Journal of Biomedical Science and Engineering
Vol.6 No.5A(2013), Article ID:32035,9 pages DOI:10.4236/jbise.2013.65A007
Efficacy of non-pharmacological interventions in controlling type 2 diabetes in patients of African descent: A systematic review
![]()
1Postgraduate Medicine, Division of Medical Education, Brighton and Sussex Medical School, Brighton, UK
2Computing, Engineering and Mathematics, University of Brighton, Brighton, UK
Email: *n.t.tabet@brighton.ac.uk
Copyright © 2013 Takira Glasgow et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 10 March 2013; revised 11 April 2013; accepted 12 May 2013
Keywords: Diabetes; Education; African Descent; Non-Pharmacological Intervention; HbA1C
ABSTRACT
Purpose: The purpose of this review is to systematically assess the potential effectiveness of targeted educational and other non-pharmacological interventions on diabetes control in populations of African descent in developed countries. Such information can inform intervention strategies and highlight evidencebased approaches to deal with this significant problem in this population. Methods: A systematic review and a meta-analysis of random controlled trials and cohort studies evaluating the influence of education and other non-pharmacological interventions on HbA1C concentrations in patients of African descent with diabetes. A comprehensive search of PubMed, EMBASE, CINAHL, ZETOC, SIGLE databases was carried out. Results: Although nine studies (8 randomised controlled trials and 1 cohort study) met the inclusion criteria, relevant HbA1C data were available for 6 of the studies for the subsequent metaanalysis. Heterogeneity of meta-analysis was high (I2 = 92%), the random effects pooled standard mean difference favoured the intervention −0.66 (−1.15, −0.17), p = 0.009. After sensitivity analysis, I2 remained moderate to high at 69%. The random effects pooled standard mean difference continued to favour the intervention −0.48 (−0.81, −0.16), p = 0.009. Conclusion: There is evidence supporting the efficacy of educational and other non-pharmacological interventions in diabetes control in populations of African descent in English speaking developed countries. This conclusion is tempered by the significant heterogeneity of selected interventions and paucity of high quality research in the target population.
1. INTRODUCTION
Estimates by the WHO demonstrate the scope of the diabetes challenge: 438 million people world-wide will have diabetes by 2030, and one in three Americans will have the disease by 2050 [1,2]. The prevalence of diabetes is much higher among populations of African descent in developed countries. In the USA, for example, African Americans are twice as likely to be diagnosed with diabetes (prevalence of 11.8%) and a third of cases are undiagnosed. Further, among African Americans type 2 diabetes accounts for 90% to 95% of all cases [3]. In the UK, it was estimated that the African Caribbean population had a prevalence of diabetes three times greater than the general population in 2006 [4].
Alongside the high prevalence of diabetes among patients from African ancestry in developed countries, increased complication rates are also reported. In the US, the National Health and Nutrition Examination Survey (NHANES) 1971-1992 prospective analysis of the amputation rates of a 14,407 cohort concluded that African American participants (2199 in number) underwent 2.8 times more amputations compared to their white counterparts [5]. Feinglass and colleagues further stated that males of African ancestry were 1.7 times more likely to experience primary and repeat amputations [6]. Likewise, the prevalence of diabetic retinopathy and macular oedema was also higher in participants from African ancestry with diabetes (36.7% and 11.1% compared to 24.8% and 2.7% among white, and 25.7% and 8.9% among Chinese patients respectively) [7]. In a different study Gulliford and colleagues determined that the prevalence of sight-threatening diabetic retinopathy was 15.2% in Africans, 14.7% in African-Caribbean and 9.4% in white Europeans. The data which were collected in three South London boroughs during an 18-month period suggested that retinopathy is not only more prevalent but also more severe in those with African ancestry [8].
Particular group characteristics may influence the management of diabetes among patients of African descent. These include the adherence to medication [9], health beliefs and cultural bias [10-14], health numeracy [15], access to health care and insurance issues [16-18], and socio-economic status [19]. Self-management practices in patients of African descent and other ethnic populations in developed countries were reviewed and it was concluded that there was lack of education, understanding and communication at the patient level and cultural differences or lack of cultural sensitivity at provider levels [20,21]. Chin and colleagues reported on effectiveness of interventions to reduce racial disparities in health care [22]. The most effective interventions were found to be multifaceted programmes aimed simultaneously at patient provider and health organisation. Culturally tailored quality improvement programmes based on cultural “leverage” showed improvement in patient empowerment for self-care, decreased barriers of access to physicians and improved cultural sensitivity by health care providers. Peek et al. [23] reviewed diabetes care interventions in multiple ethnic groups such as Hispanics, African Americans, Americans of Caribbean origin, Native American, Asian American and Pacific Islanders. The most effective interventions were noted to be culturally tailored, individual education with peer support and improvements to health care systems [23]. Hawthorne et al. [24] reviewed the literature in relation to the effectiveness of culturally appropriate health education for type 2 diabetes in patients of African descent and other ethnic groups. The authors reported improvement of mean difference in HbA1C at 3 and 6 months post-intervention, but not at 12 months. However, heterogeneity in the education and follow-up methods made interpretation of the benefits difficult to interpret.
A large number of people of African and Caribbean descent live in developed countries such as the USA and the UK. Such individuals have specific characteristics which may differentiate them from other ethnic and racial groups, and also have a high rate of type 2 diabetes. Therefore, it is important to review the effectiveness of targeted non-pharmacological interventions on diabetes control in this population. Such information is essential to establish the value of such programs and to inform the design of future care strategies. The effectiveness of these interventions will be assessed by their ability to reduce blood glucose levels in the target population. The goal is to compare the interventions with control or usual care.
2. METHODOLOGY
2.1. Search Strategy
Databases (PubMed, Embase, CINAHL, ZETOC, NHS evidence, Clinical trials.gov and SIGLE) were searched using the combined search terms “type 2 diabetes” and/ or “intervention” and “black” or “African” or “Caribbean”. In addition, references of the journals and reference text books were consulted. The searches were done between November and December 2010, May to June 2011 and between September 24th and October 6th 2011 (Figure 1).
2.2. Selection Criteria
The population of interest was adult participants of African descent in developed countries which includes “African-Americans”, “African-Caribbean”, “Non-Hispanic blacks” and “self-described blacks”. Studies were restricted to those published in English from the developed
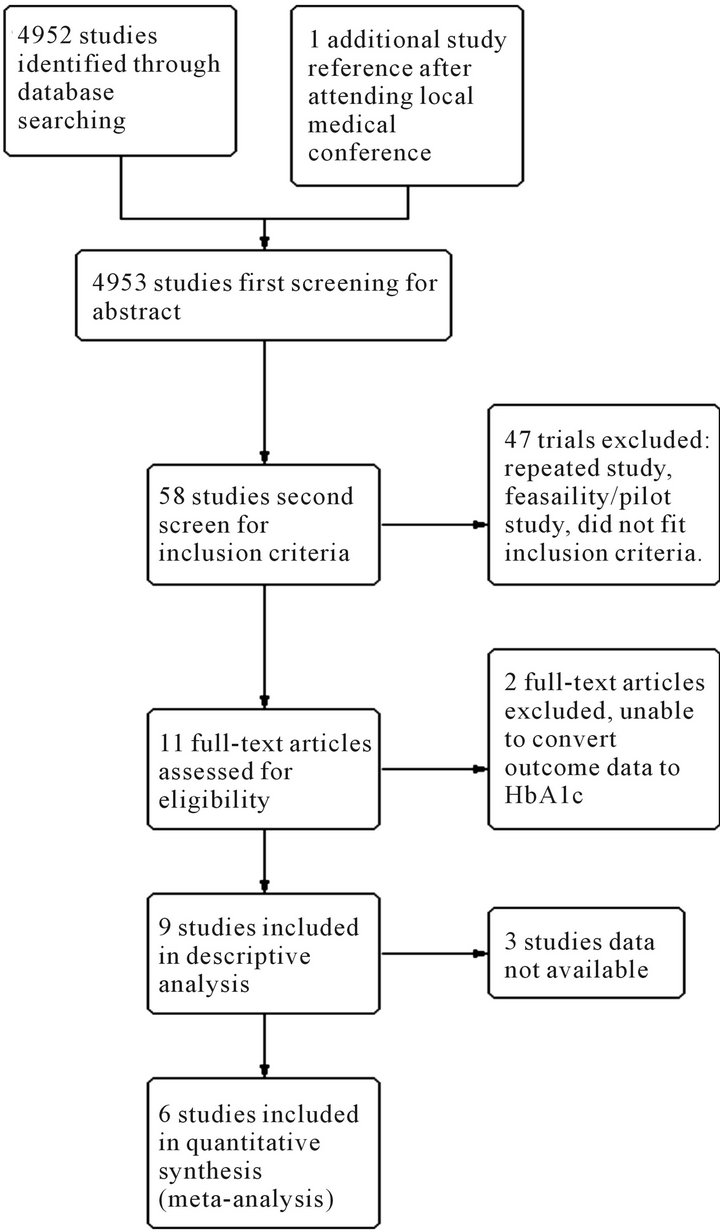
Figure 1. Flow chart screening process.
English speaking countries such as the USA and the UK The interventions of interest were non-pharmacological including educational programs. The primary outcome of interest was a measure of difference in HbA1C with the standard deviation.
2.3. Inclusion Criteria
This included randomised controlled trials (RCTs) or prospective cohort studies published between January 1st 1995 and October 6th 2011. The participants, males or females, had type 2 diabetes according to the WHO criteria and were 18 years or older (adults). Trials including participants with diabetes under age 18, persons with type 1 diabetes, known LADA, MODY and those with gestational diabetes were excluded. Also excluded, were interventions in which less than 90% of participants were of African descent. Feasibility studies for an intervention were also excluded, but pilot studies were included if the outcome data were appropriate, and if the study was not duplicated.
2.4. Quality Assessment
Critical appraisal checklists were adapted from Cochrane Collaboration tool for assessing risk of bias and the quality of each study. Information from all included studies was extracted and tabulated. Where data were insufficient for a particular study, authors were contacted for clarification.
2.5. Data Extraction
Data were extracted using a RevMan data collection form according to the selection criteria, and subsequently analysed. The information extracted included the study information (author and year), participant characteristics and number of participants recruited. The duration of intervention was 6 months where possible. Drop-outs, as well as type of intervention and duration of the intervention/study duration were also extracted with every effort to minimise missing data. The outcome measures of HbA1C difference were calculated for each trial before synthesising the data.
2.6. Data Analysis
Standardised mean difference was used to describe the data. The mean difference for the intervention and the control were calculated separately and the standard deviation within the groups calculated for missing data. The effect size calculated was from the net difference in mean HbA1C between the intervention and the control groups. Hedges unbiased estimate was used to correct the overestimated value of the mean difference in studies with small sample sizes. Sd (within) was calculated from sq root  [25].
[25].
RevMan software was used for Meta-analysis of HbA1C results. Testing for heterogeneity in the data by the chi-square test and Forest plot of the trials was included in the review. RevMan statistics were also confirmed by calculation.
3. RESULTS
Initially 4952 studies were identified through database searches of PubMed, CINAHL, Embase, and one additional from a local conference. Of the 58 potential studies for inclusion only 9 met inclusion criteria and were subsequently included in the systematic review with 8 being controlled trials. The characteristics of included studies are tabulated below (Table 1). A Pre-test posttest longitudinal study was included because this study was randomised and had two groups—a control and experimental group, resembling a RCT [26]. A control intervention time series study, a cohort study, was also included [34].
3.1. Characteristics of Included Studies
All of the studies were comparisons of interventions within an African American population and the effectiveness at improving outcomes including HbA1C. The length of trials ranged from 6 months to 36 months. The sample participant sizes ranged from 64 to 4138 with mean age of 56 - 62 years. Participants were either all or at least 94% African Americans. All selected studies were from the USA. There were over 64% females in every group. The studies took place in urban African American communities, with the exception of Skelly et al. and Anderson-Loftin et al., which were located in rural southeast and South Carolina. Control groups included a 2 × 2 factorial design [31] and a three group experimental design [33]. The studies were of an intervention compared to usual care, conventional care or minimal intervention. Comparisons between the intervention and control group baseline group characteristics were not statistically different within each study. The one exception was that of Anderson-Loftin et al. [27].
In one trial [29] HbA1C was not the primary outcome and in the remaining trials, HbA1C was not the only outcome measured; BMI/weight, lipids and blood pressure were other outcomes measured in the remaining trials. Methods used to measure the unit of the outcome HbA1C varied and included high pressure liquid chromatography, Glycaffin column method, immunoturbidimetric method, and glucometer; none of the methods accounted for haemoglobin variants. HbA1C was measured in % mg/dl; IFCC mmol/mol units were not found in the literature. Proportion of patients reaching target HbA1C was only reported in few studies so this was
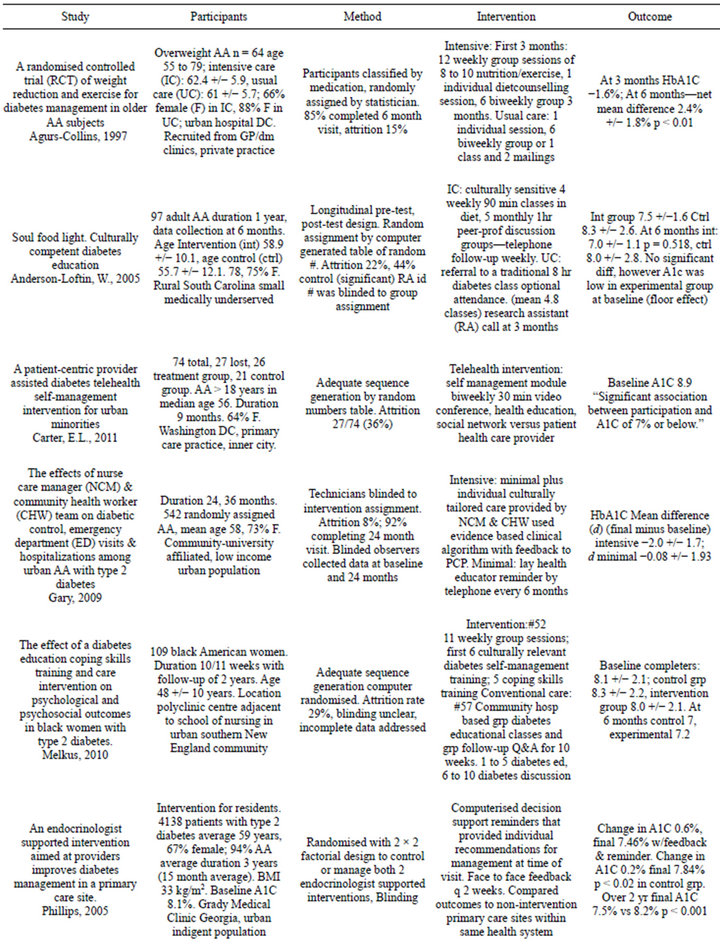
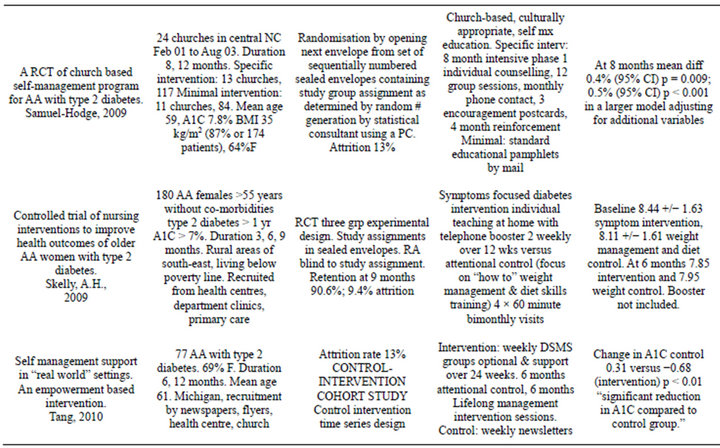
Table 1. Characteristics of included studies [26-34].
abandoned for meta-analysis.
The trials mainly targeted patient education. One study focused on exercise and dietary self-management. There were no multi-component interventions. The interventions used both individual or group designs—3 group interventions, 4 individual and 2 mixed interventions. There was one provider intervention and 8 patient interventions; the trial interventions used the expertise of diabetes educators, nurses, community health workers, lay health educators and counselors and, less often, physicians.
3.2. Quality of the Studies Selected
A total number of 3329 participants at baseline were divided into the intervention and control groups. Patients lost to attrition varied between 8% and 23% - 44%; for the latter there was a baseline difference between the intervention and control groups; all of the studies commented on attrition or addressed incomplete data. Using the modified Cochrane Collaboration tool for quality score, allocation concealment was described in one study [27], blinding in four studies [27,29,31,33], and adequate sequence generation in four [27,30,32,33]. Two studies were considered high quality, 6 studies were considered fair quality and 1 study considered inadequate/poor quality (Table 2).
Relevant HbA1C data were available for six of the studies for meta-analysis. The effect measure of standardised mean difference of the random effects model is presented in the forest plot below (Figure 2). The pooled results reveal high heterogeneity, that is, I2 = 92% of the variation between the studies is due to heterogeneity p < 0.00001; most of the observed variance is real, indicating that these studies are too different to compare. The random effects pooled standard mean difference favoured the intervention −0.66 (−1.15, −0.17). The test for overall effect produced a p = 0.009. Sensitivity analysis was done with removal of Gary study (Figure 3). This study was an outlier with weight of 18.1% (42.9% in the fixed method analysis) with sample size over 200 in each study arm; the other studies had samples sizes that were more comparable. After sensitivity analysis the heterogeneity was moderate to high I2 = 69% p < 0.01. The Chi-square test was still greater than the degrees of freedom at 12.99 versus 5 indicating heterogeneity. The random effects pooled standard mean difference still favoured the intervention after sensitivity analysis −0.48 (−0.81, −0.16). Also after sensitivity analysis the test for overall effect produced a p = 0.009.
4. DISCUSSION
In this systematic review and meta-analysis non-pharmacological care interventions specifically directed at populations of African descent appear to significantly
Table 2. Quality table for the included studies.
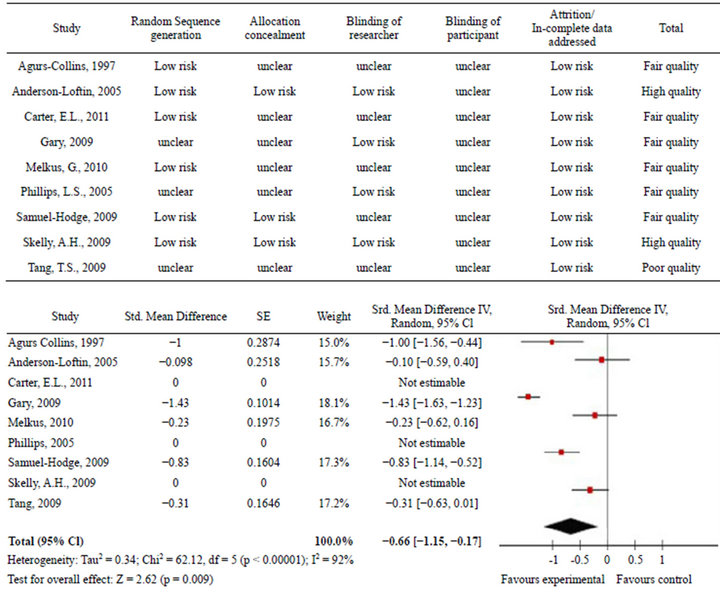
Figure 2. Forest plot of results before sensitivity analysis.
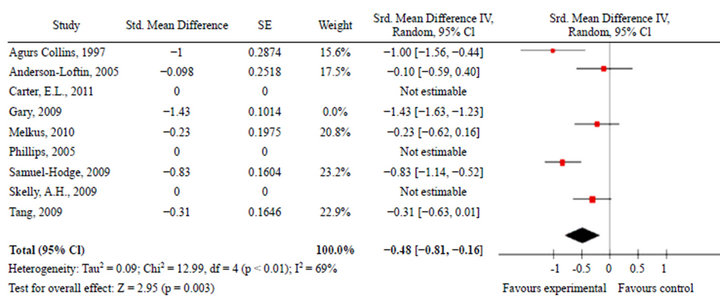
Figure 3. Forest plot of results after sensitivity analysis.
influence the concentrations of HbA1C compared to controls or usual practice. However, the conclusion of this review is likely to be influencedby the heterogeneity encountered in selected studies which undoubtedly limit the interpretation of the data. The heterogeneity encountered can be explained by the varied interventions, duration of interventions, differences in participants and differences in methods of HbA1C measurement. Although the duration of the interventions in the review was heterogeneous, improvements in glycaemic control were achievable under such circumstances. Further, the conclusion of this review is in line with previously published work showing the effectiveness of culturally tailored interventions [23]. Chin et al. [22] reported on the effectiveness of nurse-led programmes, but there was only one such programme in that review. The duration of the studies in this review is also relevant because long-term effectiveness of a trial wanes without reinforcement, and attrition also tends to decrease with the ability of a study to maintain interest and motivation. In addition, there is the possibility of successful follow-up for at least two years [29,30].
This systematic review has several limitations. Firstly, the interventions included in the systematic review were U.S. studies hence generalisability to other countries and scenarios may be limited, but nevertheless the review does give an indication of utility of targeted educational and other non-pharmacological interventions. Secondly, there was failure to comment on participant blinding and allocation concealment in 6 of the 9 selected studies, leading to selection and performance biases. Although attrition was accounted for in all studies, attrition rate was high in three of these (Carter—36%, AndersonLoftin—22% - 44%, Melkus—29%). Thirdly, publication bias leads to overestimation of intervention effect, or errors in reported effects. Grey literature was searched to decrease the possibility of bias, but this search yielded no results. Finally, the HbA1C measurement method varied between studies and although the major haemoglobinopathies of sickle cell variants are unlikely to alter measurements in populations with mean age of 56 to 62, this must be considered for the younger age groups in the general population for future research. In addition, anaemia, polycythaemia and B12 deficiencies affecting the red blood cells, affect HbA1C measurement and this was neither mentioned, nor factored into outcomes in any of the included studies.
Notwithstanding the limitations of this systematic review, there is now some indication that targeted educational and non-pharmacological interventions are worthwhile in the African ancestry population with diabetes. Hence, it is hoped that the review can impact local practice by highlighting the importance of motivating and empowering patients in their communities through appropriate interventions to complement and indeed enhance pharmacological ones. Additional well designed and powered trials are still needed to shed further light on this issue but non-controversial strategies based on current best practice can be useful and need to be implemented.
REFERENCES
- International Diabetes Federation (2009) The IDF diabetes atlas. Fourth Edition, International Diabetes Federation, Brussels.
- Boyle, J.P., Thompson, T.J., Gregg, E.W., et al. (2010) Projection of the year 2050 burden of diabetes in the US adult population: Dynamic modelling of incidence, mortality and prediabetes prevalence. Population Health Metrics, 8, 29. doi:10.1186/1478-7954-8-29
- (2011) National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States. US Department of Health and Human Services and Centers for Disease Control and Prevention, Atlanta.
- Craig, R. and Mindell, J. (2008) Health Survey for England 2006. Cardiovascular disease and risk factors in adults. http://www.ic.nhs.uk/pubs/hse06cvdandriskfactors
- Harris, M.I., Hadden, W.C., Knowler, W.C. and Bennett, P.H. (1987) Prevalence of diabetes and impaired glucose tolerance and plasma glucose levels in the US population aged 20 - 74 years. Diabetes, 36, 523-534. doi:10.2337/diabetes.36.4.523
- Feinglass, J., Rucker-Whitaker, C., Lindquist, L., McCarthy, W.J. and Pearce, W.H. (2005) Racial differences in primary and repeat lower extremity amputation: Results from a multihospital study. Journal of Vascular Surgery, 41, 823-829. doi:10.1016/j.jvs.2005.01.040
- Wong, T.Y., Klein, R., Islam, F.M.A., et al. (2006) Diabetic retinopathy in a multi-ethnic cohort in the United States. American Journal of Ophthalmology, 141, 446- 455. doi:10.1016/j.ajo.2005.08.063
- Gulliford, M.C., Dodhia, H. and Chamley, M. (2010) Socio-economic and ethnicinequalities in diabetesretinal screening. Diabetic Medicine, 27, 282-288. doi:10.1111/j.1464-5491.2010.02946.x
- Trinacty, C.M., Adams, A.S. and Soumerai, S.B. (2009) Racial differences in long-term adherence to oral antidiabetic drug therapy: A longitudinal cohort study. BMC Health Services Research, 9, 24. doi:10.1186/1472-6963-9-24
- Gamble, V.N. (1997) Under the shadow of Tuskegee: African Americans and health care. American Journal of Public Health, 87, 1773-1778. doi:10.2105/AJPH.87.11.1773
- Brown, K., Avis, M. and Hubbard, M. (2007) Health beliefs of African-Caribbean people with type 2 diabetes: A qualitative study. British Journal of General Practice, 57, 461-469.
- Scott, P.A. (1997) Culture, food, diet and diabetes: The West Indian perspective. Practical Diabetes International, 14, 209-211. doi:10.1002/pdi.1960140712
- Scott, P. (2001) Caribbean people’s health beliefs about the body and their implications for diabetes management: A South London study. Practical Diabetes International, 18, 94-98. doi:10.1002/pdi.128
- Scott, P., et al. (1998) Lay beliefs and the management of disease amongst West Indians with diabetes. Health & Social Care in the Community, 6, 407-419. doi:10.1046/j.1365-2524.1998.00148.x
- Osborn, C.Y., Cavanaugh, K. and Wallston, K.A. (2009) Diabetes numeracy: An overlooked factor in understanding racial disparities in glycemic control. Diabetes Care, 32, 1614-1619. doi:10.2337/dc09-0425
- (2009) National healthcare disparities report. Agency for Healthcare Research and Quality, Rockville. http://www.ahrq.gov/qual/nhdr09/nhdr09.pdf
- Strong, M., South, G. and Carlisle, R. (2009) The UK quality and outcomes framework pay-for-performance scheme and spirometry: Rewarding quality or just quantity? A cross-sectional study in Rotherham, UK. BMC Health Services Research, 9, 108. doi:10.1186/1472-6963-9-108
- Millett, C., Gray, J., Saxena, S., et al. (2007) Ethnic disparities in diabetes management and pay-for-performance in the UK: The Wandsworth Prospective Diabetes Study. PLOS Medicine, 4, e191. doi:10.1371/journal.pmed.0040191
- LaVeist, T.A., Thorpe Jr., R.J. and Galarraga, J.E. (2009) Environmental and socio-economic factors as contributors to racial disparities in diabetes prevalence. Journal of General Internal Medicine, 24, 1144-1148. doi:10.1007/s11606-009-1085-7
- Wilson, C., Alam, R., Latif, S., Knighting, K., Williamson, S. and Beaver, K. (2012) Patient access to healthcare services and optimisation of self-management for ethnic minority populations living with diabetes: A systematic review. Health & Social Care in the Community, 20, 1- 19. doi:10.1111/j.1365-2524.2011.01017.x
- Nam, S., Chesl, C., Stotts, N.A., Kroon, L. and Janson, L.S. (2011) Barriers to diabetes management: Patient and provider factors. Diabetes Research Clinical Practice, 93, 1-9. doi:10.1016/j.diabres.2011.02.002
- Chin, M.H., Walters, A.E., Cook, S.C. and Huang, E.S. (2007) Interventions to reduce racial and ethnic disparities in health care. Medical Care Research and Review, 64, 7S-28S. doi:10.1177/1077558707305413
- Peek, M.E., Cargill, A. and Huang, E.S. (2007) Diabetes health disparities: A systematic review of health care interventions. Medical Care Research and Review, 64, 101S-156S. doi:10.1177/1077558707305409
- Hawthorne, K., Robles, Y., Cannings-John, R. and Edwards, A.G. (2008) Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database of Systematic Reviews, 3, CD006424.
- Borenstein, M., Hedges, L.V., Higgins, J.P.T. and Rothstein, H.R. (2009) Introduction to meta-analysis. John Wiley and Sons, Ltd., Chichester.
- Agurs-Collins, T.D., Kumanyika, S.K. and Ten Have, T.R. (1997) A randomized controlled trial of weight reduction and exercise for diabetes management in older African-American subjects. Diabetes Care, 20, 1503- 1511. doi:10.2337/diacare.20.10.1503
- Anderson-Loftin, W., Barnett S. and Bunn, P. (2005) Soul food light: Culturally competent diabetes education. The Diabetes Educator, 31, 555-563. doi:10.1177/0145721705278948
- Carter, E.L., Nunlee-Bland, G. and Callender, C. (2011) A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspectives in Health Information Management, 8, 1b.
- Gary, T.L., Batts-Turner, M. and Yeh, H.C. (2009) The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: A randomized controlled trial. Archives of Internal Medicine, 169, 1788- 1794. doi:10.1001/archinternmed.2009.338
- D’Eramo Melkus, G., Chyun, D. and Vorderstrasse, A. (2010) The effect of a diabetes education, coping skills training, and care intervention on physiological and psychosocial outcomes in black women with type 2 diabetes. Biological Research for Nursing, 12, 7-19. doi:10.1177/1099800410369825
- Phillips, L.S., Ziemer, D.C. and Doyle, J.P. (2005) An endocrinologist-supported intervention aimed at providers improves diabetes management in a primary care site: Improving primary care of African Americans with diabetes (IPCAAD) 7. Diabetes Care, 28, 2352-2360. doi:10.2337/diacare.28.10.2352
- Samuel Hodge, C.D., Keyserling, T.C., Park, S., et al. (2009) A randomized trial of a church-based Diabetes self-management program for African Americans with type 2 diabetes. The Diabetes Educator, 35, 439-454. doi:10.1177/0145721709333270
- Skelly, A.H., Carlson, J., Leeman, J., et al. (2009) Controlled trial of nursing interventions to improve health outcomes of older African American women with type 2 diabetes. Nursing Research, 58, 410-418. doi:10.1097/NNR.0b013e3181bee597
- Tang, T.S., Funnell, M.M. and Brown, M.B. (2010) Selfmanagement support in “real-world” settings: An empowerment-based intervention. Patient Education and Counseling, 79, 178-184. doi:10.1016/j.pec.2009.09.029
ABBREVIATIONS
RCTs: Randomised Controlled Trials;
WHO: World Health Organisation;
LADA: Latent Autoimmune Diabetes of Adulthood;
Mody: Maturity Onset Diabetes of the Young
NOTES
g*Corresponding author.

