Open Journal of Psychiatry
Vol.2 No.4A(2012), Article ID:24719,4 pages DOI:10.4236/ojpsych.2012.224052
Simple schizophrenia revisited: Its schizophrenic body image deviation
![]()
1Tsukuba Institute for Biomedical Psychology, Tsukuba, Japan
2Saint-Pierre Hospital, Takasaki, Japan
3Faculty of Medicine, University of Tsukuba, Tsukuba, Japan
Email: ttn5aks258@mx6.ttcn.ne.jp
Received 26 September 2012; revised 24 October 2012; accepted 2 November 2012
Keywords: Simple Schizophrenia; Rorschach Test; Body Image Deviation; Diagnosis; Early Intervention
ABSTRACT
Simple schizophrenia has not yet been recognized as a well-established diagnostic category as one of the subtypes of schizophrenia, however, its inclusion to the official diagnostic system is regarded as urgent for early intervention. Here, we report our new observation that body image distortion uniquely found in typical schizophrenia, as reflected in the perception of mass of flesh of living objects in the whole or part of the Rorschach stimuli (Koide et al., 2002), was shown in the patients conforming to the original description of simple schizophrenia, to revisit its relatedness to schizophrenia from a cognitive and perceptual point of view. The Rorschach test was administered to four inpatients of a local mental hospital, showing social and occupational decline, negative symptoms and absence of positive symptoms. The presence or absence of Rorschach flesh mass body image percepts was examined. All of four patients revealed Rorschach mass of flesh responses. The fact that simple schizophrenia exhibited the same body image distortion in the flesh mass passive global perception with typical schizophrenia suggests the adequacy of reconsidering simple schizophrenia as a form of schizophrenia.
1. INTRODUCTION
There is a group of patients who show a gradual onset of pronounced negative symptoms, such as flattened affect and avolition, a reduced capacity for work and self-care, but never display prominent delusions, hallucinations, thought disorder, or catatonic symptoms. Simple schizophrenia was first conceptualized to include these patients by Diem in 1903 [1]. The concept was adopted by Bleuler [2] and Kraepelin [3], leading to be regarded as an added category to the existing subtypes of schizophrenia. It was adopted by major official psychiatric nosologies such as Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD). However, with the criticism that the conception was invalid [4-6], it was not included in DSM-III, DSM-IV and DSM-IV Text Revision (DSMIV-TR).
Recently the interest in simple schizophrenia has been revived by brain imaging studies [7-10], with neuropsychological studies [8,9], and by clinical studies by analysis of symptoms [11,12]. The family study reported its relatedness to typical schizophrenia [13]. In spite of criticism around the validity of the concept, there have been strong claims that simple schizophrenia should be reintroduced as subtype of schizophrenia [11,14]. In addition, recent reports of the effectiveness of novel-antipsychotic agents on these patients [15,16], as well as of the vital crises due to the reduced capacity for self-care of these patients by a general-medical provider [17], seem to make the reconsideration of the diagnosis of these patients important and urgent for early detection and early intervention.
In this study, we report that the patients meeting to the original conception of simple schizophrenia showed Rorschach percepts, a mass of flesh (flesh mass), reported as uniquely found in typical schizophrenia patients [18,19]. It was reported that schizophrenia patients produce Rorschach percepts implying a mass of flesh, and this unique perception was assumed to be related to the schizophrenic mass-like body image deviation. Two types of Rorschach flesh mass percepts were reported. In the direct and explicit form, flesh mass was referred as perceiving a mass of flesh or muscle of the creature. In the implicit form, it includes responses in which diminution (absence, unusual shortness, or vagueness) of arms, legs and head is mentioned. On the basis of the observation of flesh mass in simple schizophrenia, we would like to present an evidence for reconsideration for reintroduction of the concept, simple schizophrenia, as one form of schizophrenia, from a psychological point of view.
2. METHOD
2.1. Study Subjects
Four patients of the present study met the criteria for simple schizophrenia in ICD-10. They were inpatients of a psychiatric ward of a mental hospital when the Rorschach test was administered. Case A, a 18-year-old man, was brought to the hospital because of a suicidal attempt and violent behavior toward his mother. He had shown tic since his childhood, and spitting around and collecting rubbish since his early adolescence. Case B, a 23-year-old man, was brought to the hospital, because he threw away of the furniture in his home and attacked his father. He had a habit of spitting around. Case C, a 34-year-old woman, had shown severe mysophobia, as well as withdrawal since early adolescence. Case D, a 56-year-old man, was admitted to the hospital because of prominent irritability. He had a history of admission to the mental hospital several times. Several weeks before the present admission, he was prescribed anti-depressant drug under the diagnosis of depressive reaction to the succession of property, but it was not effective at all, made him more impatient and attacked a patient in the waiting room of the clinic. In all cases, novel antipsychotics (Riperidone for A, B and D, Olanzapine for C) prescribed after admission was effective on their problematic behaviors. The demographic data and symptoms of these cases are shown in Table 1. Informed consent was obtained from all cases.
2.2. Principal Measure
Principal measure of this study was Rorschach mass of flesh responses. The scoring (presence or absence of flesh mass) was conducted according to inclusion and exclusion criteria previously published [18,19]. First scoring was performed by one of the authors (YN) and was later confirmed by the other author (RK). All scoring was consistent among two raters.
In addition, existence of confabulation and contamination was examined. Also, the Exner Schizophrenia Index [20,21] was examined.
Scoring criteria for flesh mass perception is outlined below.
2.3. Schematic Drawing of Flesh Mass Scoring
The general scoring criteria of the flesh mass perception are summarized in Table 2.
Inclusion: There are two types of flesh mass; explicit and implicit. In their explicit form, (I-1) the flesh mass was referred directly as flesh mass or muscle, e.g. “a mass of flesh of some kind of an unspecified animal.”
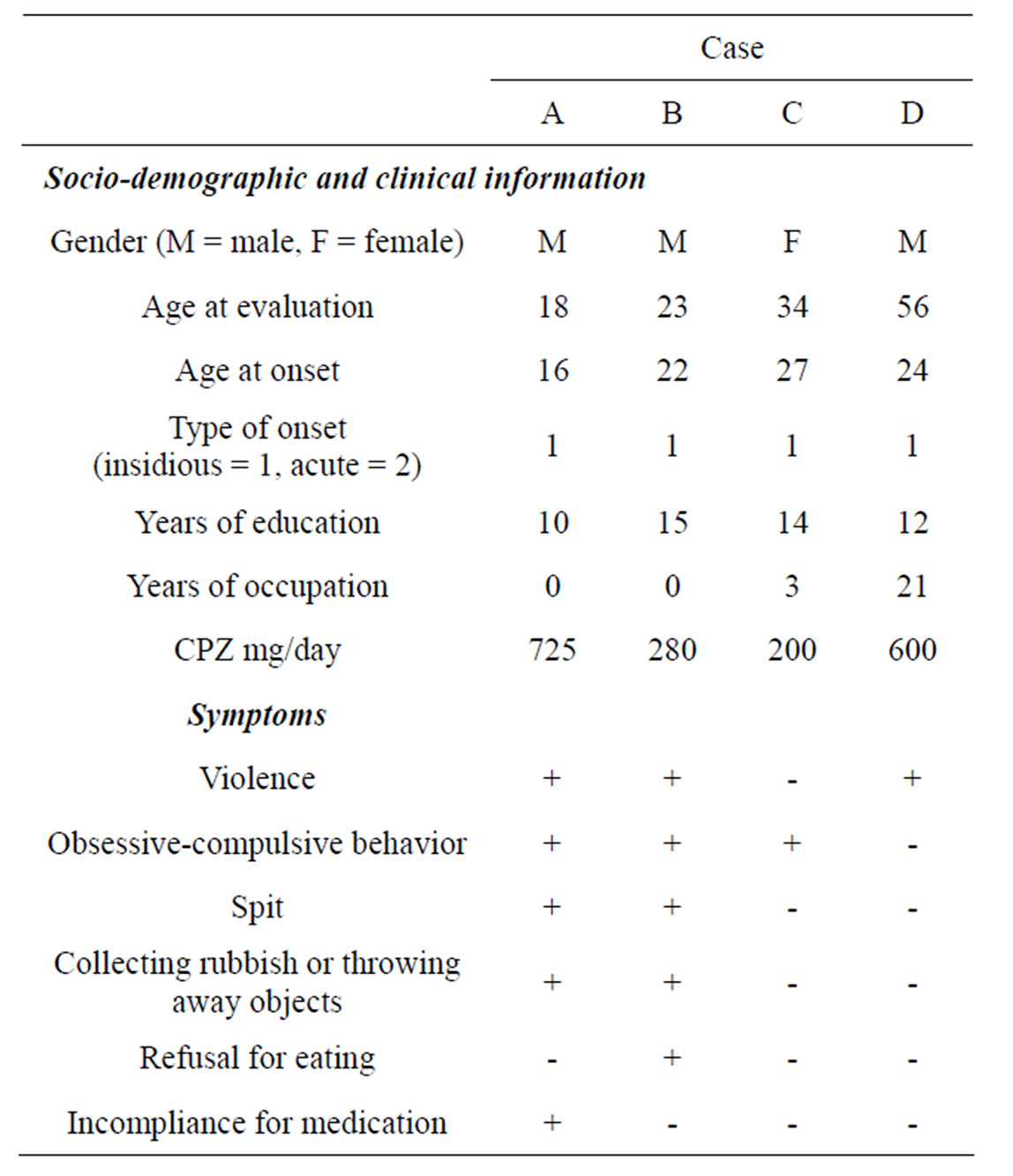
Table 1. Demopgraphic and clinical data of the study subjects.
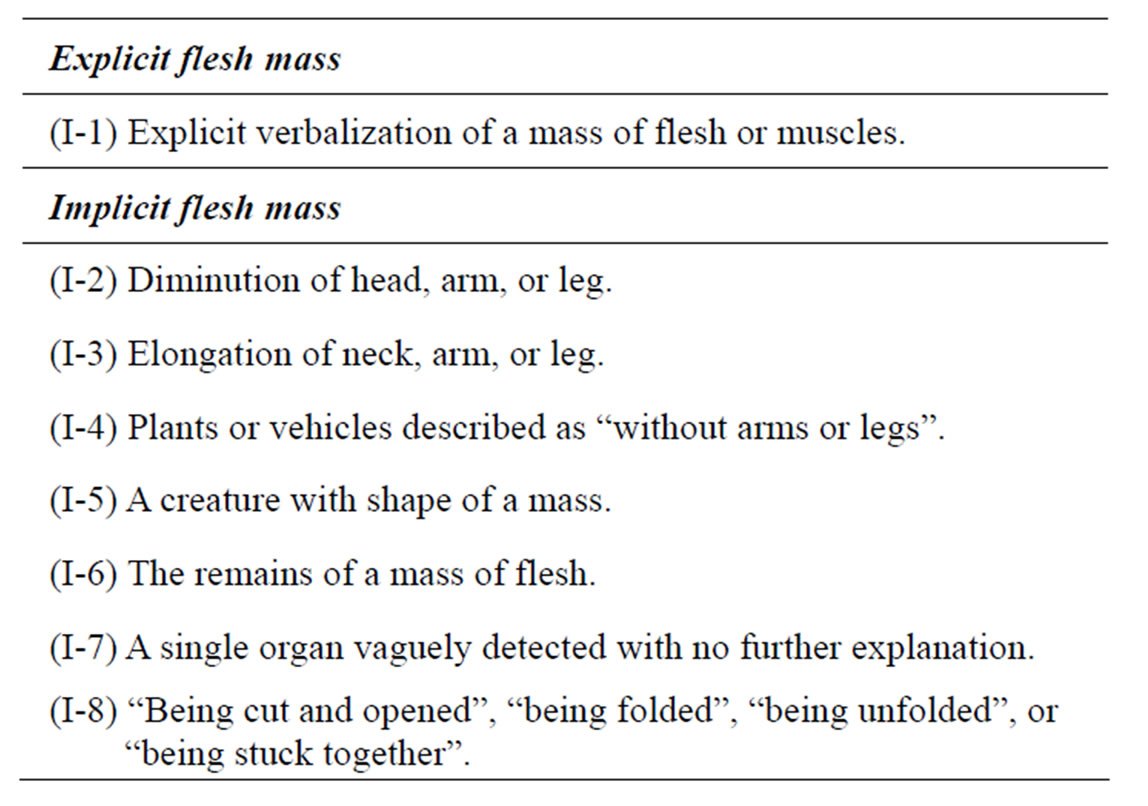
Table 2. Inclusion criteria of flesh mass perceptions.
The implicit forms of flesh mass percepts are the responses with the same implications in modified and indirect forms, (I-2) typically in the form of animals or human beings with diminution of head, leg, or arm. Also, implicit flesh mass includes (I-3) elongation of neck, leg or arm, (I-4) plants or vehicles described as “without arms or legs”, (I-5) a creature with the shape of a mass e.g. “a prawn, in this globular shape, with his back hunching up”, (I-6) the remains of a mass of flesh, (I-7) a single organ vaguely detected with no further explanation, and (I-8) responses referred as “being cut and opened”, “being folded”, “being unfolded” or “being stuck together”.
Exclusion: There is also a rule for exclusion. Perceptions of (E-1) underdeveloped animals or human beings, or animals that have intrinsically short arms or legs, without further explanation concerning diminution of arms or legs, are excluded. (E-2) Also, omissions of legs in the perceptions of human beings in the responses to Card VII are excluded, because these responses are quite common.
According to the previous report [18,19], 98% of 76 chronic schizophrenia, all 22 acute schizophrenia showed flesh mass perceptions, although 93% of 30 patients with anxiety disorders and none of the normal control subjects did not, suggesting that flesh mass scored based on this criteria was regarded as specific to schizophrenia. Precise details for this scoring should be referred to the previous study [18,19].
3. RESULTS
Rorschach flesh mass percepts were observed in all cases. The results are shown in Table 3. All of the flesh mass responses were in the category of indirect flesh mass. The flesh mass responses responded by the patients of the present study were: “a bone of a fish, the fish was slashed and opened in this way” (to card IV, by case 1), “legs, of some creature, nothing else” (to card IV, by case 2), “an insect, with irregularly long legs” (to card X, by case 2), “a fish, slashed up, with a center, its flesh in symmetry, with its fin and its tail” (to card VI, by case 3), “two sea horses being fixed together” (to card X, by case 3), and “viscera” (to card IV, by case 4).
Schizophrenic thought disorders, i.e. confabulation or contamination, was not shown in any of the patients. As to the Exner schizophrenia index, three of four patients provided small number of total responses (less than 10) so that it could not be calculated.
4. DISCUSSION
The present study showed the study patients disclosed the body image deviations reported as uniquely found in typical schizophrenia [18,19]. This suggests that simple schizophrenia, in this study, operationally defined according to ICD-10 provisionally, could be a candidate to be a subtype of schizophrenia.
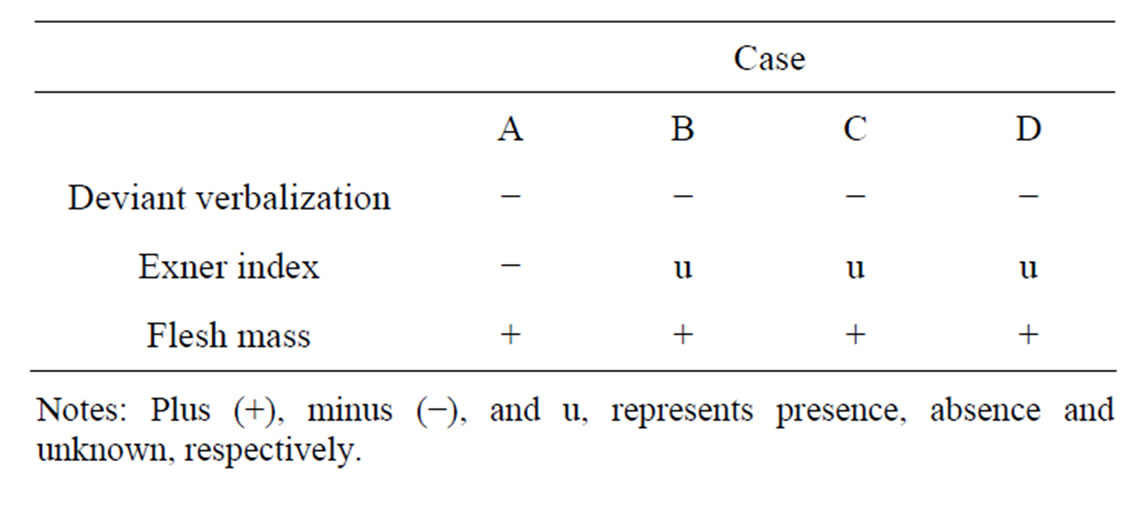
Table 3. Rorschach flesh mass responses of the study subjects.
Simple schizophrenia is a historical concept. It was introduced by Diem [1] and identified to be subtype of schizophrenia by Bleuler [2] and Kraepelin [3]. It was adopted in the diagnostic system in DSM-I and DSM-II and ICD. Although it is still maintained in ICD-10, it has been excluded from American official nosological categories since the publication of DSM-III and later. The main cause for this exclusion was its invalidity, princepally around the absence of psychotic symptoms. Presumed lack of delusion or hallucination was not considered to be enough to constitute diagnostic criteria.
However, the concept was claimed to be revived by clinical studies, by cluster analysis of symptoms [12], and a provisional criteria was proposed [11]. Recently, this concept was revisited from brain image studies along with neuropsychological studies, showing a gross parieto-occipital asymmetry [7], great ventricular subarachnoid space volumes [8], abnormalities affecting frontal and temporal regions on single photon emission computed tomography (SPECT) [9], homogeneous morphological and functional deficits in the prefrontal cortex [10], social skill impairment [8], general intellectual impairment and deficits in executive function and memory [9].
In addition, the development of psychopharmacological intervention, i.e. the introduction of novel-antipsychotic drugs, has made the claim for establishing the diagnosis as simple schizophrenia as a form of schizophrenia, with reports on effectiveness of these new agents on these patients [15,16]. Also, the lack of selfcare of these patients, just as shown by schizophrenia patients, was cautioned for inviting vital crisis, from the standpoint of general medical provider [17].
It is now in condition that accurate but practical evidence for making diagnosis is required for early intervention, beyond the presumption of absence or existence of psychotic symptoms. Evidence for reconsideration on this problem should be accumulated from a variety of domains, including psychological perspective. If a psychological task can detect the passivity in these patient, the core of negative symptoms, in the cognitive domain, regardless of their intention to be tested, i.e. regardless of their motivation for the completion of the task, it would be a more accurate indicator for making diagnosis than denying the presence of psychotic symptoms on the basis of the patients’ self-reports. However, the most psychological tests clinically employed require the fully pulledup motivation for the task in the examinee to be analyzed, so that these tasks could not be useful for inclusion of these patients in the appropriate diagnostic criteria, as far as their core symptom is “passivity”. Instead of “reaction time” adopted in intelligence scale or prevailed attention scale, more global cognitive tests which can detect passive cognitive trends without any control of internal attitude (set) of the patients are basically required to present an evidence for diagnosis. The Rorschach flesh mass percept would be one of such indexes, although the fully cautious observations by the trained examiners should be required for the scoring.
This index was originally devised to grasp the body image uniquely observed in schizophrenia [18,19]. Body image would be a frame of reference to which the individuals refer in all perception and cognition. The fact that the body image deviation as reflected in flesh mass percepts was shared with the patients meeting to ICD-10 simple schizophrenia criteria and typical schizophrenia would suggests that these patients should be regarded as one form of schizophrenia.
As a conclusion, simple schizophrenia (meeting to ICD-10 criteria) showed Rorschach flesh mass percepts reported as being unique to schizophrenia, reflecting their schizophrenic body image deviation. It would be one of the evidence to reconsider the concept of simple schizophrenia as a form of schizophrenia.
5. ACKNOWLEDGEMENTS
We appreciate Dr. Manabu Yamazaki, the president of Saint-Pierre Hospital. We also appreciate Dr. Satoshi Tsuruta of Saint-Pierre Hospital for his cooperation.
REFERENCES
- Diem, O. (1903) Die einfach demente form der dementia praecox (dementia simplex). Archiv für Psychiatrie und Nervenkrankheiten, 37, 111-187. doi:10.1007/BF02227700
- Bleuler, E. (1911) Dementia praecox, or the group of schiozophrenias. Zinkin, J., Translated, International Universities Press, New York, 1950.
- Kraepelin, E. (1919) Dementia praecox and paraphrenia. In: Textbook of Psychiatry, 8th Edition. Barclay, E.S., Translated, Livingston, Edinburgh.
- Lewis, N.D.C. (1936) Research in dementia praecox (past attainments, present trends, and future possibilities). Committee on Mental Hygiene, 27, 842-843.
- Kant, O. (1948) Clinical investigation of simple schizophrenia. Psychiatric Quarterly, 17, 141-151. doi:10.1007/BF01572410
- Stone, A.A., Hopkins, R., Mahnke, M.W., Shapiro, D.W. and Silverglate, H.A. (1968) Simple schizophrenia-syndrome or shibboleth. The American Journal of Psychiatry, 125, 61-68.
- Maj, M., Galderisi, S., Conforti, R. and D’Amato, A.C. (1995) Gross reversal of brain parieto-occipital asymmetry in a case of DSM IV simple schizophrenia. Schizophrenia Research, 14, 265-266.
- Galderisi, S., Bucci, P., Mucci, A., D’Amato, A.C., Conforti, R. and Maj, M. (1999) “Simple schizophrenia”: A controlled MRI and clinical/neuropsychological study. Psychiatry Research: Neuroimaging, 91,175-184. doi:10.1016/S0925-4927(99)00026-8
- Serra-Mestres, J., Gregory, C.A., Tandon, S., Stansfield, A.J., Kemp, P.M. and McKenna, P.J. (2000) Simple schizophrenia revisited: A clinical, neurolopsychological, and neuroimaging analysis of nine cases. Schizophrenia Bulletin, 26, 479-493. doi:10.1093/oxfordjournals.schbul.a033467
- Suzuki, M., Nohara, S., Hagino, H., Takahashi, T., Kawasaki, Y., Yamashita, I., Watyanabr, N., Seto, H. and Kurachi, M. (2005) Prefrontal abnormalities in patients with simple schizophrenia: structural and functional brainimaging studies in five cases. Psychiatry Research: Neuroimaging, 140,157-171. doi:10.1016/j.pscychresns.2005.06.005
- Black, D.W. and Boffeli, T.J. (1989) Simple schizophrenia: Past, present, and future. The American Journal of Psychiatry, 146, 1267-1273.
- Dollfus, S., Everitt, B., Ribeyre, J.M., Assouly-Besse, F., Sharp, C. and Petit, M. (1996) Identifying subtypes of schizophrenia by cluster analyses. Schizophrenia Bulletin, 22, 545-555. doi:10.1093/schbul/22.3.545
- Kendler, K.S., McGuire, M., Gruenberg, A.M. and Walsh, D. (1994) An epidemiologic, clinical, and family study of simple schizophrenia in county Roscommon, Ireland. The American Journal of Psychiatry, 151, 27-34.
- McGlashan, T.H. and Fenton, W.S. (1991) Classical subtypes for schizophrenia: literature review for DSM-IV. Schizophrenia Bulletin, 17, 609-632.
- Sekine, Y., Taei, N., Iyo, M., Mori, N., Minami, M. and Ohta T. (2001) Effective risperidone treatment for simple deteriorative disorder (simple schizophrenia): A case report. Schizophrenia Research, 50, 213-214. doi:10.1016/S0920-9964(00)00049-9
- Rollnik, J.D., Schneider, U. and Emrich, H.M. (2001) Erfolgreiche Behandlung einer Schizophrenia simplex mit atypischen Neuroleptika (Clozapin, Risperidon). Der Nervenartzt, 72, 380-383. doi:10.1007/s001150050768
- Moini, B. and Levenson, J.L.(2009) A forgotten diagnosis: Simple schizophrenia in a patient with breast cancer. Psychosomatics, 50, 87-89. doi:10.1176/appi.psy.50.1.87
- Koide, R., Chien, C.P., Iizuka, S and Morita, N. (2002) A mass of flesh: schizophrenic Rorschach percepts. Comprehensive Psychiatry, 43, 474-477. doi:10.1053/comp.2002.34633
- Koide, R. and Tamaoka, A. (2008) Body image deviation in chronic schizophrenia. NOVA Biomedical, New York.
- Exner Jr., E.J. (1991) The Rorschach: A comprehensive system: Vol. 2. Current research and advanced interpretation. 2nd Edition, Wiley, New York.
- Exner Jr., E.J. (1993) The Rorschach: A comprehensive system: Vol. 1. Basic Foundations. 3rd Edition, Wiley, New York.

