 Pharmacology & Pharmacy, 2011, 2, 354-360 doi:10.4236/pp.2011.24046 Published Online October 2011 (http://www.SciRP.org/journal/pp) Copyright © 2011 SciRes. PP Basic Research―Significance of Detection and Clinical Impact of Candida albicans in Non-Immunosuppressed Patients Petra Heizmann1, Frank Klefisch2, Wolfgang R. Heizmann3 1St. Wolfgang Clinic, Internal Medicine, Bad Griesbach, Germany; 2Paulinenhaus Krankenanstalt e.V., Berlin, Germany; 3Centre for Medical Microbiology and Infectiology, Berlin, Germany. Email: wrheizmann@aol.com Received May 15th, 2011; revised September 14th, 2011; accepted September 30th, 2011. ABSTRACT Background: The clinical significance of the detection of Candida albicans on mucous membranes of the respiratory or intestinal tract from patients in intensive care units is still not finally clarified. Many patients reveal colonization, al- though, despite increased risk, there are only a few invasive infections detectable. Therefore, antimycotic therapy in this setting is strongly discouraged. In reality, however, many patients receive antimycotics as a pre-emptive therapy. To elucidate this point, a literature research was performed. Results: In the light of new results on the pathogenicity of C. albicans, the recommendation not to treat should be discussed anew. Without becoming invasive, C. albicans influences the immune system negatively in an anti-inflammatory sense (Th2) by means of at least two distinct mechanisms [action on toll like receptors (TLR), production of farnesol], which will be discussed. Conclusion: It is believed that patients in the phase of CARS or MARS can be further endangered by concomitant colonization of mucous membranes by C. albi- cans, i.e., in the sense of an anti-inflammatory immune response. Treatment with azole preparations, like fluconazole, which interacts with ergosterol synthesis in this phase of the disease, may trigger an additional effect on the patient, through increase of farnesol concentration by way of a negative feedback. Results of animal experiments on the immune system and concomitant therapeutic consequences indicate the need for verification through clinical trials. Keywords: Candida Albicans, Farnesol, Azole, Echinocandin, TLR, Immune Answer, Th Cell 1. Introduction “The diagnosis of pulmonary moniliasis (C. albicans- Infection) is fraught with difficulties … Actually there are no indisputable criteria for establishing the diagno- sis…” [1]. Even after 50 years the clinical significance of a detection of Candida in the respiratory or intestinal tract is greatly disputed. Based on the results of studies performed on non-neutropenic patients, the detection of Candida species in specimen of the deep respiratory tract, even in high concentrations, is regarded as colonization of mucous membranes rather than invasive infection [2], Therefore, in many cases, administration of anti-fungal drugs is regarded as unwarranted and expensive [3]. On the other hand, colonization of mucous membranes represents a significant risk factor for invasive Can- dida-infections [4-6]. For example, in a previous study, growth of Candida in at least one specimen was positive in 215 of 357 patients (60.2%) [7]. Candida was mostly detected in secretions of the respiratory tract (49.8%), in rectal smears (48.3%) and in wounds (20.1%). The rela- tive part of Candida albicans was 72%, Candida gla- brata 16%, Candida tropicalis 5%, Candida parapsilosis 3% and Candida krusei 2%. A colonization—particularly in several localizations—together with other risk factors such as loss of skin and mucous membrane barrier func- tion, major surgical procedures (in particular abdominal), burns, total parenteral nutrition, acute renal failure and haemodialysis, high APACHE II scores, antacids and artificial respiration can contribute to an increased risk of invasive Candida infections. However, the number of proven invasive infections (detection in blood cultures, Candida endophthalmitis, growth from usually sterile specimen such as pleural or peritoneal fluid) based on the number of patients with colonization, is rather rare. Of a total of 1669 patients, 719 patients had no colonization or 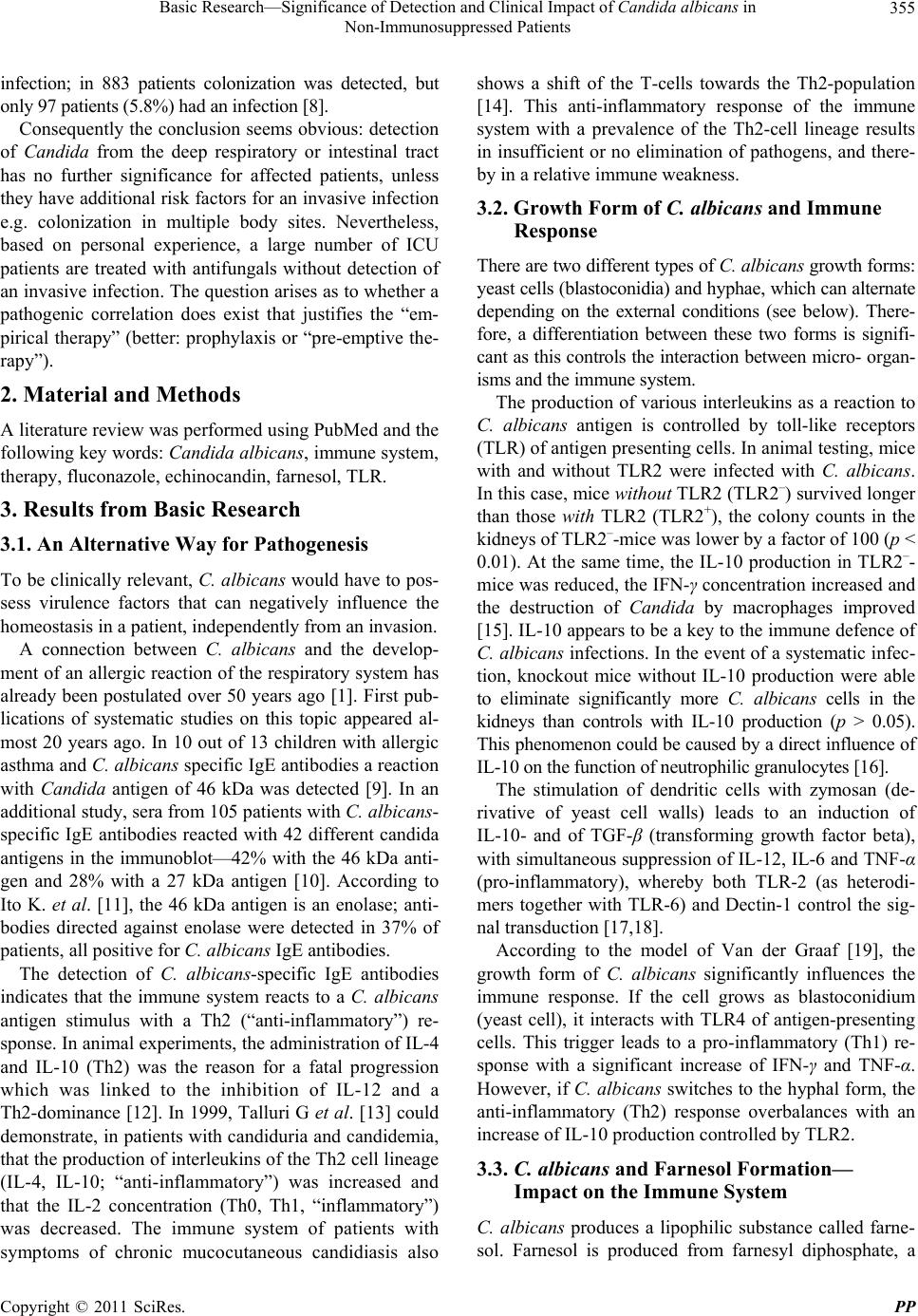 Basic Research—Significance of Detection and Clinical Impact of Candida albicans in 355 Non-Immunosuppressed Patients infection; in 883 patients colonization was detected, but only 97 patients (5.8%) had an infection [8]. Consequently the conclusion seems obvious: detection of Candida from the deep respiratory or intestinal tract has no further significance for affected patients, unless they have additional risk factors for an invasive infection e.g. colonization in multiple body sites. Nevertheless, based on personal experience, a large number of ICU patients are treated with antifungals without detection of an invasive infection. The question arises as to whether a pathogenic correlation does exist that justifies the “em- pirical therapy” (better: prophylaxis or “pre-emptive the- rapy”). 2. Material and Methods A literature review was performed using PubMed and the following key words: Candida albicans, immune system, therapy, fluconazole, echinocandin, farnesol, TLR. 3. Results from Basic Research 3.1. An Alternative Way for Pathogenesis To be clinically relevant, C. albicans would have to pos- sess virulence factors that can negatively influence the homeostasis in a patient, independently from an invasion. A connection between C. albicans and the develop- ment of an allergic reaction of the respiratory system has already been postulated over 50 years ago [1]. First pub- lications of systematic studies on this topic appeared al- most 20 years ago. In 10 out of 13 children with allergic asthma and C. albicans specific IgE antibodies a reaction with Candida antigen of 46 kDa was detected [9]. In an additional study, sera from 105 patients with C. albicans- specific IgE antibodies reacted with 42 different candida antigens in the immunoblot—42% with the 46 kDa anti- gen and 28% with a 27 kDa antigen [10]. According to Ito K. et al. [11], the 46 kDa antigen is an enolase; anti- bodies directed against enolase were detected in 37% of patients, all positive for C. albicans IgE antibodies. The detection of C. albicans-specific IgE antibodies indicates that the immune system reacts to a C. albicans antigen stimulus with a Th2 (“anti-inflammatory”) re- sponse. In animal experiments, the administration of IL-4 and IL-10 (Th2) was the reason for a fatal progression which was linked to the inhibition of IL-12 and a Th2-dominance [12]. In 1999, Talluri G et al. [13] could demonstrate, in patients with candiduria and candidemia, that the production of interleukins of the Th2 cell lineage (IL-4, IL-10; “anti-inflammatory”) was increased and that the IL-2 concentration (Th0, Th1, “inflammatory”) was decreased. The immune system of patients with symptoms of chronic mucocutaneous candidiasis also shows a shift of the T-cells towards the Th2-population [14]. This anti-inflammatory response of the immune system with a prevalence of the Th2-cell lineage results in insufficient or no elimination of pathogens, and there- by in a relative immune weakness. 3.2. Growth Form of C. albicans and Immune Response There are two different types of C. albicans growth forms: yeast cells (blastoconidia) and hyphae, which can alternate depending on the external conditions (see below). There- fore, a differentiation between these two forms is signifi- cant as this controls the interaction between micro- organ- isms and the immune system. The production of various interleukins as a reaction to C. albicans antigen is controlled by toll-like receptors (TLR) of antigen presenting cells. In animal testing, mice with and without TLR2 were infected with C. albicans. In this case, mice without TLR2 (TLR2–) survived longer than those with TLR2 (TLR2+), the colony counts in the kidneys of TLR2–-mice was lower by a factor of 100 (p < 0.01). At the same time, the IL-10 production in TLR2–- mice was reduced, the IFN-γ concentration increased and the destruction of Candida by macrophages improved [15]. IL-10 appears to be a key to the immune defence of C. albicans infections. In the event of a systematic infec- tion, knockout mice without IL-10 production were able to eliminate significantly more C. albicans cells in the kidneys than controls with IL-10 production (p > 0.05). This phenomenon could be caused by a direct influence of IL-10 on the function of neutrophilic granulocytes [16]. The stimulation of dendritic cells with zymosan (de- rivative of yeast cell walls) leads to an induction of IL-10- and of TGF-β (transforming growth factor beta), with simultaneous suppression of IL-12, IL-6 and TNF-α (pro-inflammatory), whereby both TLR-2 (as heterodi- mers together with TLR-6) and Dectin-1 control the sig- nal transduction [17,18]. According to the model of Van der Graaf [19], the growth form of C. albicans significantly influences the immune response. If the cell grows as blastoconidium (yeast cell), it interacts with TLR4 of antigen-presenting cells. This trigger leads to a pro-inflammatory (Th1) re- sponse with a significant increase of IFN-γ and TNF-α. However, if C. albicans switches to the hyphal form, the anti-inflammatory (Th2) response overbalances with an increase of IL-10 production controlled by TLR2. 3.3. C. albicans and Farnesol Formation— Impact on the Immune System C. albicans produces a lipophilic substance called farne- sol. Farnesol is produced from farnesyl diphosphate, a Copyright © 2011 SciRes. PP 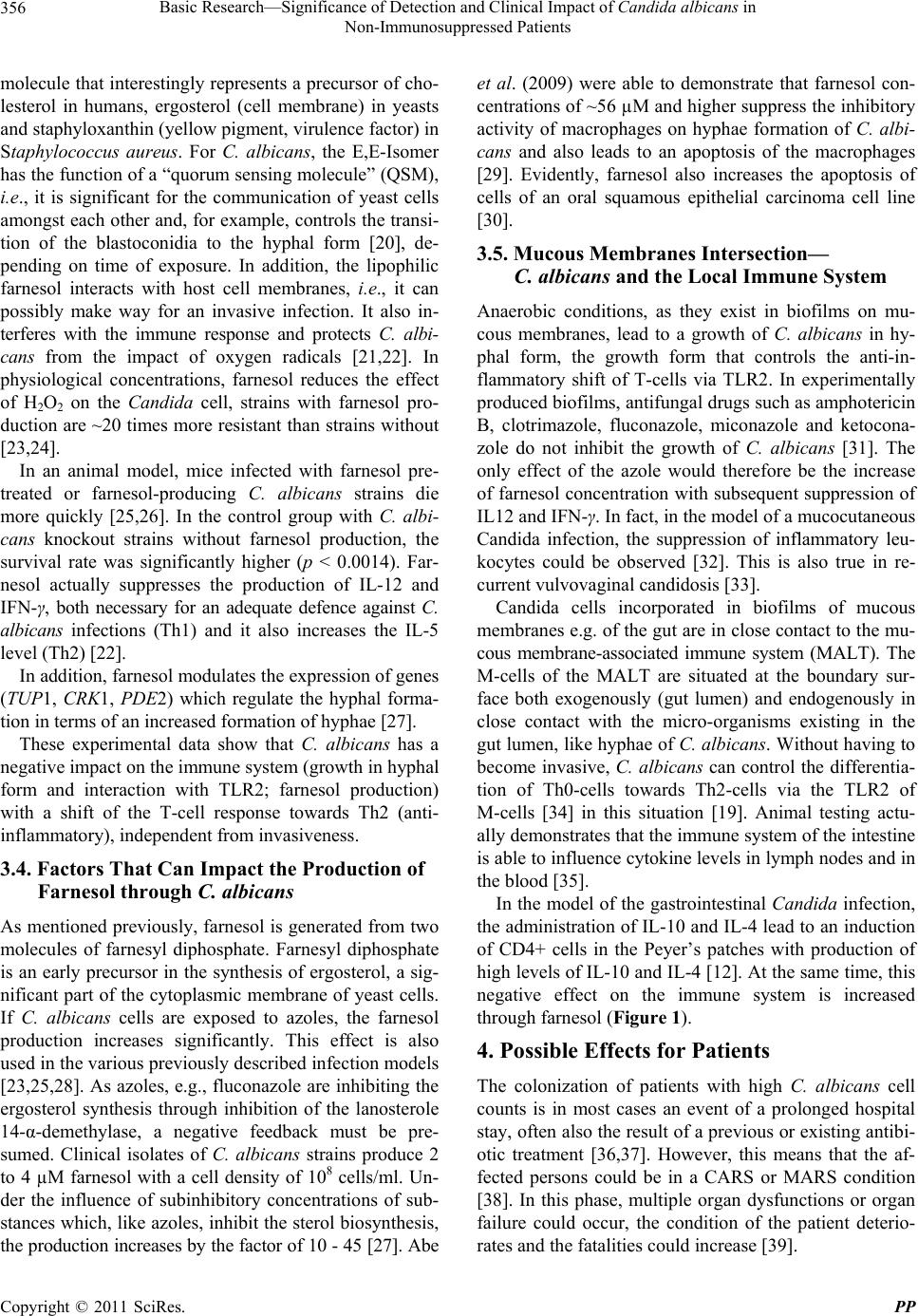 Basic Research—Significance of Detection and Clinical Impact of Candida albicans in 356 Non-Immunosuppressed Patients molecule that interestingly represents a precursor of cho- lesterol in humans, ergosterol (cell membrane) in yeasts and staphyloxanthin (yellow pigment, virulence factor) in Staphylococcus aureus. For C. albicans, the E,E-Isomer has the function of a “quorum sensing molecule” (QSM), i.e., it is significant for the communication of yeast cells amongst each other and, for example, controls the transi- tion of the blastoconidia to the hyphal form [20], de- pending on time of exposure. In addition, the lipophilic farnesol interacts with host cell membranes, i.e., it can possibly make way for an invasive infection. It also in- terferes with the immune response and protects C. albi- cans from the impact of oxygen radicals [21,22]. In physiological concentrations, farnesol reduces the effect of H2O2 on the Candida cell, strains with farnesol pro- duction are ~20 times more resistant than strains without [23,24]. In an animal model, mice infected with farnesol pre- treated or farnesol-producing C. albicans strains die more quickly [25,26]. In the control group with C. albi- cans knockout strains without farnesol production, the survival rate was significantly higher (p < 0.0014). Far- nesol actually suppresses the production of IL-12 and IFN-γ, both necessary for an adequate defence against C. albicans infections (Th1) and it also increases the IL-5 level (Th2) [22]. In addition, farnesol modulates the expression of genes (TUP1, CRK1, PDE2) which regulate the hyphal forma- tion in terms of an increased formation of hyphae [27]. These experimental data show that C. albicans has a negative impact on the immune system (growth in hyphal form and interaction with TLR2; farnesol production) with a shift of the T-cell response towards Th2 (anti- inflammatory), independent from invasiveness. 3.4. Factors That Can Impact the Production of Farnesol through C. albicans As mentioned previously, farnesol is generated from two molecules of farnesyl diphosphate. Farnesyl diphosphate is an early precursor in the synthesis of ergosterol, a sig- nificant part of the cytoplasmic membrane of yeast cells. If C. albicans cells are exposed to azoles, the farnesol production increases significantly. This effect is also used in the various previously described infection models [23,25,28]. As azoles, e.g., fluconazole are inhibiting the ergosterol synthesis through inhibition of the lanosterole 14-α-demethylase, a negative feedback must be pre- sumed. Clinical isolates of C. albicans strains produce 2 to 4 µM farnesol with a cell density of 108 cells/ml. Un- der the influence of subinhibitory concentrations of sub- stances which, like azoles, inhibit the sterol biosynthesis, the production increases by the factor of 10 - 45 [27]. Abe et al. (2009) were able to demonstrate that farnesol con- centrations of ~56 µM and higher suppress the inhibitory activity of macrophages on hyphae formation of C. albi- cans and also leads to an apoptosis of the macrophages [29]. Evidently, farnesol also increases the apoptosis of cells of an oral squamous epithelial carcinoma cell line [30]. 3.5. Mucous Membranes Intersection— C. albicans and the Local Immune System Anaerobic conditions, as they exist in biofilms on mu- cous membranes, lead to a growth of C. albicans in hy- phal form, the growth form that controls the anti-in- flammatory shift of T-cells via TLR2. In experimentally produced biofilms, antifungal drugs such as amphotericin B, clotrimazole, fluconazole, miconazole and ketocona- zole do not inhibit the growth of C. albicans [31]. The only effect of the azole would therefore be the increase of farnesol concentration with subsequent suppression of IL12 and IFN-γ. In fact, in the model of a mucocutaneous Candida infection, the suppression of inflammatory leu- kocytes could be observed [32]. This is also true in re- current vulvovaginal candidosis [33]. Candida cells incorporated in biofilms of mucous membranes e.g. of the gut are in close contact to the mu- cous membrane-associated immune system (MALT). The M-cells of the MALT are situated at the boundary sur- face both exogenously (gut lumen) and endogenously in close contact with the micro-organisms existing in the gut lumen, like hyphae of C. albicans. Without having to become invasive, C. albicans can control the differentia- tion of Th0-cells towards Th2-cells via the TLR2 of M-cells [34] in this situation [19]. Animal testing actu- ally demonstrates that the immune system of the intestine is able to influence cytokine levels in lymph nodes and in the blood [35]. In the model of the gastrointestinal Candida infection, the administration of IL-10 and IL-4 lead to an induction of CD4+ cells in the Peyer’s patches with production of high levels of IL-10 and IL-4 [12]. At the same time, this negative effect on the immune system is increased through farnesol (Figure 1). 4. Possible Effects for Patients The colonization of patients with high C. albicans cell counts is in most cases an event of a prolonged hospital stay, often also the result of a previous or existing antibi- otic treatment [36,37]. However, this means that the af- fected persons could be in a CARS or MARS condition [38]. In this phase, multiple organ dysfunctions or organ failure could occur, the condition of the patient deterio- rates and the fatalities could increase [39]. Copyright © 2011 SciRes. PP  Basic Research—Significance of Detection and Clinical Impact of Candida albicans in 357 Non-Immunosuppressed Patients Blastoconidi TLR 4 TLR 2 Antigen-presenting cell Hypha Th1-answer inflammatory IL-10 Th2-answer anti-inflammatory Farnesol-diphosphate Farnesol IL-5 IL-12 Figure 1. Impact of C. albicans on the immune system. Blas- toconidia cause the stimulation of the inflammatory Th1 response by TLR4 mediated activation of antigen-pre- senting cells. Hyphae stimulate TLR2 signalling and pro- duction of IL-10 which promotes an anti-inflammatory Th2 response. Farnesol leads to up-regulation of IL-5 and down- regulation of IL-12 and IFNγ promoting the Th2 response. In patients with a colonization of the mucous mem- branes through C. albicans, the immune system could be weakened via the above-mentioned mechanisms during this critical period of illness. If it is now decided—often also because previous antibiotic treatments have not re- sulted in an improved clinical condition—to eliminate the yeasts by administering antifungal drugs, fluconazole is often selected nowadays. However, this decision in particular could be associ- ated with serious disadvantages for the patient, in light of the illustrated pathogenic processes. In the case of a sep- sis through a Gram-negative pathogen like Escherichia coli, the production of IL-12 usually increases via the release of liopolysaccharides of the cell wall. A Th1- response develops that leads to an inflammatory response and therefore to elimination of the pathogen. However, Navarathna et al. [26] demonstrated in their experiment that, under the influence of farnesol, this IL-12 stimula- tion remains absent: therefore, a significant function of the immune system fails (Table 1). 5. Conclusion and Therapeutic Consequences Basic research of previous years has demonstrated how actively C. albicans can impact the host immune system via TLR and farnesol production in terms of an anti-in- Table 1. Changes of the IL-12 production under the influence of LPS, IFN-γ and farnesol [26]. Average IL-12 production (pg/ml) Pre-treatment p40 p70 None 1.5 4.25 Farnesol (100 µM) 0.33 2 IFN-γ + LPS 3215 40.8 Farnesol + IFN-γ + LPS 1.7 7.1 flammatory (Th2) immune response. Thus, the detection of C. albicans on mucous membranes obtains—at least in some patients—a completely new, clinically relevant sig- nificance. Precisely in those patients who are in the phase of CARS or MARS with reduced cellular defence, an increase of this process in phases with bacterial translo- cation could lead to a worsening in the course of the dis- ease. Due to the results of basic research, a rational basis exists nowadays to treat these patients with antifungal drugs in order to interrupt the pathogenic process of the immune modulation. Azole should subsequently not be prescribed for critically ill patients as this would result in an increase of farnesol formation by a negative feedback through inhibition of the ergosterol synthesis. Contrary to azoles, echinocandins like caspofungin or anidulafungin do not inhibit the ergosterol metabolism of C. albicans and are effective in biofilms [40]: C. albicans is eliminated without directly resulting in an increase of the farnesol concentration through negative feedback. In addition, echinocandins possess a further significant property. They interfere with the cell wall of C. albicans, which mainly consists of β-glucans and that have an im- pact on the immune system in terms of a pro-inflamma- tory response. However, this characteristic does not usu- ally occur as the β-glucans are not accessible to the im- mune system through an external mannan layer. Only when C. albicans cells are exposed to sub-inhibitory concentrations of caspofungin the level of TNFα (Th1- response) increases three to four times under experimen- tal conditions, in comparison to untreated Candida cells [41]. The model presented here—immune modulating effects of C. albicans—could also explain the debated superior clinical outcome of anidulafungin in comparison to flu- conazole in C. albicans infections [42]. Of specific interest are future clinical studies in which the design is applied such that it can demonstrate which patients with C. albicans colonization ideally benefit from an echinocandin therapy. Copyright © 2011 SciRes. PP  Basic Research—Significance of Detection and Clinical Impact of Candida albicans in 358 Non-Immunosuppressed Patients REFERENCES [1] E. L. Keeney, “Pulmonary Mycotic Infections; Allergic and Immunologic Factors,” California Medicine, Vol. 81, No. 6, 1954, pp. 367-378. [2] J. Rello, M. E. Esandi, E. Diaz, D. Mariscal, M. Gallego and J. Valles, “The Role of Candida sp Isolated from Bron- choscopic Samples in Nonneutropenic Patients,” Chest, Vol. 114, No. 1, 1998, pp. 146-149. doi:10.1378/chest.114.1.146 [3] J. Barenfanger, P. Arakere, R. D. Cruz, A. Imran, C. Drake, J. Lawhorn, S. J. Verhulst and N. Khardori, “Im- proved Outcomes Associated with Limiting Identification of Candida spp. in Respiratory Secretions,” Journal of Clinical Microbiology, Vol. 41, No. 12, 2003, pp. 5645- 5649. doi:10.1128/JCM.41.12.5645-5649.2003 [4] D. Pittet, M. Monod, P. M. Suter, E. Frenk and R. Auck- enthaler, “Candida Colonization and Subsequent Infec- tions in Critically Ill Surgical Patients,” Annals of Surgery, Vol. 220, No. 6, 1994, pp. 751-758. doi:10.1097/00000658-199412000-00008 [5] D. R. Reagan, M. A. Pfaller, R. J. Hollis and R. P. Wen- zel, “Characterization of the Sequence of Colonization and Nosocomial Candidemia Using DNA Fingerprinting and a DNA Probe,” Journal of Clinical Microbiology, Vol. 28, No. 12, 1990, pp. 2733-2738. [6] A. Voss, R. J. Hollis, M. A. Pfaller, R. P. Wenzel and B. N. Doebbeling, “Investigation of the Sequence of Colo- nization and Candidemia in Nonneutropenic Patients,” Journal of Clinical Microbiology, Vol. 32, No. 4, 1994, pp. 975-980. [7] M. Laverdiere, A. C. Labbe, C. Restieri, C. Rotstein, D. Heyland, S. Madger and T. Stewart, “Susceptibility Pat- terns of Candida Species Recovered from Canadian In- tensive Care Units,” Journal of Critical Care, Vol. 22, No. 3, 2007, pp. 245- 250. doi:10.1016/j.jcrc.2006.10.038 [8] C. Leon, S. Ruiz-Santana, P. Saavedra, B. Almirante, J. Nolla-Salas, F. Alvarez-Lerma, J. Garnacho-Montero and M. A. Leon, “A Bedside Scoring System (“Candida score”) for Early Antifungal Treatment in Nonneutropenic Criti- cally Ill Patients with Candi da Colonization,” Critical Care Medicine, Vol. 34, No. 3, 2006, pp. 730-737. doi:10.1097/01.CCM.0000202208.37364.7D [9] J. Savolainen, M. Viander and A. Koivikko, “IgE-, IgA- and IgG-Antibody Responses to Carbohydrate and Pro- tein Antigens of Candida albicans in Asthmatic Chil- dren,” Allergy, Vol. 45, No. 1, 1990, pp. 54-63. doi:10.1111/j.1398-9995.1990.tb01084.x [10] J. Savolainen, “A Standardized Densitometric Immuno- blotting Analysis of Candida albicans Protein Allergens,” Clinical & Experimental Allergy, Vol. 25, No. 4, 1995, pp. 357-363. doi:10.1111/j.1365-2222.1995.tb01054.x [11] K. Ito, A. Ishiguro, T. Kanbe, K. Tanaka and S. Torii, “Detection of IgE Antibody against Candida albicans enolase and Its Crossreactivity to Saccharomyces cere- visiae Enolase,” Clinical & Experimental Allergy, Vol. 25, No. 6, 1995, pp. 522-528. doi:10.1111/j.1365-2222.1995.tb01089.x [12] L. Tonnetti, R. Spaccapelo, E. Cenci, A. Mencacci, P. Puccetti, R. L. Coffman, F. Bistoni and L. Romani, “In- terleukin-4 and -10 Exacerbate Candidiasis in Mice,” European Journal of Immunology, Vol. 25, No. 6, 1995, pp. 1559-1565. doi:10.1002/eji.1830250614 [13] G. Talluri, V. K. Marella, D. Shirazian and G. J. Wise, “Immune Response in Patients with Persistent Candiduria and Occult Candidemia,” Journal of Urology, Vol. 162, No. 4, 1999, pp. 1361-1364. doi:10.1016/S0022-5347(05)68288-2 [14] D. Lilic, I. Gravenor, N. Robson, D. A. Lammas, P. Drysdale, J. E. Calvert, A. J. Cant and M. Abinun, “De- regulated Production of Protective Cytokines in Response to Candida albicans Infection in Patients with Chronic Mucocutaneous Candidiasis,” Infection and Immunity, Vol. 71, No. 10, 2003, pp. 5690-5699. doi:10.1128/IAI.71.10.5690-5699.2003 [15] M. G. Netea, R. Sutmuller, C. Hermann, C. A. van der Graaf, J. W. van der Meer, J. H. van Krieken, T. Hartung, G. Adema and B. J. Kullberg, “Toll-Like Receptor 2 Sup- presses Immunity against Candida albicans through In- duction of IL-10 and Regulatory T Cells,” Journal of Immunology, Vol. 172, No. 6, 2004, pp. 3712-3718. [16] A. Vazquez-Torres, J. Jones-Carson, R. D. Wagner, T. Warner and E. Balish, “Early Resistance of interleukin-10 Knockout Mice to Acute Systemic Candidiasis,” Infection and Immunity, Vol. 67, No. 2, 1999, pp. 670-674. [17] S. Dillon, S. Agrawal, K. Banerjee, J. Letterio, T. L. Denning, K. Oswald-Richter, D. J. Kasprowicz, K. Kellar, J. Pare, T. van Dyke, S. Ziegler, D. Unutmaz and B. Pu- lendran, “Yeast Zymosan, a Stimulus for TLR2 and Dec- tin-1, Induces Regulatory Antigen-Presenting Cells and Immunological Tolerance,” Journal of Clinical Investiga- tion, Vol. 116, No. 4, 2006, pp. 916-928. doi:10.1172/JCI27203 [18] M. G. Netea, F. van de Veerdonk, I. Verschueren, J. W. van der Meer and B. J. Kullberg, “Role of TLR1 and TLR6 in the Host Defense against Disseminated Can- didiasis,” FEMS Immunology & Medical Microbiology, Vol. 52, No. 1, 2008, pp. 118-123. doi:10.1111/j.1574-695X.2007.00353.x [19] C. A. van der Graaf, M. G. Netea, I. Verschueren, J. W. van der Meer and B. J. Kullberg, “Differential Cytokine Production and Toll-Like Receptor Signaling Pathways by Candida albicans Blastoconidia and Hyphae,” Infec- tion and Immunity, Vol. 73, No. 11, 2005, pp. 7458-7464. doi:10.1128/IAI.73.11.7458-7464.2005 [20] D. D. Mosel, R. Dumitru, J. M. Hornby, A. L. Atkin and K. W. Nickerson, “Farnesol Concentrations Required to Block Germ Tube Formation in Candida albicans in the Presence and Absence of Serum,” Applied and Environmental Mi- crobiology, Vol. 71, No. 8, 2005, pp. 4938-4940. doi:10.1128/AEM.71.8.4938-4940.2005 [21] J. M. Hornby, E. C. Jensen, A. D. Lisec, J. J. Tasto, B. Jahnke, R. Shoemaker, P. Dussault and K. W. Nickerson, “Quorum Sensing in the Dimorphic Fungus Candida albi- Copyright © 2011 SciRes. PP  Basic Research—Significance of Detection and Clinical Impact of Candida albicans in 359 Non-Immunosuppressed Patients cans Is Mediated by Farnesol,” Applied and Environmental Microbiology, Vol. 67, No. 7, 2001, pp. 2982-2992. doi:10.1128/AEM.67.7.2982-2992.2001 [22] D. H. Navarathna, K. W. Nickerson, G. E. Duhamel, T. R. Jerrels and T. M. Petro, “Exogenous Farnesol Interferes with the Normal Progression of Cytokine Expression dur- ing Candidiasis in a Mouse Model,” Infection and Immu- nity, 2007, Vol. 75, No. 8, pp. 4006-4011. doi:10.1128/IAI.00397-07 [23] C. Westwater, E. Balish and D. A. Schofield, “Candida albicans-Conditioned Medium Protects Yeast Cells from Oxidative Stress: A Possible Link between Quorum Sen- sing and Oxidative Stress Resistance,” Eukaryotic Cell, Vol. 4, No. 10, 2005, pp. 1654-1661. doi:10.1128/EC.4.10.1654-1661.2005 [24] A. Deveau, A. E. Piispanen, A. A. Jackson and D. A. Hogan, “Farnesol Induces Hydrogen Peroxide Resistance in Candida albicans Yeast by Inhibiting the Ras-Cyclic AMP Signaling Pathway,” Eukaryotic Cell, Vol. 9, No. 4, 2010, pp. 569-577. doi:10.1128/EC.00321-09 [25] D. H. Navarathna, J. M. Hornby, N. Hoerrmann, A. M. Parkhurst, G. E. Duhamel and K. W. Nickerson, “En- hanced Pathogenicity of Candida albicans Pre-Treated with Subinhibitory Concentrations of Fluconazole in a Mouse Model of Disseminated Candidiasis,” Journal of Antimicrobial Chemotherapy, Vol. 56, No. 6, 2005, pp. 1156-1159. doi:10.1093/jac/dki383 [26] D. H. Navarathna, J. M. Hornby, N. Krishnan, A. Park- hurst, G. E. Duhamel and K. W. Nickerson, “Effect of Farnesol on a Mouse Model of Systemic Candidiasis, Determined by Use of a DPP3 Knockout Mutant of Can- dida albicans,” Infection and Immunity, Vol. 75, No. 4, 2007, pp. 1609-1618. [27] Y. Y. Cao, Y. B. Cao, Z. Xu, K. Ying, Y. Li, Y. Xie, Z. Y. Zhu, W. S. Chen and Y. Y. Jiang, “cDNA Microarray Ana- lysis of Differential Gene Expression in Candida albicans Biofilm Exposed to Farnesol,” Antimicrobial Agents and Chemotherapy, Vol. 49, No. 2, 2005, pp. 584-589. doi:10.1128/AAC.49.2.584-589.2005 [28] J. M. Hornby and K. W. Nickerson, “Enhanced Produc- tion of Farnesol by Candida albicans Treated with Four Azoles,” Antimicrobial Agents and Chemotherapy, Vol. 48, No. 6, 2004, pp. 2305-2307. doi:10.1128/AAC.48.6.2305-2307.2004 [29] S. Abe, R. Tsunashima, R. Iijima, T. Yamada, N. Maru- yama, T. Hisajima, Y. Abe, H. Oshima and M. Yamazaki, “Suppression of Anti-Candida Activity of Macrophages by a Quorum-Sensing Molecule, Farnesol, through Induc- tion of Oxidative Stress,” Microbiology and Immunology, Vol. 53, No. 6, 2009, pp. 323-330. doi:10.1111/j.1348-0421.2009.00128.x [30] M. A. Scheper, M. E. Shirtliff, T. F. Meiller, B. M. Peters and M. A. Jabra-Rizk, “Farnesol, a Fungal Quorum-Sen- sing Molecule Triggers Apoptosis in Human Oral Squa- mous Carcinoma Cells,” Neoplasia, Vol. 10, No. 9, 2008, pp. 954-963. [31] R. Dumitru, J. M. Hornby and K. W. Nickerson, “Defined Anaerobic Growth Medium for Studying Candida albi- cans Basic Biology and Resistance to Eight Antifungal Drugs,” Antimicrobial Agents and Chemotherapy, Vol. 48, No. 7, 2004, pp. 2350-2354. doi:10.1128/AAC.48.7.2350-2354.2004 [32] T. Hisajima, N. Maruyama, Y. Tanabe, H. Ishibashi, T. Yamada, K. Makimura, Y. Nishiyama, K. Funakoshi, H. Oshima and S. Abe, “Protective Effects of Farnesol against Oral Candidiasis in Mice,” Microbiology and Im- munology, Vol. 52, No. 7, 2008, pp. 327-333. doi:10.1111/j.1348-0421.2008.00044.x [33] T. M. Weissenbacher, S. S. Witkin, A. Gingelmaier, C. Scholz, K. Friese and I. Mylonas, “Relationship between Recurrent Vuvovaginal Candidosis and Immune Media- tors in Vaginal Fluid,” European Journal of Obstetrics & Gynecology and Reproductive Biology, Vol. 144, No. 1, 2009, pp. 59-63. doi:10.1016/j.ejogrb.2009.01.010 [34] S. M. Chabot, T. S. Chernin, M. Shawi, J. Wagner, S. Farrant, D. S. Burt, C. Cyr and M. R. Neutra, “TLR2 Ac- tivation by Proteosomes Promotes Uptake of Particulate Vaccines at Mucosal Surfaces,” Vaccine, Vol. 25, No. 29, 2007, pp. 5348-5358. doi:10.1016/j.vaccine.2007.05.029 [35] M. R. Mainous, W. Ertel, I. H. Chaudry and E. A. Deitch, “The Gut: A Cytokine-Generating Organ in Systemic In- flammation?” Shock, Vol. 4, No. 3, 1995, pp. 193-199. doi:10.1097/00024382-199509000-00007 [36] E. Mavromanolakis, S. Maraki, A. Cranidis, Y. Tselentis, D. P. Kontoyiannis and G. Samonis, “The Impact of Nor- floxacin, Ciprofloxacin and Ofloxacin on Human Gut Colonization by Candida albicans,” Scandinavian Journal of Infectious Diseases, Vol. 33, No. 6, 2001, pp. 477-478. doi:10.1080/00365540152030006 [37] G. Samonis, H. Anastassiadou, M. Dassiou, Y. Tselentis and G. P. Bodey, “Effects of Broad-Spectrum Antibiotics on Colonization of Gastrointestinal Tracts of Mice by Candida albicans,” Antimicrobial Agents and Chemo- therapy, Vol. 38, No. 3, 1994, pp. 602-603. [38] A. Oberholzer, C. Oberholzer and L. L. Moldawer, “Sep- sis Syndromes: Understanding the Role of Innate and ac- quired Immunity,” Shock, Vol. 16, No. 2, 2001, pp. 83-96. doi:10.1097/00024382-200116020-00001 [39] R. S. Hotchkiss and I. E. Karl, “The Pathophysiology and Treatment of Sepsis,” The New England Journal of Medicine, Vol. 348, No. 2, 2003, pp. 138-150. doi:10.1056/NEJMra021333 [40] A. Katragkou, A. Chatzimoschou, M. Simitsopoulou, M. Dalakiouridou, E. Diza-Mataftsi, C. Tsantali and E. Roilides, “Differential Activities of Newer Antifungal Agents against Candida albicans and Candida parapsilo- sis Biofilms,” Antimicrobial Agents and Chemotherapy, Vol. 52, No. 1, 2008, pp. 357-360. doi:10.1128/AAC.00856-07 [41] R. T. Wheeler and G. R. Fink, “A Drug-Sensitive Genetic Network Masks Fungi from the Immune System,” PLoS Pathogens, Vol. 2, No. 4, 2006, p. e35. www.10.1371/journal.ppat.0020035 [42] A. C. Reboli, C. Rotstein, P. G. Pappas, S. W. Chapman, Copyright © 2011 SciRes. PP  Basic Research—Significance of Detection and Clinical Impact of Candida albicans in Non-Immunosuppressed Patients Copyright © 2011 SciRes. PP 360 D. H. Kett, D. Kumar, R. Betts, M. Wible, B. P. Gold- stein, J. Schranz, D. S. Krause and T. J. Walsh, “Anidu- lafungin versus Fluconazole for Invasive Candidiasis,” The New England Journal of Medicine, Vol. 356, No. 24, 2007, pp. 2472-2482. doi:10.1056/NEJMoa066906 Abbreviations CARS Compensatory anti-inflammatory response syn- drome GOLD Global Initiative for Chronic Obstructive Lung Disease ICU Intensive care unit Ig Immunoglobulin IL Interleukin IFN Interferon CFU Colony forming units LPS Lipopolysaccharide MARS Mixed anti-inflammatory response syndrome TGF Tumour growth factor Th T helper cells TLR Toll like receptor TNF Tumour necrosis factor
|