Journal of Cosmetics, Dermatological Sciences and Applications
Vol.4 No.3(2014), Article ID:46505,6 pages
DOI:10.4236/jcdsa.2014.43025
Evaluation of Self-Treatment of Acne Using Silk’n Blue Phototherapy System
Judith Hellman*, Cielo A. Ramirez
Mt. Sinai Hospital, New York, USA
Email: *jhderm@gmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 15 April 2014; revised 12 May 2014; accepted 19 May 2014
ABSTRACT
Background: At-home phototherapy devices for the treatment of acne have emerged as an appealing treatment option and as an effective adjunct treatment to existing modalities. The principal goal of the study was to determine the changes in the number of inflammatory lesions in acne patients. Methods: Patients received instruction for daily at-home use of Silk’n Blue device for 12 weeks. Follow-up visits were conducted at 1 and 3 months to collect data. Results: Fifteen subjects with mild to severe cases experienced improvement over the course of the trial. The decrease in mean inflammatory acne counts (from 41.26 to 24.46) and mean percent reduction (41.8%) were statistically significant (p < 0.001). Some participants experienced percent reductions as great as 67%. No adverse events were recorded. Conclusions: The Silk’n Blue device is a safe and effective modality for at-home treatment of mild, moderate, and severe inflammatory acne vulgaris with proper use.
Keywords:Acne, Blue Light Therapy, LED Phototherapy

1. Introduction
Acne vulgaris affects 80% - 90% of people during their adolescence, and half continue to experience symptoms into adulthood [1] -[3] . The condition is moderate-to-severe in 15% - 20% of people in their late teens [4] . It is characterized by noninflammatory open or closed comedones, and by inflammatory papules, pustules, and cysts. Secondary scarring may also result. The disfigurement caused by severe acne and acne scars can have negative psychological and psychosocial effects [5] . These include stigmatization from peers, lower self-esteem, interpersonal difficulties, anxiety, depression, and higher unemployment rates [6] .
The treatment of acne is directed towards four known pathogenic factors. These are the plugging of the follicle, excess sebum production, the presence and activity of the bacteria Propionibacterium acnes (P. acnes), and inflammation of the skin [7] . Existing pharmacotherapeutic options are topical comedolytics, topical and systemic antibiotics, hormonal manipulations, and oral retinoids. Procedural treatments include manual extraction of comedones, intralesional steroid injections, and superficial glycolic or salicylic acid peels.
Despite a wide variety of treatment options, there is a growing demand among both patients and practitioners for fast, safe, and side-effect-free interventions [8] . Various forms of phototherapy with visible light have been shown to be effective in the treatment of acne vulgaris [9] . Treatments using light within the blue range have been found to be particularly effective in the selective destruction of P. acnes bacterium. The bacteria produce and store endogenous porphyrins, absorbing light energy at the near-UV and blue light spectrum [9] . Absorption of the appropriate wavelength of light energy causes the creation of a highly reactive free radical species leading to the destruction of the bacterial cell wall [10] . Infrared laser light selectively targets the dermal layer where sebaceous glands are located [8] . The heat from the absorbed energy creates thermal injury and alters the structure of the sebaceous glands. Reduction in size of sebaceous glands and sebum output also results in acne improvement.
The objective of this open-label study was to evaluate the safety, efficacy, and usage compliance of the FDAapproved Silk’n Blue system for the self-treatment of mild to severe acne. The primary goal of the study was to determine the changes in the number of inflammatory lesions.
2. Materials and Methods
2.1. Study Design
This study was a 12-week, open-label, prospective cohort study carried out in New York, NY, USA between June and October 2013. Patients were instructed to treat themselves at home daily for 12 weeks. Follow-up visits to evaluate the results were scheduled at 1 and 3 months following the last treatment. Each patient served as its own control by comparing the acne count at base-line to the follow-up results.
During the first visit, each patient received verbal instruction of treatment guidelines and was instructed on how to turn on the Silk’n Blue device and to hold the applicator against the skin. Patients were to hold the Blue applicator on the skin without moving the device for 3 minutes on a section of the affected area, repeating until the entire affected area had been treated. Treatment time could be increased to 5 minutes as tolerated per actively treated area.
Inflammatory lesion counts were conducted at baseline, at 1 month, and at 3 months, using individual lesion counts of the entire face, ranging from hairline to jawline. Standardized digital photographs were taken at all three visits. A subject questionnaire on response to treatment and discomfort was completed at each follow-up visit.
2.2. Subjects
Written informed consent was obtained from all subjects prior to enrollment. Fifteen participants aged 17 - 31 years with Fitzpatrick skin types I-VI (12 women and 3 men) were enrolled. Mild acne was graded as the presence of a small number of inflammatory papules. Moderate acne was graded as a greater number of papules, pustules, and some inflammatory cysts. Severe acne was characterized by a greater number of papules, pustules, and inflammatory cysts, as well as the presence of inflamed acne scars.
The inclusion criterion for participants was the presence of persistent inflammatory acne. Patients were allowed to continue using prescribed topical acne treatments. Participants were required to refrain from using systemic oral treatments or undergoing laser treatments during this period of time or the 6 months preceding participation in this clinical trial.
2.3. Light Source
The Silk’n Blue (Home Skinovations, Yokneam, Israel) is a rechargeable hand-held device for patient-controlled application of blue light therapy and an infrared heating. An array of 24 LEDs produces blue-violet light of wavelengths in the 405 - 460 nm range. The light is emitted in a uniform distribution to avoid hot spots. A proximity sensor causes the lights to turn on only with skin contact to the light head. The device features a temperature sensor that turns the device off when the skin temperature reaches 41˚C to prevent overheating of the skin.
2.4. Statistics
One-tailed student’s t tests were used to determine the statistical significance for a non-normal distribution with large variation.
3. Results
3.1. Acne Counts
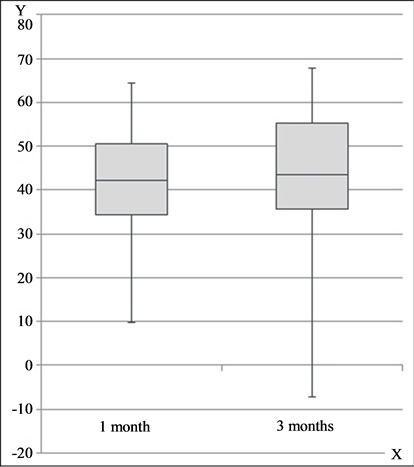
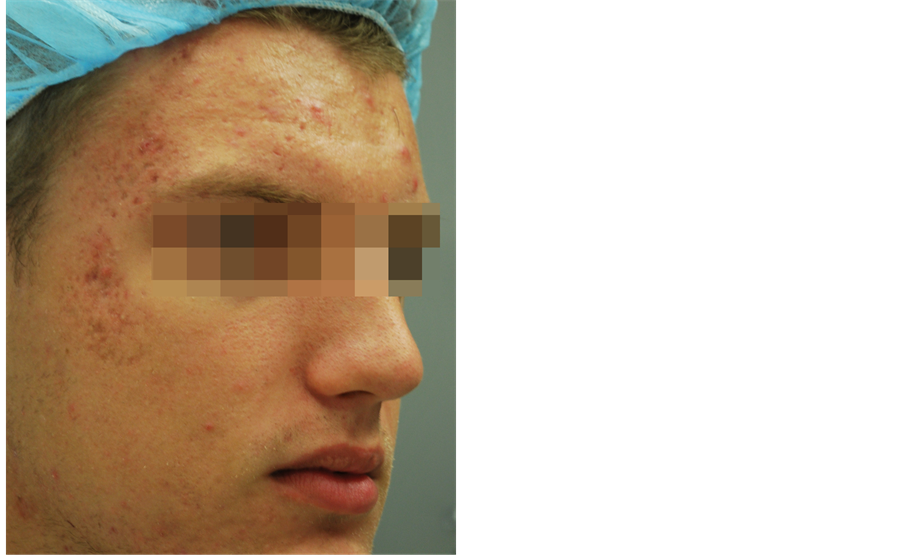
Inflammatory lesion counts were significantly reduced by blue light LED treatments after one month of treatment (41.7% reduction, from a mean of 40.26 to 26.33, p < 0.001) (see Figure 1(a) and Figure 1(b)). The greatest decrease occurred during the first month, and this significant improvement was sustained over the course of the study. At 3 months, the mean percent reduction from baseline was 41.8% (from a mean of 41.26 to 24.46, p < 0.001). Representative clinical photographs are shown in Figure 2(a) and Figure 2(b).
At 3 months, fourteen of the fifteen participants showed a decrease in total lesions from baseline. Two participants experienced percent reductions in inflammatory lesions of 61% and 67%. Eleven patients experienced further improvement after the first month of treatment. Three participants experienced an increased lesion count after the first month, and one patient returned to baseline results at 3 months. These results demonstrate shortterm efficacy in the reduction of lesions for all participants and a long-term maintenance of improved outcomes for the majority of patients with continued use.
3.2. Patient Subjective Assessment
The subjective surveys elicited some important information. Two participants of Fitzpatrick skin type IV experienced slight pain and tenderness for 10 - 15 minutes after treatments. In both cases, these symptoms subsided after one week of continued use. Eight subjects reported that they “liked” the device and found it to be effective. Four subjects said that they “loved” the treatment system and expressed a commitment to continued use. Only one participant did not see noticeable improvement and stopped consistent use of the device after breaking out during the fourth week of the trial. Four participants expressed some difficulty in maintaining a consistent schedule, but reported that they were overall pleased with the results.
 (a)
(a)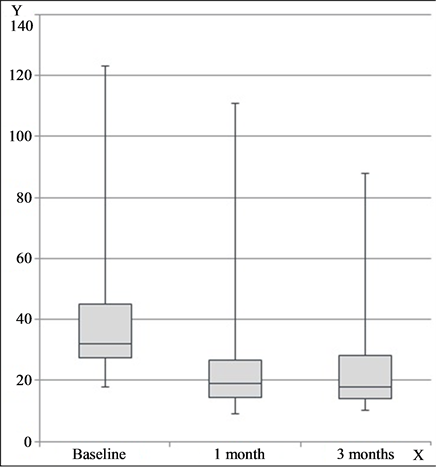 (b)
(b)
Figure 1. (a) Inflammatory acne lesion counts; (b) Percent improvement in lesion count. X = time, Y = lesion count (a); % improvement (b).
Clinical Photographs
 (a)
(a)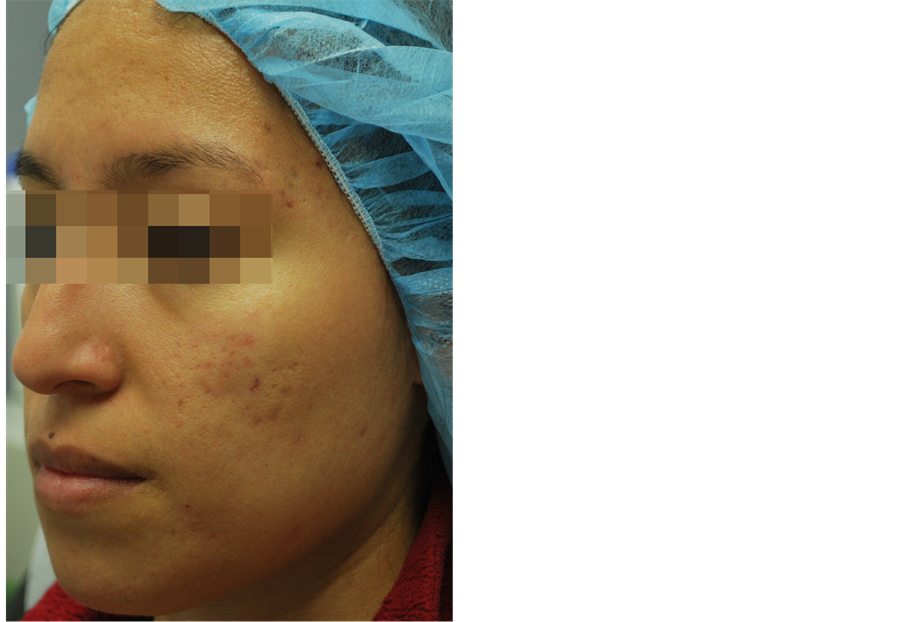 (b)
(b)
Figure 2. (a) Male, 19 yo, Fitzpatrick skin type II. Left: baseline, right: 3 months follow-up; (b) Female, 24 yo, Fitzpatrick skin type IV. Left: baseline, right: 3 months follow-up.
4. Discussion
Inflammatory lesions counts decreased for all participants during the first month. The majority of participants were significantly satisfied with their overall trend towards clearer skin. They found that they were able to maintain and improve upon the progress that they had made into the third month of treatment. Four of the 15 participants experienced an increase in lesions after 4 weeks, which may be explained by a decrease in novelty and motivation to uphold usage compliance as directed. Nearly all patients stated that integrating the Silk’n Blue treatment system into their daily routine had been a worthy use of their time and efforts.
This is the second open-label study investigating the safety and efficacy of the Silk’n Blue device [11] . This trial evaluated the device’s at-home efficacy in reducing inflammatory lesion counts for a sample group with greater variation in acne severity. The similarity in results between these two trials indicates that the Silk’n Blue system is suitable for patients who may prefer self-treatment or have decreased access to regular in-office treatments. The results of the present study support previous findings of blue and infrared light therapy as a suitable stand-alone treatment for Acne vulgaris. This light therapy may be as, if not more, effective in combined use with modalities that only a doctor can provide a patient.
Related studies have found that devices that use a combination of red and blue light are similarly effective in decreasing the amount of P. acnes and inflammation in treated skin [12] . Red light can penetrate to the level of the sebaceous glands and may have anti-inflammatory properties related to cytokine release from macrophages [9] . A comparative study between the effectiveness of blue light therapy versus combination blue-red light therapy is our recommendation for further research in this field.
5. Conclusion
The results of this study suggest that the Silk’n Blue device may be a safe and effective blue and infrared light therapy for at-home treatment of mild, moderate, and severe inflammatory acne. Further study of the safety and efficacy of combined blue and infrared light therapy systems is required for the treatment of different acne symptoms in a larger set of patients with longer follow-up periods.
References
- Yentzer, B.A., Hick, J., Reese, E.L., Uhas, A., Feldman, S.R. and Balkrishnan, R. (2010) Acne Vulgaris in the United States: A Descriptive Epidemiology. Cutis, 86, 94-99.
- Law, M.P., Chuh, A.A., Lee, A. and Molinari, N. (2010) Acne Prevalence and Beyond: Acne Disability and Its Predictive Factors among Chinese Late Adolescents in Hong Kong. Clinical and Experimental Dermatology, 35, 16-21. http://dx.doi.org/10.1111/j.1365-2230.2009.03340.x
- Yahya, H. (2009) Acne Vulgaris in Nigerian Adolescents—Prevalence, Severity, Beliefs, Perceptions, and Practices. International Journal of Dermatology, 48, 498-505. http://dx.doi.org/10.1111/j.1365-4632.2009.03922.x
- Bhate, K. and Williams, H.C. (2013) Epidemiology of Acne Vulgaris. British Journal of Dermatology, 168, 474-485. http://dx.doi.org/10.1111/bjd.12149
- Niemeier, V., Kupfer, J. and Gieler, U. (2006) Acne Vulgaris—Psychosomatic Aspects. Journal der Deutschen Dermatologischen Gesellschaft, 4, 1027-1036. http://dx.doi.org/10.1111/j.1610-0387.2006.06110.x
- Mulder, M.M., Sigurdsson, V., van Zuuren, E.J., Klaassen, E.J., Faber, J.A., de Wit, J.B. and van Vloten, W.A. (2001) Psychosocial Impact of Acne Vulgaris. Evaluation of the Relation between a Change in Clinical Acne Severity and Psychosocial State. Dermatology, 203, 124-130. http://dx.doi.org/10.1159/000051726
- Harper, J.C. (2004) An Update on the Pathogenesis and Management of Acne Vulgaris. Journal of the American Academy of Dermatology, 51, S36-S38. http://dx.doi.org/10.1016/j.jaad.2004.01.023
- Elman, M. and Lebzelter, J. (2004) Light Therapy in the Treatment of Acne Vulgaris. Dermatologic Surgery, 30, 139- 146. http://dx.doi.org/10.1111/j.1524-4725.2004.30053.x
- Rai, R. and Natarajan, K. (2013) Laser and Light Based Treatments of Acne. Indian Journal of Dermatology, Venerology, and Leprology, 79, 300-309. http://dx.doi.org/10.4103/0378-6323.110755
- Melo, T.B. (1987) Uptake of Protoporphyrin and Violet Light Photodestruction of Propionibacterium Acnes. Zeitschrift für Naturforschung, 42, 123-128.
- Gold, M.H., Biron, J.A. and Sensing, W. (2013) Clinical and Usability Study to Determine the Safety and Efficacy of the Silk’n Blue Device for the Treatment of Mild to Moderate Inflammatory Acne Vulgaris. Journal of Cosmetic and Laser Therapy. http://dx.doi.org/10.3109/14764172.2013.854638
NOTES

*Corresponding author.

