Journal of Diabetes Mellitus
Vol.3 No.3(2013), Article ID:35012,6 pages DOI:10.4236/jdm.2013.33021
Family responsibility dynamics for young adults in transition to adult health care*
![]()
1Adjunct Senior Lecturer Curtin University and Centre for Nursing Research, Sir Charles Gairdner Hospital, Perth, Australia; #Corresponding Author: pat.rapley@health.wa.gov.au
2Department of Endocrinology and Diabetes, Sir Charles Gairdner Hospital, Perth, Australia
Copyright © 2013 Pat Rapley et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 30 May 2013; revised 30 June 2013; accepted 8 July 2013
Keywords: Diabetes; Health-Care Transition; Parent; Adolescent; Transition Coordinator
ABSTRACT
Aim: To explore family responsibility dynamics, metabolic control, clinic attendance, and emergency admissions when young adults (YA) with type 1 diabetes transition to an adult hospital. Method: A longitudinal mixed method design with two study groups (parents, n = 28; YA intervention group, n = 23) and a YA comparison group (n = 20). Sample recruited from an outpatient diabetes centre. Demographic, clinic attendance, emergency admissions, biodata, and the Diabetes Family Responsibility Questionnaire (DFRQ) were completed on entry and sixmonths later as part of an 18-month trial of a diabetes transition coordinator (DTC). The selfreport DFRQ were analyzed using derived parent-child dyadic variables to explore differences at baseline and end of study using Wilcoxon Signed Rank Test. The relationship between metabolic control and the DFRQ patterns was explored using Spearman’s rho. Results: On completion of the study, the change in HBA1C for both adolescent groups was not significant but was less than ideal for 25% of adolescents in the study. The YA intervention group had significantly fewer missed appointments between them compared to the comparison group. The DFRQ indicated that the derived parent-child dyadic variable of task-discordance increased during the study. Conclusion: The clinically relevant diabetes-task dissonance between parents and young adults offers a challenge and a diagnostic opportunity for diabetes educators.
1. INTRODUCTION
There are approximately 10,000 15 - 25-year olds with diabetes type 1 in Australia. This group has the greatest risk of developing preventable complications with 30% - 40% lost from specialist diabetes care during transition each year. Hence, Diabetes Australia’s National Policy Priorities 2010 [1] includes better support for young people transitioning to adult services as a key issue. It recommends that young adults aged 15 - 24 have access to annual comprehensive health assessment, mental health screening at 15 years, and a central coordination system to identify and track transition progress.
Effective health care transition for adolescents with a chronic illness covers three domains: The adolescent’s emerging self-care skills and knowledge; medical management; and parents’ educational, emotional and tangible support whilst reducing involvement in their child’s diabetes-related decision-making. To this end, it has been suggested that a case-manager or diabetes transition coordinator (DTC) could support these three domains during transitioning [2,3]. In addition, the parent’s role also needs to change with the adolescent’s increasing demands for independence [4] and parental support for positive choices remains vital [4,5]. Family conflict [6] or disagreements between parent and child in perception of who assumes responsibility for the diabetes regimen and adherence level are significant predictors of glycemic control [7]. The views of the parent [4], however, have not been explored in detail previously. Hence, the purpose of this study was to explore family responsibility dynamics, metabolic control, clinic attendance, and emergency admissions when young adults (YA) with type 1 diabetes transition to an adult hospital.
1) Improve health status of adolescents and young adults transitioning from a pediatric hospital to a Young Adults with Diabetes (YAD) clinic at the adult hospital.
2) Reduce the number of ‘missed’ appointments.
3) Reduce the number of DKA events.
2. METHODS
A longitudinal, exploratory, mixed method design was used. Ethics approvals were obtained from Human Research Ethics Committees at the adult and pediatric hospitals. Although the study extended over 18 months, duration of individual contact with the diabetes transition coordinator (DTC) during the study varied from four to six months.
Once notified by the pediatric hospital, the DTC contacted and worked with adolescents and their family prior to transfer or soon after to help negotiate the adult system, assist with appointments, and promote independence in self-care behaviour. An initial interview with the adolescent and parent, alone or separately, was followed by monthly telephone contact. Participants were also encouraged to contact the DTC as needed.
2.1. Participants and Procedures
Inclusion criteria included adolescents identified for transition to the adult hospital within the next two months or recently transferred. Parents of adolescents who did not consent were not excluded and vice versa. Adolescents under 18 years of age required parental assent. A comparison group of YA was created from nonparticipants in the target group who had had more than one appointment at the YAD clinic during the study recruitment period (n = 61). Questionnaires and hospital records were used to collect data.
2.2. Instruments
Permission to use the Diabetes Family Responsibility questionnaire (DFRQ) was granted [7]. Both parent and adolescent participants completed the DFRQ preand post-intervention. The DFRQ, with proven reliability [8-10], explored the relationship between parent’s and adolescent’s self-reported view of who had responsibility for 17 tasks covering three subscales-general health, regimen tasks and social presentation. This three-point questionnaire was completed separately by the adolescent and a parent, each indicating who (adolescent, equal, parent) had responsibility. Tasks considered an adolescent responsibility were scored as one, two if a joint responsibility task and three if parent took responsibility. Hence, higher scores indicated more parental responsibility. The three possible response patterns suggested by Anderson [7] were categorised as 1) perfect agreement, 2) disagreement or an overlap pattern with each claiming more responsibility than the other, and 3) discordant pattern or disagreement in which no one was taking responsibility. Clinically, the discordant pattern was most concerning because it has been reported as most likely associated with poor health outcomes [7]. The derived dyadic variables of agreement, discordance and overlap had a score range of 0 to 17. The internal consistency results for this sample were adequate given its novel use with an adolescent cohort [11-13] with alphas of 0.78 for the adolescent sample and 0.84 for parents at T0 and 0.79 and 0.83 at T6 respectively. These results are also consistent with other studies [8-10].
2.3. Analyses
Demographic, biodata and DFRQ scores were analysed using the Statistical Package for the Social Sciences (IBM SPSS version 19) software package and its default settings. Descriptive statistics provided demographic context for study findings. Where possible, chi-square analysis was used to explore bivariate group differences. Parent and child responses to the self-report DFRQ were analysed using derived parent-child dyadic variables to explore differences at baseline and end of study using Wilcoxon Signed Rank Test. The number of tasks in the discordance category and change over time was also explored. The relationship between metabolic control and the DFRQ patterns was explored using Spearman’s rho.
3. RESULTS
The 51 volunteer participants included 23 adolescents and 28 parents. Mothers represented 78.57% of the parent group. The non-participant group (n = 61) included 41 individuals for whom there were minimal data—age and or gender only. The remaining 20 adolescents formed a comparison group. The adolescent intervention group’s mean age was 18.39 (17 - 20 years ± 0.722) with 73.91% being male (n = 17). The comparison group’s mean age was 18.95 (17 - 20 years ± 0.887) with 40% male (n = 8); a significantly greater proportion of males in the intervention group (73.91%, Fisher’s Exact Test P = 0.033, 2-sided). Duration of diabetes for the intervention adolescent group ranged from 1-18 years (median = 11 ± 4.62).
Hospital records for the nine months prior to the study indicated four YA (18.2%) in the intervention group had either one or two DKA events compared to three participants who had one DKA event during the study period. One of the four had two DKA events prior to and one during the study. Insufficient hospital data available for the comparison group before or during the study period.
Group comparison between the equivalent nine-month periods before and during the study identified zero to seven missed appointments which reduced to three during the study. Chi-square analyses of appointment history indicated the intervention group’s missed appointments during the study were significantly less than for the comparison group (n = 34, χ2 = 18.67, df = 3, P < 0.001). That is, eight of the intervention group had 10 missed appointments between them compared to the comparison group’s 12 individuals with 17 missed appointments.
Comparing the previous nine months to the equivalent period of the study, 11 of the 16 (68.75%) intervention group with pre and post HbA1c data had improved. Changes in HbA1c ranged from −37 to 45 mmol/mol (−3.4% to 4.1%). A successful or adequate change in HbA1c from entry (T0) to six months later (T6) was defined as a T6 HbA1c less than or equal to 59 mmol/mol (7.5%) or, if T0 greater than 59 mmol/mol but difference was equal to or less than 5.5 mmol/mol (0.5%). Similarly, for those in the comparison group for whom we had sufficient data, 15 of the 19 (78.94%) improved. Their change in HbA1c ranged from −22 mmol/mol to 27 mmol/mol (−2.0% to 2.5%). Difference was not significant (n = 35, Fisher’s Exact test P = 0.700 2-sided). In total, however, only 26 of the 35 (74.286%) YA were judged to have effective metabolic control.
The DFRQ completed by both intervention groups included 22 pairs at T0 and 20 at T6. Wilcoxon Signed Rank Test for differences between the three DFRQ dyadic patterns of agreement, overlap and discordance over six months indicated retention of the null hypothesis. By the study end the overlap of responsibility pattern was less with greater congruence about task responsibility— the agreement pattern. The 22 pairs agreed on 5 - 15 of the 17 tasks at T0 whereas 20 of the pairs agreed on 8 - 15 of the tasks six months later. See Table 1. However,
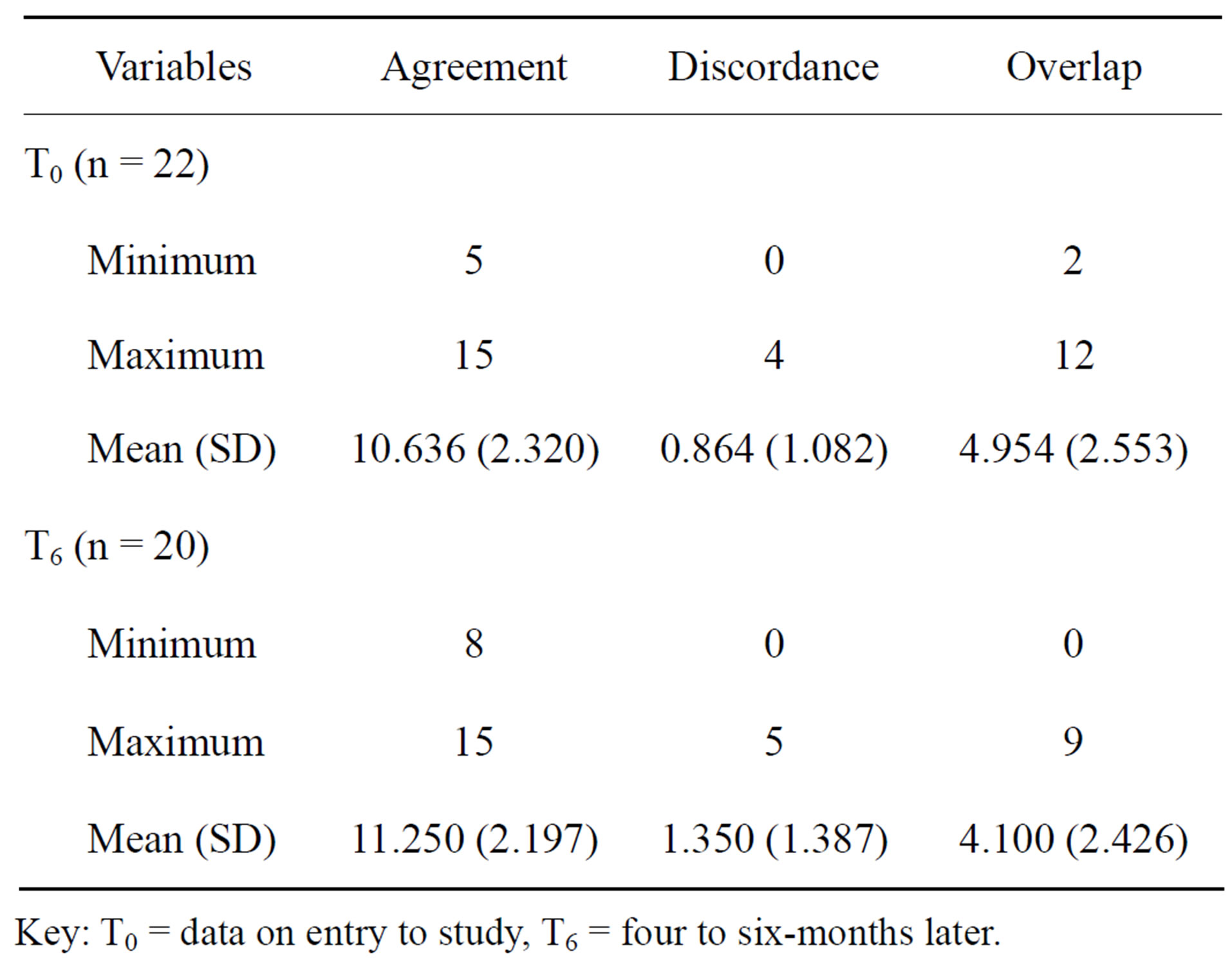
Table 1. Minima, maxima, mean and standard deviation (SD) for each DFRQ dyadic pattern at T0 and T6.
Key: T0 = data on entry to study, T6 = four to six-months later.
the frequency of the clinically important pattern of discordance increased. Initially 11 (50%) parent-child pairs indicated a discordance pattern for 1 - 4 of the 17-DFRQ tasks and 14 (70%) did so for 1 - 5 items six months later. Of the 20 dyadic parent-child scores, only five increased their item-discordance pattern by one, one pair increased by three and another by five—giving seven pairs with a greater item-discordance pattern at the study’s end. A Spearman’s rho analysis indicated a moderate but nonsignificant relationship between the initial T0 agreement pattern and HbA1c (rs = −0.40, n = 20, P = 0.079).
4. DISCUSSION
The purpose of this study was to explore family responsibility dynamics when YA with type 1 diabetes transitioned to an adult hospital with a DTC to facilitate the transition process. The principal finding was a significantly greater compliance with clinic attendance by the intervention group. However, whilst this could not be solely attributed to the DTC it should be noted that the actual clinic attendance rate was higher than an earlier study at the same hospital prior to the introduction of the DTC [14]. Other studies have attributed their improved clinic attendance rate to their separate young adult clinic and a policy of pursuing non-attendees by telephone or letter [15,16]. Since the context for this study included both a DTC and a YAD clinic, their separate contribution cannot be quantified. The results could be explained by the single line of communication where problems could be discussed and avoided or fixed, including appointment problems [16,17]. One communication channel can also mean a less daunting new environment for adolescents.
More telling is the metabolic control for this sample. Whilst most of the comparison and intervention group met the criteria for adequate improvement in their HBA1C, it is concerning that the HbA1c is less than ideal for 25% of adolescents in the study. The non-significant difference in HbA1c levels for the two groups is, however, consistent with another Australian study [18]. More generally, however, the consensus is that the competing peer-group, career and diabetes self-management demands on the YA at this time can mean deterioration in metabolic control [19-21].
Another change dynamic at this time is the role of parents in the young persons’ diabetes self-management. The study’s underlying assumption is that, not only are parents or carers an essential part of the solution to improving health outcomes after transition for the young adults [22,23], but equally, clinic attendance in the first two years after transition. Therefore, it was necessary for the DTC to work with parents and their child, whilst observing everyone’s rights for confidentiality. Whilst the DFRQ, for this sample indicates less ambiguity and more agreement about task responsibilities over time, it also reveals a worrying trend of more discordance between some parent-child dyads after transitioning. The increase in diabetes self-care tasks for which no-one takes responsibility is a warning for the diabetes team working with an 18 - 25 year old cohort.
The T0 agreement pattern and HbA1c at the start of the study reflects the more parent-dependent role found at transition and young adults’ reliance on parents as a coping strategy to manage HbA1c levels [4]. It could also be argued that the increased frequency of the clinically important pattern of discordance pattern at the study’s end suggests diminishing reliance on parents with emergent independence and conflict. Concomitant service delivery support informed by assessment of the adolescent’s readiness for self-management either before or after transition to adult health care, perhaps using the DFRQ, and an adolescent-friendly appointment process could create the environment for a smooth transition and improved metabolic control. Other studies have demonstrated the importance to metabolic control of clarifying diabetes-related task responsibilities [8,9,24,25].
The study has several limitations. First, the small sample and the number of missing values prevented more detailed statistical analyses. The missing data were mainly due to participants’ missed appointments, the phenomenon at the heart of the study itself. Second, we could not examine the relationship between adolescentparent responsibility and metabolic control as suggested by Belendez [26]. However, given that the DFRQ is a valid and reliable measure, results provides some credibility and support for a longer multi-centre study. Nevertheless, the results should be interpreted with caution.
5. CONCLUSIONS
The economic burden of diabetes is high for the individual, the family, the health care sector and the whole community [27, p. 1]. This burden will only increase if transition from pediatric to adult health care is less than ideal [28-31]. The success of dedicated transition clinics [16,17,32] and recommendations from the international literature for a DTC [17,33] or similar role provides direction for practice change. In general, however, the focus needs to change from an adult medical model of care to one that acknowledges adolescent health differences. One that also recognises the young adult’s need for continued parental involvement and support [22,34], and one that can foster their emerging self-management skills. Thus, the clinically relevant diabetes-task dissonance between parent and the young adult offers a challenge and a diagnostic opportunity not previously explored by adult hospital health professionals.
Furthermore, for the young metropolitan adults in this sample who need some support, this study suggests that a more youth-friendly appointment system is needed to meet the recommended three-monthly appointments for the two years after transition to the adult hospital [35].
Whilst not directly addressing the constraints within the existing adult hospital appointment system, changes implemented include the use of mobile phone reminders and E-referrals to dedicated transition mailbox used by pediatric and adult YAD clinic endocrinologist and nurse coordinator. Also, adult-hospital staff sensitivity toward the continuing parent-child co-decision-making process around glycemic targets and of the needs and role of parents attending the YAD clinic is increasing. Rather than automatic exclusion of parents because of confidentiality concerns, a prompt question that provides the possibility of parent inclusion is part of the welcome conversation.
Furthermore, since the DFRQ only takes a minute to complete, it will be trialled as a diagnostic tool used at the initial YADs clinic by the diabetes educator for targeted remedial action by identifying tasks for which no one is claiming responsibility. Many youths are still not taking full responsibility for their diabetes self-management six months after transfer to adult health care. Diabetes educators with specialist knowledge of adolescent health can advocate for the young adult whilst supporting the parent [22,31,36]. Learning to “let go” when your child has diabetes can be fraught with danger—a situation more understood by the parent than the child.
6. ACKNOWLEDGEMENTS
The project was financially supported by the Diabetes Research Foundation (Western Australia). In addition the authors would like to thank Professor Tim Jones, Princess Margaret Hospital for Children, for his assistance in developing the grant proposal and initial project design.
REFERENCES
- Johnson, G. (2010) National policy priorities 2010: Towards better management and prevention of diabetes for all Australia. Conquest, Winter, 30-31.
- Pacaud, D. (2005) Editorial commentary. Bridge over troubled water: Improving the transition from pediatric to adult care. The pediatric perspective. Canadian Journal of Diabetes, 29, 183-184. http://www.diabetes.ca/files/Pacaud,Blumer%20Commentaries--Bridging--Staying.pdf
- Reid, G., Irvine, J., McCrindle, B., et al. (2004) Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics, 113, e611- e612. doi:10.1542/peds.113.3.e197
- Karlsson, A., Arman, M. and Wikblad, K. (2008) Teenagers with type 1 diabetes—A phenomenological study of the transition towards autonomy in self-management. International Journal of Nursing Studies, 45, 562-570. doi:10.1016/j.ijnurstu.2006.08.022
- He, K., Kramer, E., Houser, R., Chomitz, V. and Hacker, K. (2004) Defining and understanding healthy lifestyle choices for adolescents. Journal of Adolescent Health, 35, 26-33. doi:10.1016/j.jadohealth.2003.09.004
- Lancaster, B.M., Pfeffer, B., McElligott, M., et al. (2010) Assessing treatment barriers in young adults with type 1 diabetes. Diabetes Research and Clinical Practice, 90, 243-249. doi:10.1016/j.diabres.2010.07.003
- Anderson, B., Auslander, W., Jung, K., Miller, J.P. and Santiago, J. (1990) Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology, 15, 477-492. doi:10.1093/jpepsy/15.4.477
- Anderson, B.J., Holmbeck, G., Iannotti, R.J., et al. (2009) Dyadic measures of the parent-child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Families, Systems, & Health, 27, 141-152. doi:10.1037/a0015759
- Cameron, F., Skinner, T., de Beaufort, C., et al. (2008) Are family factors universally related to metabolic outcomes in adolescents with type 1 diabetes? Diabetic Medicine, 25, 463-468. doi:10.1111/j.1464-5491.2008.02399.x
- Vesco, A., Anderson, B., Laffel, L., Dolan, L., Ingerski, L. and Hood, K. (2010) Responsibility sharing between adolescents with type 1 diabetes and their caregivers: Importance of adolescent perceptions on diabetes management and control Journal of Pediatric Psychology, 35, 1168-1177. doi:10.1093/jpepsy/jsq038
- Field, A. (2005) Reliability analysis. In: Field, A., Ed., Discovering Statistics Using spss. 2nd Edition, Sage, London, Chapter 15.
- Lance, C., Butts, M. and Michels, L. (2006) The sources of four commonly reported cutoff criteria: What did they really say? Organizational Research Methods, 9, 202-220. doi:10.1177/1094428105284919
- Nunnally, J. and Bernstein, I. (1994) Psychometric theory. 3rd Edition, McGraw-Hill, New York.
- Rapley, P., Hart, L., Babel, G. and Kaye, J. (2007) Young adults transferring to a young adult diabetes clinic: Hba1c and missed appointments. Australian Diabetes Educator, 10, 8, 10-12, 30.
- Gholap, N., Pillai, M., Virmani, S., et al. (2006) The alphabet strategy and standards of care in young adults with type 1 diabetes. The British Journal of Diabetes & Vascular Disease, 6, 168-170. doi:10.1177/14746514060060040401
- Holmes-Walker, D., Llewellyn, A. and Farrell, K. (2007) A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with type 1 diabetes aged 15-25 years. Diabetic Medicine, 24, 764-769. doi:10.1111/j.1464-5491.2007.02152.x
- Crowley, R., Wolfe, I., Lock, K. and McKee, M. (2011) Improving the transition between paediatric and adult healthcare: A systematic review. Archives of Disease in Childhood, 96, 548-553. doi:10.1136/adc.2010.202473
- Farrell, K. and Holmes-Walker, J. (2011) Maintaining outcomes after 10 years of a diabetes transition support program. Australian Diabetes Society & Australian Diabetes Education Association Annual Scientific Meeting, Perth, 31 August-2 September 2011, 2241.
- Beskine, D. and Owen, P. (2008) Review of transitional care for young people with diabetes. Journal of Diabetes Nursing, 12, 34-38.
- Grey, M., Davidson, M., Boland, E. and Tamborlane, W. (2001) Clinical and psychosocial factors associated with achievement of treatment goals in adolescents with diabetes mellitus. Journal of Adolescent Health, 28, 377-385. doi:10.1016/S1054-139X(00)00211-1
- Helgeson, V., Snyder, P., Seltman, H., Escobar, O., Becker, D. and Siminerio, L. (2010) Brief report: Trajectories of glycemic control over early to middle adolescence Journal of Pediatric Psychology, 35, 1161-1167. doi:10.1093/jpepsy/jsq011
- Allen, D., Channon, S., Lowes, L., Atwell, C. and Lane, C. (2011) Behind the scenes: The changing roles of parents in the transition from child to adult diabetes service. Diabetic Medicine, 28, 994-1000. doi:10.1111/j.1464-5491.2011.03310.x
- Lewin, A.B., Heidgerken, A.D., Geffken, G.R., et al. (2006) The relation between family factors and metabolic control: The role of diabetes adherence. Journal of Pediatric Psychology, 31, 174-183. doi:10.1093/jpepsy/jsj004
- Dashiff, C., Hardeman, T. and McLain, R. (2008) Parent-adolescent communication and diabetes: An integrative review. Journal of Advanced Nursing, 62, 140-162. doi:10.1111/j.1365-2648.2007.04549.x
- Ingerski, L., Anderson, B., Dolan, L. and Hood, K. (2010) Blood glucose monitoring and glycaemic control in adolescence: Contribution of diabetes-specific responsibility and family conflict. Journal of Adolescent Health, 47, 191-197. doi:10.1016/j.jadohealth.2010.01.012
- Beléndez, M., de Wit, M. and Snoek, F.J. (2010) Assessment of parent-adolescent partnership in diabetes care: A review of measures. The Diabetes Educator, 36, 205-215. doi:10.1177/0145721709359205
- National Health and Medical Research Council. (2005) Clinical practice guidelines: Type 1 diabetes in children and adolescents. Department of Health and Ageing, Canberra, 315, 2169.
- Bryden, K., Dunger, D., Mayou, R., Peveler, R. and Neil, H.A. (2003) Poor prognosis of young adults with type 1 diabetes: A longitudinal study. Diabetes Care, 26, 1052- 1057. doi:10.2337/diacare.26.4.1052
- Busse, F.P., Hiermann, P., Galler, A., et al. (2007) Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Hormone Research, 67, 132-138. doi:10.1159/000096583
- Kipps, S., Bahu, T., Ong, K., et al. (2002) Current methods of transfer of young people with type 1 diabetes to adult services. Diabetic Medicine, 19, 649-654. doi:10.1046/j.1464-5491.2002.00757.x
- Visentin, K., Koch, T. and Kralik, D. (2006) Adolescents with type 1 diabetes: Transition between diabetes services. Journal of Clinical Nursing, 15, 761-769. doi:10.1111/j.1365-2702.2006.01347.x
- Diabetes Australia (2007) National review of transitional care. Diabetes Australia and Eli Lilly, Canberra.
- Jones, S. and Hamilton, S. (2008) The missing link: Paediatric to adult transition in diabetes services. British Journal of Nursing, 17, 842-847.
- Viklund, G. and Wikblad, K. (2009) Teenagers’ perceptions of factors affecting decision-making competence in the management of type 1 diabetes. Journal of Clinical Nursing, 18, 3262-3270. doi:10.1111/j.1365-2702.2009.02963.x
- National Collaborating Centre for Women’s and Children’s Health (2004) Type 1 diabetes: Diagnosis and management of type 1 diabetes in children and young people. RCOG Press, London.
- Rapley, P. and Davidson, P.M. (2010) Enough of the problem: A review of time for health care transition solutions for young adults with a chronic illness. Journal of Clinical Nursing, 19, 313-323. doi:10.1111/j.1365-2702.2009.03027.x
NOTES
*Conflicts of interest statement: the authors had no conflict of interest, real or perceived. Funding for the study was a competitive grant. The funding body had no role in the study design, data collection, and analysis of the data or the writing of the manuscript. The funding body, however, does have an expectation that the results will be published.

