H. KAKIZAKI ET AL.
Copyright © 2011 SciRes. SS
416
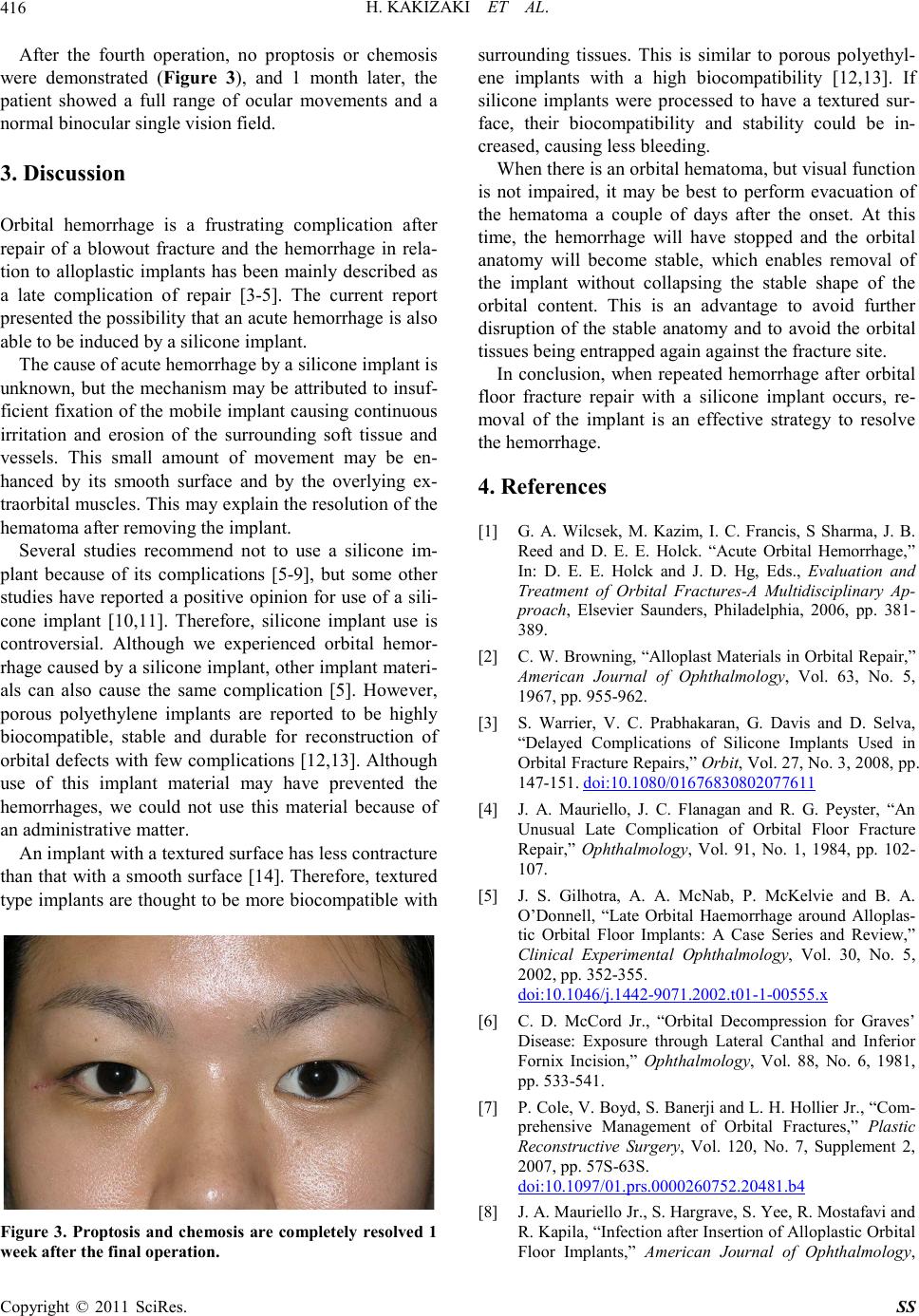
After the fourth operation, no proptosis or chemosis
were demonstrated (Figure 3), and 1 month later, the
patient showed a full range of ocular movements and a
normal binoc ular single visi on field.
3. Discussion
Orbital hemorrhage is a frustrating complication after
repair of a blowout fracture and the hemorrhage in rela-
tion to alloplastic implants has been mainly described as
a late complication of repair [3-5]. The current report
presented the possibility that an acute hemorrhage is also
able to be induced by a silicone implant.
The cause of acute hemorrhage by a silicone implant is
unknown, but the mec hanism may be attributed to insuf-
ficient fixation of the mobile implant causing continuous
irritation and erosion of the surrounding soft tissue and
vessels. This small amount of movement may be en-
hanced by its smooth surface and by the overlying ex-
traorbital muscles. This may explain the resolution of the
hematoma after removing the implant.
Several studies recommend not to use a silicone im-
plant because of its complications [5-9], but some other
studies have reported a positive opinion for use of a sili-
cone implant [10,11]. Therefore, silicone implant use is
controversial. Although we experienced orbital hemor-
rhage caused by a silicone implant, other implant materi-
als can also cause the same complication [5]. However,
porous polyethylene implants are reported to be highly
biocompatible, stable and durable for reconstruction of
orbital defects with few complications [12,13]. Although
use of this implant material may have prevented the
hemorrhages, we could not use this material because of
an administrative matter.
An implant with a textured surface has less contracture
than that with a smooth surface [14]. Therefore, textured
type implants are thought to be more biocompatible with
Figure 3. Proptosis and chemosis are completely resolved 1
week after the fin al operation.
surrounding tissues. This is similar to porous polyethyl-
ene implants with a high biocompatibility [12,13]. If
silicone implants were processed to have a textured sur-
face, their biocompatibility and stability could be in-
creased, causing less bleeding.
When there is an orbital hematoma, but visual function
is not impaired, it may be best to perform evacuation of
the hematoma a couple of days after the onset. At this
time, the hemorrhage will have stopped and the orbital
anatomy will become stable, which enables removal of
the implant without collapsing the stable shape of the
orbital content. This is an advantage to avoid further
disruption of the stable anatomy and to avoid the orbital
tissues being entrapped again against the fracture site.
In conclusion, when repeated hemorrhage after orbital
floor fracture repair with a silicone implant occurs, re-
moval of the implant is an effective strategy to resolve
the hemorrhage.
4. References
[1] G. A. Wilcsek, M. Kazim, I. C. Francis, S Sharma, J. B.
Reed and D. E. E. Holck. “Acute Orbital Hemorrhage,”
In: D. E. E. Holck and J. D. Hg, Eds., Evaluation and
Treatment of Orbital Fractures-A Multidisciplinary Ap-
proach, Elsevier Saunders, Philadelphia, 2006, pp. 381-
389.
[2] C. W. Browning, “Alloplast Materials in Orbital Repair,”
American Journal of Ophthalmology, Vol. 63, No. 5,
1967, pp. 9 55-962.
[3] S. Warrier, V. C. Prabhakaran, G. Davis and D. Selva,
“Delayed Complications of Silicone Implants Used in
Orbital Fracture Repairs,” Orbit, Vol. 27, No. 3, 2008, pp.
147-151. doi:10.1080/01676830802077611
[4] J. A. Mauriello, J. C. Flanagan and R. G. Peyster, “An
Unusual Late Complication of Orbital Floor Fracture
Repair,” Ophthalmology, Vol. 91, No. 1, 1984, pp. 102-
107.
[5] J. S. Gilhotra, A. A. McNab, P. McKelvie and B. A.
O’Donnell, “Late Orbital Haemorrhage around Alloplas-
tic Orbital Floor Implants: A Case Series and Review,”
Clinical Experimental Ophthalmology, Vol. 30, No. 5,
2002, pp. 352-355.
doi:10.1046/j.1442-9071.2002.t01-1-00555.x
[6] C. D. McCord Jr., “Orbital Decompression for Graves’
Disease: Exposure through Lateral Canthal and Inferior
Fornix Incision,” Ophthalmology, Vol. 88, No. 6, 1981,
pp. 533- 541 .
[7] P. Cole, V. Boyd, S. Banerji and L. H. Hollier Jr., “Com-
prehensive Management of Orbital Fractures,” Plastic
Reconstructive Surgery, Vol. 120, No. 7, Supplement 2,
2007, pp . 57S-63S.
do i:10. 1097/01.prs.000026 0752.20481.b4
[8] J. A. Mauriello Jr., S. Hargrave, S. Yee, R. Mostafavi and
R. Kapila, “Infection after Insertion of Alloplastic Orbital
Floor Implants,” American Journal of Ophthalmology,