International Journal of Clinical Medicine
Vol.1 No.2(2010), Article ID:3259,3 pages DOI:10.4236/ijcm.2010.12014
Another Example of Devastating Complication of Heparin-Induced Thrombocytopenia Post-Cardiac Surgery
![]()
Department of Anesthesia and Cardiac Surgery, SMBD Jewish General Hospital, McGill University, Montreal, Canada.
Email: {sgermain, jmorin, dhickey}@jgh.mcgill.ca, fbeique@ana.jgh.mcgill.ca
Received August 18th, 2010; revised September 2nd, 2010; accepted September 2nd, 2010.
Keywords: Danaparoid, Heparin-Induced Thrombocytopenia, Stroke, Emboli
ABSTRACT
We describe a patient who developed catastrophic consequences of heparin-induced thrombocytopenia (HIT) post cardiac surgery, for which she required reoperation using CPB. We also illustrate the impact of intraoperative transesophageal echocardiography (TEE) in the surgical management of this patient.
1. Summary
In 2004, a 51-year-old woman underwent coronary artery bypass grafting surgery complicated by heparin-induced thrombocytopenia with thrombosis 9 days post operatively. Because this patient was already anticoagulated with danaparoid, the decision was made to use this anticoagulant during cardiopulmonary bypass for extraction of thrombi from both atria and pulmonary arteries. Clots were observed in the surgical field despite recommended dosing. Post-operatively, this patient exhibited excessive bleeding requiring massive transfusion and suffered from a stroke. Failure of danaparoid anticoagulation in our patient reinforces the need for an alternative anticoagulant.
2. Case Presentation
In 2004, a 51-year-old woman developed crescendo angina for which she was treated with unfractioned heparin (UFH). She underwent uncomplicated coronary artery bypass grafting (CABG) surgery. She was re-admitted nine days after her CABG with dyspnea and hypoxemia, where she was started on UFH for a suspected pulmonary embolus (PE). A complete blood count revealed a hemoglobin of 90 g/L and a platelet count of 42 000/l. Transthoracic echocardiogram (TTE) illustrated a large RA (right atrium) thrombus measuring 6×2 cm floating in and out of the right ventricle (RV) as seen in Figure 1. A spiral CT of the chest revealed massive emboli in the right and left pulmonary arteries. A clinical diagnosis of heparin-induced thrombocytopenia with thrombosis (HITT) was made. All heparin containing substances were discontinued, and the patient was anticoagulated with danaparoid (2250 U bolus, followed by 400 U/hr) the patient was then referred to cardiac surgery for removal of a right atrial thrombus and pulmonary embolectomy. Because the patient was already anticoagulated with danaparoid, the decision was made to use this anticoagulant during cardiopulmonary bypass (CPB). Therefore a bolus of danaparoid 3000 u was administered before CPB and the infusion was continued until separation from CPB. Arrangements were made with the hematologist and the laboratory to get urgent anti-Xa levels intra-operatively, in order to appropriately adjust the danaparoid levels. An additional bolus of danaparoid 1500 U was administered because visible clots were observed in the surgical field during CPB. Aprotinin was given in the hopes of minimizing post-operative bleeding as previously described in patients receiving danaparoid during cardiac surgery, though its efficacy is unproven in this setting [1].
3. Method
Intra-operative TEE was performed, and showed a left atrial (LA) thrombus, in addition to the RA thrombus visualized on the preoperative TEE. Although there was no report of a thrombus in the left atrium with TTE, a review of the echocardiographic study that was previously performed revealed a small clot in the LA. Under
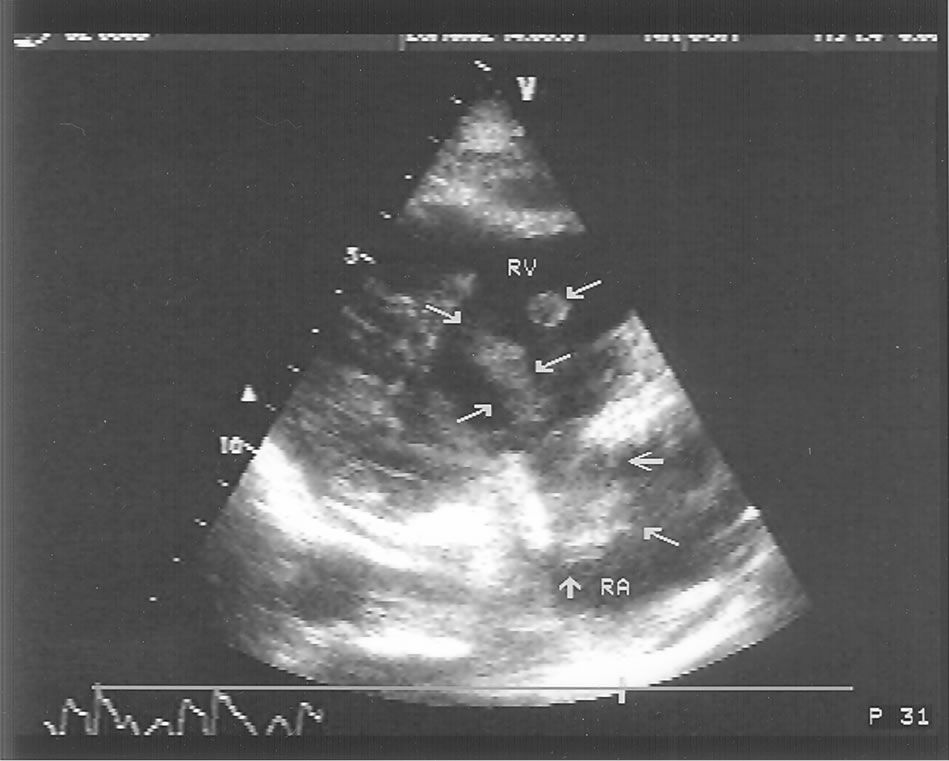
Figure 1. Transgastric right ventricular inflow view. Note arrows indicating thrombi in both the right atrium (RA) and right ventricle (RV)
full CPB, the RA and LA thrombi were excised, and the patient underwent bilateral pulmonary embolectomy. Intraoperatively, she required 7 U PRBC’s, 12 U platelets, and 4 U FFP’s. In the Intensive Care, the patient was titrated off pressor and inotropic support 2 days postoperatively. She received 3 more U PRBCs, 8 U FFPs, and 10 U cryoprecipitate. Chest tube drainage totaled 2900 ml in the first 24 hours. The patient was on continuous veno-veno hemofiltration (CVVH) for 12 hours post-operatively based on the assumption that it may enhance elimination of danaparoid and decrease postoperative bleeding. Two days later, the patient was noted to have developed dense left hemiparesis. A CT of the head revealed a right temporo-parietal infarct with mild right parietal hemorrhagic transformation and mass effect on the right ventricle. Her weakness improved gradually with physiotherapy, and she was discharged to Rehabilitation on Coumadin and Entrophen.
4. Discussion
The largest study reported results of 47 patients with HIT given danaparoid for cardiac surgery [1]. In two patients, surgery was abandoned because significant clots were observed in the operative field or the CPB circuit. In another 16 patients, further danaparoid doses had to be given because of clots in the field. Severe bleeding was observed in 22% of patients (requiring > 20 u of blood products) and 38% of patients required re-exploration for excessive post-operative bleeding. At 6 week follow-up, 77% of patients were still alive. As a result of both persistent thrombosis despite “appropriate” dosage, and increased bleeding, lack of reliable assay for intra-operative use and its long t1/2, danaparoid is a poor option for patients with HIT II undergoing CPB. Although danaparoid is still available in Canada and continental Europe, it has been removed form the US market in April 2002.
There are also several reports of Bivalirudin successful use for CPB in patients with HIT II [2-4]. Bivalirudin's short t1/2, significant organ independent elimination, and possibly its titratibility to the ACT, makes result in it a being an extremely better option for treatment of patients with HIT II undergoing CPB.
Our patient had already been started on danaparoid by the intensivist as soon as the suspicion of HIT II was entertained. Given its long t1/2, and the complexity of dosing another anticoagulant with danaparoid already on board, we decided to continue the use of danaparoid for CPB.
The patient underwent pulmonary embolectomy, and removal of RA, RV and LA thrombus. The intraoperative TEE can confirm pre-operative findings while ensuring that there are no new thrombi. Post cardiopulmonary bypass, the intraoperative TEE can also be used to confirm that there are no residual thrombi.
5. Results
Two days after her surgery, the patient developed dense left hemiparesis. This complication may have occurred as an embolic phenomenon from an intra-cardiac thrombus. Cross reactivity of danaproid with HIT antibodies may have also occurred, resulting in arterial thrombosis. Lastly, there have been speculations with regards to the danger of using aprotinin in patients with HIT II considering their degree of thrombogenicity [1].
This case report illustrates yet another example that danaparoid is a sub-optimal choice for anticoagulation in patients with HIT II whereby clots were observed in the surgical field despite recommended dosing. In addition, the patient exhibited excessive bleeding requiring massive transfusion, and suffered from a stroke post-operatively. Failure of danaparoid anticoagulation in our patient reinforces the need for an alternative anticoagulant and the establishment of a multidisciplinary, hospital-based protocol in patients with HIT II requiring urgent surgery. In our opinion, the use of bivalirudin represents the best non-heparin anticoagulant currently available for patients with HIT that require anticoagulant for both off-pump [5] and on-pump cardiac surgical cases. The use of intraoperative TEE is also recommended both to facilitate the hemodynamic management of these patients and to ensure that there are no new thrombi or residual thrombi at the end of surgery.
REFERENCES
- H. N Magnani, R. J. R. Beijering, J. W. Tencate, et al., “Orgaran Anticoagulation for Cardiopulmonary Bypass In Patients with Heparin-Induced Thrombocytopenia,” In: R. Pifarre, Ed., New Anticoagulants for the Cardiovascular Patients, Hanley & Belfus, Philadelphia 1997, pp. 487-500.
- G. Gordon, H. Rastegar, R. Schumann, et al., “Successful Use of Bivalirudin for Cardiopulmonary Bypass in a Patient with Heparin-Induced Thrombocytopenia,” Journal Cardiothoracic and Vascular Anesthesia, Vol. 17, 2003, pp. 632-635.
- A. Koster, B. Spiess and D. Chew, “Effectiveness of Bivalirudin as a Replacement for Heparin During Cardiopulmonary Bypass in Patients Undergoing Coronary Artery Bypass grafting,” American Journal of Cardiology, Vol. 93, 2004. pp. 356-359.
- A. Davis, R. Anderson, D. Short, et al., “Favourable Outcome with Bivalirudin Anticoagulation during Cardiopulmonary Bypass,” The Annals of Thoracic Surgery, Vol. 75, 2003, pp. 264-265.
- M. Carrier, D. Robitaille, L. Perrault, et al., “Heparin versus Danaparoid in Off-pump Coronary Bypass Grafting: Results of a Prospective Randomized Clinical Trial,” Journal of Thoracic Cardiovascular Surgery, Vol. 125, 2003, pp. 325-329.

