International Journal of Otolaryngology and Head & Neck Surgery
Vol.04 No.03(2015), Article ID:56014,4 pages
10.4236/ijohns.2015.43036
Klestadt’s Cyst: Case Report
Kartik Parelkar, Smita Nagle, Mohan Jagade, Reshma Hanwate, Madhavi Pandare, Devkumar Rangaraja, Kiran Kulsange, Bandu Nagrale, Arpita Singhal
Department of ENT, Grant Govt Medical College & Sir J J Group of Hospitals, Mumbai, India
Email: kartikparelkar@ymail.com
Copyright © 2015 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 4 April 2015; accepted 20 April 2015; published 28 April 2015
ABSTRACT
Klestadt’s cyst, more commonly known as the nasolabial cyst, is an uncommon, non-odontogenic, and soft tissue cyst. It is classified as a fissural cyst, found outside the bone, and on the region corresponding to the nasolabial furrow and alar nose. Following its description first by Zukuerkandl in 1882, only 267 cases have been found in English literature. In spite of the low occurrence of nasolabial cysts, it is important to recognize the clinical characteristics of this lesion. The purpose of this report is to review the literature and discuss the histomorphology and etiology of this condition, and also its management by surgical excision. As per our experience, sublabial approach is the best for complete and scarless excision of this cyst.
Keywords:
Klestadt’s, Nasolabial Cyst, Non-Odontogenic

1. Introduction
The nasolabial cyst is a rare nonodontogenic cyst originating in maxillofacial soft tissues [1] . Following its description first by Zukuerkandl in 1882, only 267 cases have been found in English literature [2] .
Rao revised the nomenclature and defined nasolabial cysts as lesions located entirely within soft tissue, different from nasoalveolar cysts, which caused maxillary bone erosion [3] .
There are two main etiological theories having been proposed. One holds that the lesion arises from trapped nasolacrimal duct tissue [4] , while the other affirms that it is an embryonic fissural cyst [5] . Klestadt [6] first postulated an embryologic origin for these cysts and considered that these lesions must originate from embryonic epithelium, entrapped in the developmental fissures between the lateral nasal and maxillary processes. Since then, many authors have classified this entity based on Klestadt’s embryologic theory as a fissural cyst [7] .
Klestadt’s cyst presents at an extraosseous location in the region of the nasolabial fold and can cause swelling in the furrow, alar nose elevation and upper lip projection.
Though uncommon, management of this cyst is based on its correct diagnosis. Hence, we report this case of nasolabial cyst.
2. Case Report
A 45-year-old woman presented to our ENT department with a right sided nasal mass (Figure 1) which she had noticed since last 2 years. She had complaints of partial nasal obstruction on the same side.
There was no h/o epistaxsis, nasal trauma or any previous surgery. On examination the mass was visible in the right nasal vestibule; the furrow of the alar cartilage was lost partially.
The swelling was cystic in consistency and could be palpated bimanually through the nose and the oral cavity. Rest of the oral cavity and the nose appeared to be normal.
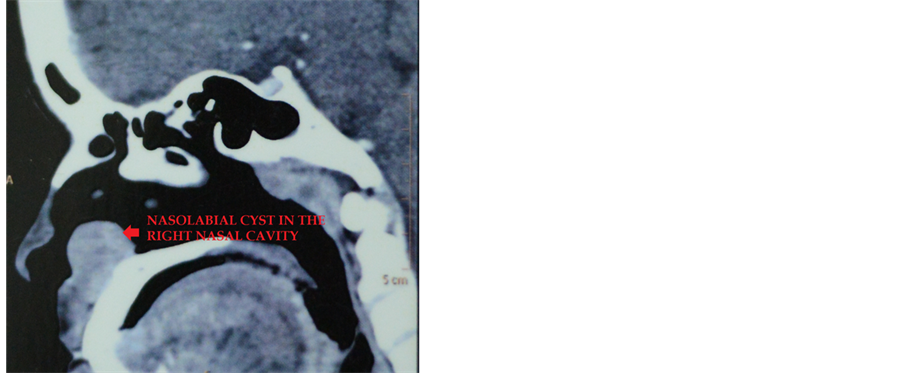
A CT (computed tomography) with contrast of the paranasal sinuses revealed a 2.3 × 2.1 cm round mass like lesion in the right anteroinferior nasal cavity. CT attenuation value measured 59 HU on plain scan and 73 HU on post contrast study, with homogenous enhancement. There was minimal scalloping of the adjacent maxillary bone but no obvious erosion (Figure 2).
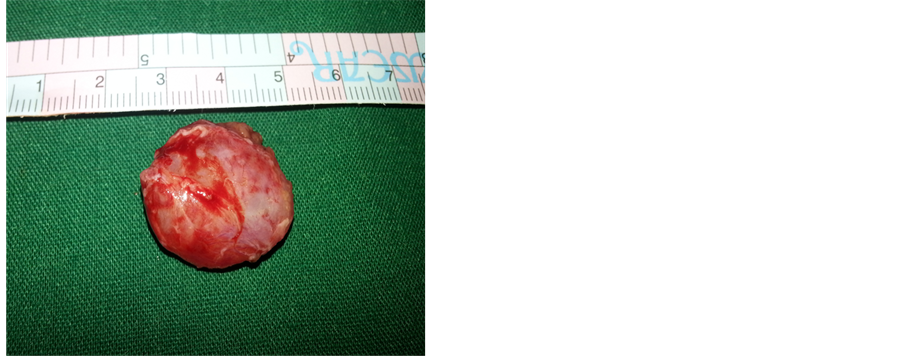
After routine pre-anaesthetic workup and patients consent excision of the mass was planned. Asublabial incision of approximately 4 cms was made on the right side and the cyst was finely dissected from the surrounding tissue (Figure 3 and Figure 4).
There was a small breach in the floor of the nose, the mucosa was reposited and sandwiched between a layer of betadine soaked gelfoam. The sublabial incision was sutured with vicryl 4 - 0. Postoperative period was insignificant. There is no evidence of recurrence 6months postoperatively.
The histopathological report stated that the cyst contained yellowish straw coloured fluid and it was lined by respiratory epithelium with squamous metaplasia and mucous glands in the fibrous stroma suggestive of a nasolabial cyst (Figure 5).
3. Discussion
Nasolabial cysts represent about 0.7% of all cysts in the maxillofacial region [2] , and 2.5% of non odontogenic cysts [1] . Many authors believe that its prevalence is actually higher than presented in the literature; however, due to misdiagnosis, indexes remain low [1] .
Figure 1. Right nasal mass.
Figure 2. CT scan showing the nasolabial cyst in the right nasal cavity (axial and sagittal cuts respectively).
Figure 3. Intraoperative view after dissecting the cyst from the surrounding tissue.
Figure 4. Excised nasolabial cyst specimen.
Figure 5. H & E stained slide showing ciliated columnar epithelial lining and fibrous stroma of the cyst wall.
These cysts are usually unilateral, but bilateral cases have been also reported, it has been estimated that approximately 10% of the cases are bilateral [8] [9] . There is a sex predilection of incidence in females (3.7:1) and age predilection in 2nd to 7th decade though it frequently occurs during middle age [1] .
The clinical findings are fairly typical. Patients usually complain of a swelling adjacent to the nose, and sometimes the cyst may be observed on routine examination [10] [11] . The development of swelling in the maxillary buccal sulcus may reach great dimensions, causing discomfort with the use of dentures, breathing obstruction and facial asymmetry. In this report, the patient mainly complained about alar nose flaring, diminished nasolabial sulcus, and nasal mass which was actually the elevated floor of the nasal cavity.
Due to similar signs and symptoms, this lesion may be misdiagnosed as a dental or periodontal abscess, odontogenic cyst, tumor and choanal polyp [12] .
The odontogenic cysts that should be excluded are periapical inflammatory lesions (granuloma, cyst or abscess) that have thinned out the bone. Careful examination of the adjacent teeth and testing its vitality can help to rule out this possibility. Orthopantomogram (OPG) will show evidence of non vital tooth with radiolucency. OPG in our patient was normal.
Dentigerous cyst also needs to be excluded. Usual radiographic appearance of dentigerous cyst is that of a well-demarcated radiolucent lesion attached at an acute angle to the cervical area of an unerupted tooth.
Another possible cyst of non-odontogenic origin is the epidermoid or epidermal inclusion cyst. As opposed to the normal pink or bluish coloration of a nasolabial cyst, this cyst is yellow hue in colour and patient may have a history of trauma or previous surgery.
Also neoplasm that needs to be excluded in this area is minor salivary gland tumor. As oppose to nasolabial cyst, minor salivary gland tumors are usually non fluctuant.
CT scan can help to exclude mass lesions causing bony erosion and most of the differentials. Though in the literature, rare cases of radicular absorption due to these cysts do exist. However, minimal scalloping of the maxillary bone as observed in our case was also observed by other authors [13] [14] .
Histologically, the cyst may be lined by pseudostratified columnar epithelium which is sometimes ciliated often with goblet cells and mucous cells, or by stratified squamous epithelium [15] .
Though marsupialisation has been done in some cases, surgical excision via the sublabial incision is the treatment of choice.
Because this cyst is usually closely related to the floor of the nose [16] [17] perforation of the nasal mucosa may be expected during its removal. When very small perforations are caused, they can be left untreated, as in our case. However, larger ones must be sutured.
Malignant transformation is rare and has been documented in only one case [18] .
4. Conclusion
Klestadt’s cyst is rare maybe due to its misdiagnosis and must be kept in mind in differential diagnosis of nasal vestibule, nasal base, and sublabial area lesions. Although uncommon in occurrence, it is imperative for the clinician to make an accurate diagnosis and provide appropriate treatment.
References
- Mervyn, S. and Speight, P. (2007) Cysts of the Oral and Maxillofacial Regions. 4th Edition, Blackwell publishing limited, Singapore.
- Patil, K., Mahima, V.G. and Divya, A. (2007) Klestadt’s Cyst: A Rarity. Indian Journal of Dental Research, 18, 23-26. http://dx.doi.org/10.4103/0970-9290.30918
- Tiago, R.S., Maia, M.S., Nascimento, G.M., Correa, J.P. and Salgado, D.C. (2008) Nasolabial Cyst: Diagnostic and Therapeutical Aspects. Revista Brasileira de Otorrinolaringologia, 74, 1. http://dx.doi.org/10.1590/S0034-72992008000100007
- Precious, D.S. (1987) Chronic Nasolabial Cyst. Journal of the Canadian Dental Association, 53, 307-308.
- Wesley, R.K., Scannel, T. and Nathan, L.E. (1984) Nasolabial Cyst: Presentation of a Case with a Review of the Literature. Journal of Oral and Maxillofacial Surgery, 42, 188-192. http://dx.doi.org/10.1016/S0278-2391(84)80032-4
- Klestadt, W.D. (1953) Nasal Cyst and Facial Cleft Cyst Theory. Annals of Otology, Rhinology, and Laryngology, 62, 84-89. http://dx.doi.org/10.1177/000348945306200108
- Egervary, G. and Csiba, A. (1969) Bilateral Nasolabial Cyst. Dental Digest, 75, 504-507.
- Smith, R.A., Katibah, R.N. and Merrell, P. (1982) Nasolabial Cyst: Report of a Case. Journal of the Canadian Dental Association, 11, 727-729.
- Roed-Petersen, B. (1969) Nasolabial Cysts: A Presentation of Five Patients with a Review of the Literature. British Journal of Oral Surgery, 7, 84-95. http://dx.doi.org/10.1016/S0007-117X(69)80002-8
- Campbell, R.L. and Burkes Jr., E.F. (1975) Nasolabial Cyst: Report of Case. The Journal of the American Dental Association, 91, 1210-1213. http://dx.doi.org/10.14219/jada.archive.1975.0575
- Rao, R.V. (1955) Naso-Labial Cyst. Journal of Laryngology & Otology, 69, 352-354. http://dx.doi.org/10.1017/S0022215100050799
- Werner, P.E., Lehman, R.H., Collentine, M.E. and Darling, R.J. (1968) Intraoral Presentation of a Nasal (Choanal) Polyp: Report of Case. Journal of Oral Surgery, 26, 588-592.
- Balfour, R.S. (1977) Nasoalveolar Cyst. J MD State Dent Assoc, 20, 92-94.
- Seward, G.R. (1962) Nasolabial Cysts and Their Radiology. Dent Pract, 12, 154-161.
- Pereira Filho, V.A., Silva, A.C., Moraes, M., Moreira, R.W. and Villalba, H. (2002) Nasolabial Cyst: Case Report. Brazilian Dental Journal, 13, 212-214. http://dx.doi.org/10.1590/S0103-64402002000300015
- Allard, R.H.B. (1982) Nasolabial Cyst. A Review of the Literature and Report of Cases. Int J Oral Surg, 11, 351-359.
- Brandão, G.S., Ebling, H. and Souza, I.F. (1974) Bilateral Nasolabial Cyst. Oral Surgery, Oral Medicine, Oral Pathology, 37, 480-484. http://dx.doi.org/10.1016/0030-4220(74)90124-8
- López-Ríos, F., Lassaletta-Atienza, L., Domingo-Carrasco, C. and Martinez-Tello, F.J. (1997) Nasolabial Cyst: Report of a Case with Extensive Apocrine Change. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 84, 404-406. http://dx.doi.org/10.1016/S1079-2104(97)90039-1