364 M. KOPLAY ET AL.
Figure 1. US image shows the echogenic lesion in 7th seg-
ment of the liver (arrow).
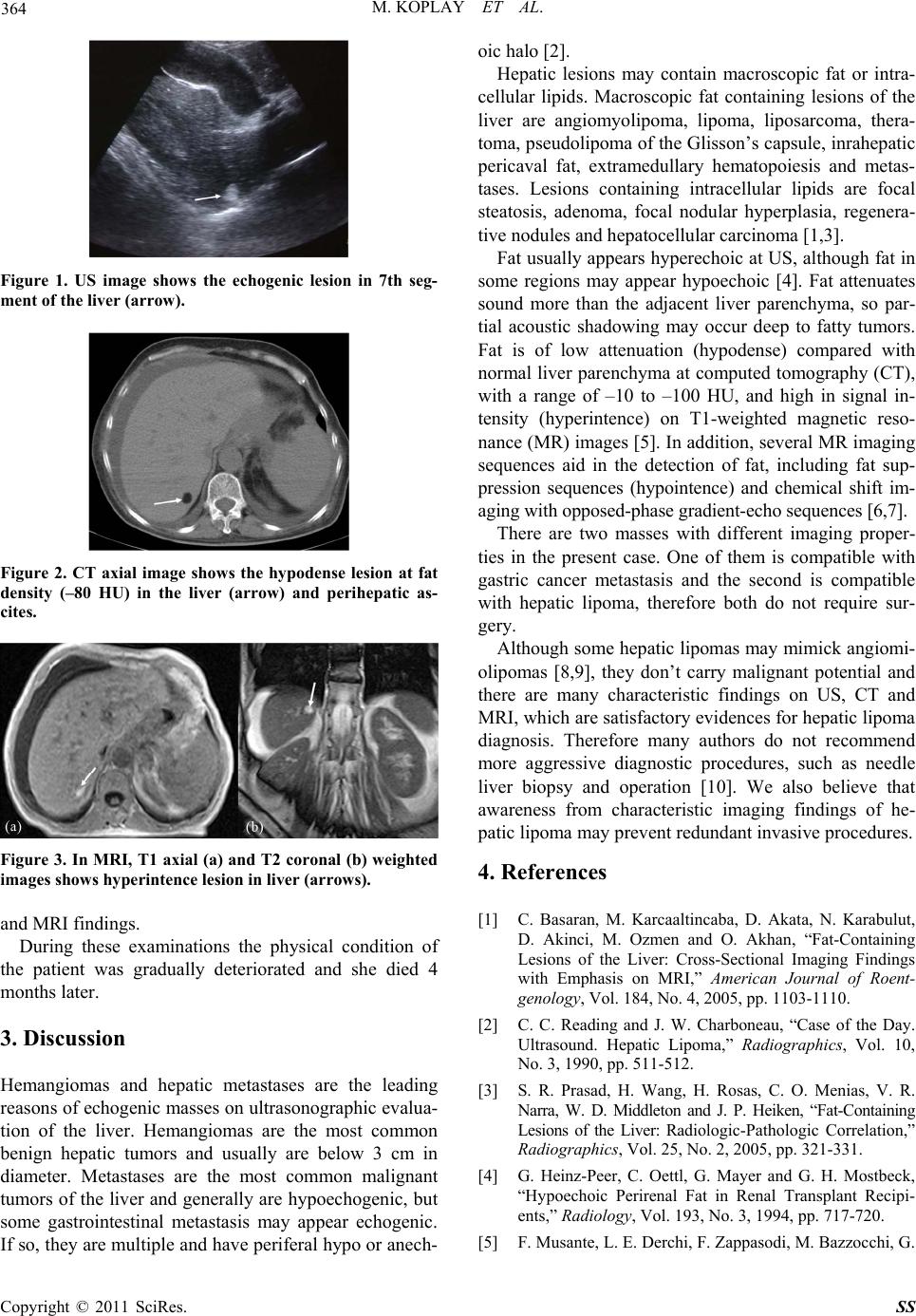
Figure 2. CT axial image shows the hypodense lesion at fat
density (–80 HU) in the liver (arrow) and perihepatic as-
cites.
Figure 3. In MRI, T1 axial (a) and T2 coronal (b) weighted
images shows hyperintence lesion in liver (arrows).
and MRI findings.
During these examinations the physical condition of
the patient was gradually deteriorated and she died 4
months later.
3. Discussion
Hemangiomas and hepatic metastases are the leading
reasons of echogenic masses on ultrasonographic evalua-
tion of the liver. Hemangiomas are the most common
benign hepatic tumors and usually are below 3 cm in
diameter. Metastases are the most common malignant
tumors of the liver and generally are hypoechogenic, but
some gastrointestinal metastasis may appear echogenic.
If so, they are multiple and have periferal hypo or anech-
oic halo [2].
Hepatic lesions may contain macroscopic fat or intra-
cellular lipids. Macroscopic fat containing lesions of the
liver are angiomyolipoma, lipoma, liposarcoma, thera-
toma, pseudolipoma of the Glisson’s capsule, inrahepatic
pericaval fat, extramedullary hematopoiesis and metas-
tases. Lesions containing intracellular lipids are focal
steatosis, adenoma, focal nodular hyperplasia, regenera-
tive nodules and hepatocellular carcinoma [1,3].
Fat usually appears hyperechoic at US, although fat in
some regions may appear hypoechoic [4]. Fat attenuates
sound more than the adjacent liver parenchyma, so par-
tial acoustic shadowing may occur deep to fatty tumors.
Fat is of low attenuation (hypodense) compared with
normal liver parenchyma at computed tomography (CT),
with a range of –10 to –100 HU, and high in signal in-
tensity (hyperintence) on T1-weighted magnetic reso-
nance (MR) images [5]. In addition, several MR imaging
sequences aid in the detection of fat, including fat sup-
pression sequences (hypointence) and chemical shift im-
aging with opposed-phase gradient-echo sequences [6,7].
There are two masses with different imaging proper-
ties in the present case. One of them is compatible with
gastric cancer metastasis and the second is compatible
with hepatic lipoma, therefore both do not require sur-
gery.
Although some hepatic lipomas may mimick angiomi-
olipomas [8,9], they don’t carry malignant potential and
there are many characteristic findings on US, CT and
MRI, which are satisfactory evidences for hepatic lipoma
diagnosis. Therefore many authors do not recommend
more aggressive diagnostic procedures, such as needle
liver biopsy and operation [10]. We also believe that
awareness from characteristic imaging findings of he-
patic lipoma may prevent redundant invasive procedures.
4. References
[1] C. Basaran, M. Karcaaltincaba, D. Akata, N. Karabulut,
D. Akinci, M. Ozmen and O. Akhan, “Fat-Containing
Lesions of the Liver: Cross-Sectional Imaging Findings
with Emphasis on MRI,” American Journal of Roent-
genology, Vol. 184, No. 4, 2005, pp. 1103-1110.
[2] C. C. Reading and J. W. Charboneau, “Case of the Day.
Ultrasound. Hepatic Lipoma,” Radiographics, Vol. 10,
No. 3, 1990, pp. 511-512.
[3] S. R. Prasad, H. Wang, H. Rosas, C. O. Menias, V. R.
Narra, W. D. Middleton and J. P. Heiken, “Fat-Containing
Lesions of the Liver: Radiologic-Pathologic Correlation,”
Radiographics, Vol. 25, No. 2, 2005, pp. 321-331.
[4] G. Heinz-Peer, C. Oettl, G. Mayer and G. H. Mostbeck,
“Hypoechoic Perirenal Fat in Renal Transplant Recipi-
ents,” Radiology, Vol. 193, No. 3, 1994, pp. 717-720.
[5] F. Musante, L. E. Derchi, F. Zappasodi, M. Bazzocchi, G.
Copyright © 2011 SciRes. SS