular Screw Fixation for Atlantoaxial Instability-Modified Margels Technique in 38 Patients. Journal of Orthopaedic Surgery and Research, 5, 1-8. http://dx.doi.org/10.1186/1749-799X-5-87
- Dickman, C.A., Sonntag, V.K., Papadopoulos, S.M. and Hadley, M.N. (1991) The Interspinous Method of Posterior Atlantoaxial Arthrodesis. Journal of Neurosurgery, 74, 190-198. http://dx.doi.org/10.3171/jns.1991.74.2.0190
- Gallie, W.E. (1939) Fracture and Dislocations of the Cervical Spine. The American Journal of Surgery, 46, 495-499. http://dx.doi.org/10.1016/S0002-9610(39)90309-0
- Goel, A., Desai, K. and Mazumdar, D. (2002) Atlantoaxial Fixation Using Plate and Screw Method: A Report of 160 Treated Patients. Neurosurgery, 51, 1351-1356.
- Kwan, M.K., Chan, C.Y.W., Kwan, T.C.C., Gash, Y.N. and Saw, L.B. (2010) Safety Issues and Neurological Improvement Following C1-C2 Fusion Using C1 Lateral Mass and C2 Pedicle Screw in Atlantoaxial Instability. Malaysian Orthopaedic Journal, 4, 17-22. http://dx.doi.org/10.5704/MOJ.1007.003
- Margel, F.S.P. (1987) Stable Posterior Fusion of the Atlas and Axis by Transarticular Screw Fixation. In: Kehr, P. and Weidner, A., Eds., Cervicale Spine I, Springer Wien Berlin Heidelberg, New York, 322-327.
- Reilly, T.M., Sasso, R.C. and Hall, P.V. (2003) Atlantoaxial Stabilization: Clinical Comparison of Posterior Cervical Wiring Technique with Transarticular Screw Fixation. Journal of Spinal Disorders Techniques, 16, 248-253. http://dx.doi.org/10.1097/00024720-200306000-00004
- Gunnarsson, T., Massicotte, E.M., Govender, P.V., Raja Rampersaud, Y. and Fehlings, M.G. (2007) The Use of C1 Lateral Mass Screws in Complex Cervical Spine Surgery: Indications, Techniques, and Outcome in a Prospective Consecutive Series of 25 Cases. Journal of Spinal Disorders Techniques, 20, 308-316. http://dx.doi.org/10.1097/01.bsd.0000211291.21766.4d
- Mummaneni, P.V. and Haid, R.W. (2005) Atlantoaxial Fixation: Overview of All Techniques. Neurology India, 53, 409-415. http://dx.doi.org/10.4103/0028-3886.22606
- Frankel, H.L., Hancock, D.O., Hyslop, G., Melzak, J., Michaelis, L.S., Ungar, G.H., et al. (1969) The Value of Postural Reduction in the Initial Management of Closed Injuries of the Spine with Paraplegia and Tetraplegia. I. Paraplegia, 7, 179-192.http://dx.doi.org/10.1038/sc.1969.30
- Sharma, M.K., Chichanovskaya, L.V., Shlemsky, V.A. and Petrukhina, E. (2013) A Comprehensive Study of Outcome after Lumbar Discectomy for Lumbar Degenerative Spine Disease at 6 Months Post-Operative Period. The Open Neurosurgery Journal, 6, 1-5. http://dx.doi.org/10.2174/1876529701306010001
- Pang, D. and Li, V. (2004) Atlantoaxial Rotator Fixation: Part 1—Biomechanics of Normal Rotation at Atlantoaxial Joint in Children. Neurosurgery, 55, 614-625. http://dx.doi.org/10.1227/01.NEU.0000134386.31806.A6
- Hanimoglu, H., Hancl, L., Kaynar, M.Y. and Hancl, M. (2009) Bilateral C1-C2 Claw for Atlantoaxial Instability. Turkish Neurosurgery, 19, 345-348.
- Brooks, A.L. and Jenkins, E.B. (1978) Atlanto-Axial Arthrodesis by the Wedge Compression Method. Journal of Bone and Joint Surgery, 60, 279-284.
- Saito, R., Hase, H., Mikami, Y., Tsuji, Y., Ikeda, T., Osawa, T., et al. (2006) Clinical Study of a Modified Brooks Technique for Atlanto-Axial Subluxation Using Polyethylene Tape. Journal of Spinal Disorders Techniques, 19, 11-17. http://dx.doi.org/10.1097/01.bsd.0000173839.51476.63
- Grob, D. and Magerl, F. (1987) Surgical Stabilization of C1 and C2 Fractures. Orthopade, 16, 46-54.
- Goel, A. and Laheri, V. (1994) Plate and Screw Fixation for Atlantoaxial Subluxation. Acta Neurochirurgica (Wien), 129, 47-53. http://dx.doi.org/10.1007/BF01400872
NOTES

*Corresponding author.

