International Journal of Clinical Medicine
Vol.5 No.10(2014), Article
ID:46216,5
pages
DOI:10.4236/ijcm.2014.510080
A Cognitive Behavioural Intervention for the Treatment of Vasovagal and Unexplained Syncope
France Bedard1,2, Andre Marchand2,3, Teresa Kus4, Bernard Thibault5, Bianca D’Antono1,6*
1Research Center, Montreal Heart Institute, Montreal, Canada
2Psychology Department, University of Quebec in Montreal, Montreal, Canada
3Research Center of Montreal of Mental health University Institute, Montreal, Canada
4Cardiology Department, Hôpital du Sacré-Coeur de Montréal, Montreal, Canada
5Electrophysiology Service, Montreal Heart Institute, Montreal, Canada
6Psychology Department, University of Montreal, Montreal, Canada
Email: *bianca.d.antono@umontreal.ca, marchand.andre@uqam.ca
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 19 March 2014; revised 18 April 2014; accepted 12 May 2014
ABSTRACT
Vasovagal syncope and unexplained syncope are the most commonly observed types of syncope in outpatient and hospital settings. Medical interventions usually target at the physiological mechanisms responsible for loss of consciousness in an attempt to limit the frequency of recurrences. However, this type of intervention does not take into account the psychological and functional impact of syncope, nor the importance of psychological variables in triggering and maintaining syncope. In the present pilot study, four participants presenting significant psychological distress and recurrent syncope were treated using a multimodal intervention targeting at both the medical and psychological aspects of the problem. Results showed a significant reduction in the frequency of syncope/presyncope, in the level of emotional distress experienced, as well as improved functional status in three of the four participants. Several recommendations are made to medical practitioners and psychologists, in view of identifying patients likely to benefit from this type of intervention or components thereof.
Keywords:Syncope, Cognitive Behavioural Intervention, Psychological Distress, Functional Status

1. Introduction
Syncope refers to a transient loss of consciousness and postural tone [1] . It can be preceded by presyncope characterized by prodromes such as dizziness, sweating/hot flashes, weakness or nausea [1] . Life-time prevalence of syncope is established at 35% in individuals over 65, with recurrences occurring in nearly 35% of patients [2] [3] . In the United States, it accounts for 1% to 6% of hospital admissions, and 3% of visits to the emergency department [3] .
Syncope can be of cardiac, neurological, metabolic or respiratory origin, or can result from use of certain medications [4] . Vasovagal syncope (VVS) is the most common type of diagnosed syncope (approximately 35% of cases) and is due to a dysregulation of the autonomic nervous system [4] . However, the sporadic nature of syncopal episodes often makes it difficult to establish a diagnosis using standard tests. As a result, an afflicted individual may wait several years before receiving a diagnosis. In the interim, syncope is likely to be classified as unexplained (US) [4] -[6] . In about 25% to 30% of cases of US, a diagnosis of VVS will eventually be established [5] [6] .
1.1. Consequences of Vasovagal Syncope and Unexplained Syncope
While VVS and US are not generally life-threatening, they place a high economic burden on the healthcare system [7] [8] . They also have considerable impact on the personal, social and professional lives of afflicted individuals. In fact, patients report that loss of consciousness interferes with their daily activities such as driving, keeping a job and enjoying an active life [9] . In a study conducted by St-Jean and colleagues [10] , 44% of patients with recurrent VVS or US had sustained an injury during a fainting episode, involving bruising (32%), lacerations (9%), fractures (8%) and serious internal injuries (10%).
Moreover, St-Jean and colleagues [10] reported a marked decrease in general quality of life in this population, particularly in the leisure, affective and cognitive performance domains. Given these functional difficulties, it is not surprising that a substantial number of patients reported experiencing significant psychological distress [11] . Moreover, the severity of psychological distress reported by these patients predicted further syncope recurrence and, consequently, seems to contribute to the maintenance of these difficulties [11] -[14] .
1.2. Triggers of Vasovagal Syncope and Unexplained Syncope
Certain situations are recognised by health specialists as conducive to fainting episodes, because they stimulate sympathetic and/or parasympathetic nervous system activity responsible for syncope. These situations include the sight of blood, medical and dental procedures, exposure to heat, prolonged periods in static positions, and excessive alcohol intake [15] [16] . The same physiological systems are also activated in emotional or social situations requiring acute mobilisation of the individual [17] . Patients frequently associate particular emotions (e.g., fear, anger, sadness) or situations with the onset of their symptoms. These situations include an anticipated physical threat (e.g., pain, needles, blood), psychological threat (e.g., fear of humiliation, loss of status) or concern about the possible consequences of fainting episodes (e.g., injury, fear of death or fear of losing control) [15] -[17] .
1.3. Factors Triggering Vasovagal Syncope and Unexplained Syncope Recurrence
Although intense emotions and specific situations can trigger syncope, patients can sometimes confuse certain harmless physiological sensations (e.g., increased heart rate and breathing rate, trembling) with signs of impending syncope [18] [19] . In an effort to prevent further fainting episodes, some patients become hypervigilant with respect to their physical sensations, attempting to recognize symptoms that may signal an impending syncope [20] [21] . Patients may also anxiously anticipate the occurrence of another syncope for days, and avoid situations potentially associated with syncope-related sensations (e.g., physical exercise, particular places, social situations). These behaviours can have a number of negative consequences on patients’ lives, such as increased anxiety or psychological distress, as well as impaired functioning in a variety of domains.
Moreover, apprehension, hypervigilance and fear of relapse can increase patients’ level of physiological arousal and lead to real symptoms of syncope, thereby validating their need to remain hypervigilant and fearful of certain interceptive stimuli or situations. These reactions contribute to creating a vicious cycle involving psychological factors, functioning and physiological sensations/symptoms [18] [19] . In short, evidence suggests that patients’ beliefs, emotions and behaviours in relation to their syncope constitute important variables in the development and maintenance of the difficulties observed in this population.
1.4. Treatment for Vasovagal Syncope and Unexplained Syncope
Several studies have examined the efficacy of both conventional and complementary treatments in reducing the recurrence of syncope in patients presenting with VVS [22] . For US, no clinical studies have been undertaken, and as such, there is no currently recognised treatment for this population [23] . Conventional treatments for VVS include medication, education and, in severe cases, a pacemaker for patients with significant bradycardia [22] . Complementary treatments include orthostatic training, applied tension and psychologically oriented interventions (e.g., cognitive-behavioural strategies) [22] . To date, education and applied tension have proven effective in reducing syncope occurrence [23] .
Education is a simple and safe strategy that can benefit patients with VVS [24] . It is recommended as an initial intervention by the European Task Force on Syncope [22] . The aim of this strategy is to inform patients of the benign nature of the disorder, and to demystify the underlying physiological mechanisms responsible for their fainting [24] . As education was usually included as a control condition in studies examining other interventions, to our knowledge, only one study to date has specifically and directly examined the therapeutic impact of education on the frequency of syncope occurrence [25] .
However, the education protocol also involved instruction in various manoeuvers, such as applied tension, manoeuvres to be performed in cases of presyncope. Thus, the differential impact of information versus the manoeuvres is difficult to distinquish. Moreover, a study conducted by D’Antono and her colleagues [11] suggests that education provided following a diagnosis of VVS does not appear to reduce psychological distress in patients with this condition. This may reflect of lack of consideration, during education sessions, for psychological factors that can trigger or maintain VVS and US recurrence or associated difficulties. Even when discussed, patients do not necessarily receive additional tools in coping with these psychological difficulties.
Applied tension is another strategy that can be helpful to patients presenting a prodromal phase prior to loss of consciousness [22] . This intervention consists of simultaneous contractions of the leg and arm muscles, that the patient is required to begin as soon as the first symptoms of pre-syncope appear. While breathing normally, the patient contracts his muscles for 10 seconds, then releases them for 5 seconds, and begins again until the symptoms disappear. Applied muscle tension increases blood pressure, presumably reducing the effects of the autonomic reflex that precedes fainting [26] [27] . The optimal use of this strategy entails first identifying the onset of a prodromal phase before loss of consciousness. However, one third of patients had seen for syncope in a hospital department or outpatient clinic report experiencing no prodromal symptoms prior to fainting. The extent to which they can benefit from this procedure may therefore be more limited [28] .
Finally, the consequences of fainting (e.g., psychological distress, impaired functioning, reduced quality of life) and the presence of psychological factors that trigger or maintain syncope recurrence (e.g., emotions, hypervigilance, beliefs, avoidance) have led a few investigators over the past decade to examine the efficacy of cognitive-behavioural strategies (e.g., relaxation, cognitive restructuring and gradual exposure for patients with VVS) in reducing syncope recurrence [29] -[31] . These were for the most part small observational case studies, with short follow-up periods (generally less than 6 months), that unfortunately provided limited details regarding the population examination, and the interventions proposed to patients [23] .
1.5. Towards a Multimodal Treatment for Patients with Vasovagal Syncope and Unexplained Syncope
For patients with VVS who experience little psychological distress and present identifiable precipitating factors or a prodromal phase before loss of consciousness, unimodal interventions (e.g., education, applied tension) may be sufficient for satisfactory management of syncope [22] [23] . However, patients with VVS and US presenting impaired functioning or significant psychological distress are likely to benefit from multimodal intervention if their needs are to be met adequately.
In fact, VVS patients without prodromes before fainting episodes have rarely been the subject of studies on the behavioural or psychological treatment of syncope. Patients with US, for their part, do not currently benefit from any recognised and effective treatment [23] . Nonetheless, patients with VVS and US present certain similarities in terms of how they cope at a cognitive, emotional and behavioural level, and may therefore benefit from the same treatment strategies. This is all the more true that a notable percentage of individuals with US are ultimately diagnosed with VVS.
Moreover, many patients with VVS or US report experiencing significant psychological distress or impaired functioning that are not suitably addressed by education or applied tension [9] [11] [32] . A multimodal intervention for these populations should ideally contribute to improved management of syncope by focusing on the psychological consequences, triggers and maintenance of syncope recurrence [23] .
2. Method
2.1. Objective of the Study
The purpose of the present exploratory Phase 1 study is to address certain methodological lacunae in previous studies, and to evaluate a structured multimodal strategy aimed at helping patients better manage their VVS or US and the psychological distress associated with it. To our knowledge, this is the first study examining a treatment for both VVS with or without a prodromal phase, and for US. The following hypotheses are presented: 1) the participants’ symptoms and the number of syncope/presyncope will show clinically and statistically significant reductions following treatment; 2) participants will report a statistically significant reduction of their anxiety and symptoms of depression following the therapeutic sessions; 3) participants will see their quality of life and their psychosocial functions improve following the intervention; 4) the improvements will be maintained at a 6-month follow-up, demonstrating stability over time.
2.2. Participants
Four participants with a VVS or US diagnosis participated in this study. To be eligible, participants had to be between 18 and 65 years of age and present recurrent VVS or US, involving at least two syncopal episodes, with or without a prodromal phase, occurring over the past two years. The VVS diagnosis was confirmed on the basis of medical expertise and/or via medical tests. Syncope was labelled “unexplained” when medical tests failed to confirm another diagnosis. Finally, during the initial telephone contact, participants had to report that their syncope adversely affected their psychological functioning and their daily lives. Participants were excluded from the study either after this initial contact or in the course of the intervention for the following reasons: 1) if their fainting episodes were diagnosed as originating from a) cardiac dysfunction; b) hypersensitivity of the carotid sinus; c) the presence of an auriculoventricular block, or d) epilepsy; 2) if they suffered from a serious physical or psychological disorder (e.g., deafness, chronic pain, cancer, schizophrenia); 3) if they could not understand or complete the questionnaire and, finally; 4) if no significant distress was observed at the beginning of the treatment Twenty-two patients were referred for the study (see Figure 1 for flow chart). Five patients refused to participate, and four were excluded after the initial contact. Out of the 13 patients who partook in the initial telephone contact, four were retained and became participants in the present study (see Table 1 for baseline characteristics of patients enrolled in the study).
Two types of recruitment procedures were used to enroll participants in the study. First, cardiologists at the Montreal Heart Institute and the Hôpital du Sacré-Coeur de Montréal referred patients with a VVS or US diagnosis to the research team. A research assistant then contacted potential participants by phone so as to explain the specifics of the tudy in greater detail. The second approach consisted of mailing a letter describing the study to patients that had been diagnosed with either a VVS or US during the year prior to the study. The names of these patients were obtained by consulting the medical records of potential participants. These individuals were invited to contact the research assistant to obtain more information about the project.
3. Measures
The sociodemographic/medical questionnaire and the self-administered questionnaires were completed by participants two weeks before and after treatment, as well as at the 6-month follow up. Each participant was asked to take notes in a self-monitoring booklet in order to record data daily for the entire duration of treatment, and during the two weeks prior to the post-treatment evaluation, and the 6-month follow-up.
3.1. Self-Monitoring Booklet
Daily self-observations were made using a scale ranging from 0 to 100. These observations were used to establish
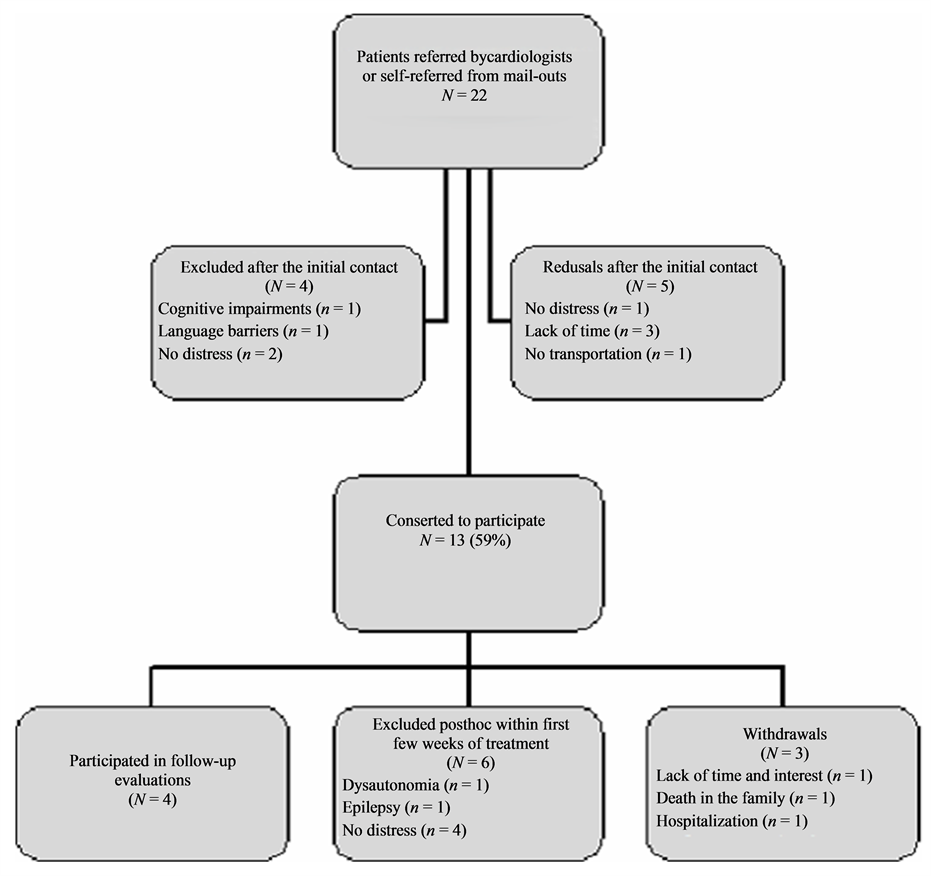
Figure 1. Flow of patients in the study.
Table 1. Case series of four patients with VVS or US referred for cognitive behavioural intervention.
Note. P = Participant; F = Female; M = Male; VVS = Vasovagal Syncope; US = Unexplained Syncope.
a baseline level before treatment (two weeks duration), as well as to make daily assessments during the multimodal intervention. The observations concerned: 1) the frequency of syncope and presyncope occurrence; 2) the degree of worry concerning the consequences of their syncope and presyncope; 3) the degree of hypervigilance in regard to physical sensations.
3.2. Symptom and Other Measures
Sociodemographic and medical questionnaire. This questionnaire records information about the participant’s age, sex, marital status, level of education, personal and family income, frequency of syncope and presyncope during the last few months/years, and personal and family medical history.
Anxiety Sensibility Index (ASI) [33] . This self-administered 16-item questionnaire evaluates fear related to the physical symptoms of anxiety, and the beliefs concerning the social and physical consequences of the symptoms. The questionnaire has good internal consistency (0.87) and temporal stability over a three-week period (0.91).
Beck Anxiety Inventory (BAI) [34] . This inventory consists of 21 items and measures cognitive, affective, and physical symptoms that have been present in the previous week. Internal consistency varies from 0.84 to 0.93, and temporal stability over 4 weeks attains 0.63 in a cohort of students [35] .
Beck Depression Inventory-II (BDI-II) [36] . This 21-item questionnaire measures the presence and intensity of depressive symptoms in the previous week. Temporal stability at 4 months is 0.62, and internal consistency varies from 0.90 to 0.92 [37] .
Current functioning evaluation questionnaire (CFE) [38] . This unpublished questionnaire measures the intensity of the difficulties encountered by the participant over the past two weeks in seven areas of his or her life: professional activities, education, marital relations, family relations, social life, leisure and daily activities. Although this questionnaire has not been validated, it is easy to complete and provides a global evaluation of psychological functioning SF-12 health-related quality of life questionnaire (SF-12) [39] . This 12-item questionnaire is composed of two subscales and measures quality of life in relation to physical and mental health. It has an established test-retest reliability (0.85) [36] , structural validity [40] , and internal consistency [41] .
3.3. Treatment
The first component of the intervention consisted of psychoeducation, and sought to help participants understand the biological mechanisms triggering syncope, to identify possible precipitating factors, and to make life style changes designed to prevent relapse. At this stage, participants were also informed that beliefs, emotions and behaviours constitute important variables in the development and maintenance of their difficulties. The second component of the intervention addressed different ways of modifying cognitive and behavioural factors that are likely involved in either aggravating or maintaining the participants’ difficulties. They were taught several techniques that they were encouraged to practice at home to better manage their emotional and physical symptoms. These included breathing retraining, progressive muscle and passive relaxation techniques, and problem solving, with the aim of reducing daily stress levels and negative emotions experienced by participants. Similarly, the use of strategies like cognitive restructuring, and in vivo exposure was intended to modify dysfunctional beliefs, as well as reduce avoidance and escape behaviours that are frequently adopted by participants in response to fainting episodes. Finally, although the applied tension technique was initially designed to be used by patients with VVS preceded by prodromes, this technique was taught to all participants. This was done given that participants without prodromes may actually present subtle symptoms that would become identifiable after a session of psychoeducation, and because participants with US may eventually receive a diagnosis of VVS (as was the case here).
An independent psychologist specialised in cognitive-behavioural therapy and trained in the treatment of syncope, administered the treatment. She was not involved in study design or analysis of results. She followed the instructions that were presented in a treatment manual. The latter provided a summary for the content of each session and described the components and intervention strategies of the multimodal treatment. Moreover, participants were given a Participant’s Manual containing the detailed information presented in the sessions.
3.4. Procedures
This study used a single-case protocol based on ending the intervention after a certain period (AB). The protocol comprises a baseline period and ends once the intervention has been completed. This type of protocol is often used in cases where the effect of the intervention is not reversible, such as the acquisition of a new ability. Participants were evaluated at three points in time: before the start of the intervention (T0: pre-test), at the end of the intervention (T1) and at 6-month follow-up (T2).
At their first visit to the Montreal Heart Institute or the Hôpital du Sacré-Coeur de Montréal, participants read and signed a consent form, and authorised the audio recording of the sessions. They were asked to complete a sociodemographic/medical questionnaire and several self-report questionnaires (T0). They were also given a self-monitoring booklet to fill out daily, for a period starting two weeks prior to treatment and ending two weeks after the end of treatment, in order to obtain a continuous evaluation of syncope symptoms, presyncope, anxiety, and depression.
The minimal baseline period was 14 days. The first meeting with the therapist took place when symptom stability or worsening was observed in a participant (based on the self-monitoring booklet) in the preceding 14 day-period. These participants then began a standardized 7-week therapy program with the therapist in person. For two weeks after the last session (T1) and at the 6-month follow-up (T2), participants once again filled out their self-monitoring booklets daily. With the exception of the medical questionnaire which was completed via a short interview by telephone, the subsequent interview, i.e. the 6-month follow-up, was completed by mail (T2). The therapy sessions were taped in order to evaluate treatment integrity. Random audits of 25% of each participant’s sessions ensured that the intervention themes were covered during the sessions. Treatment integrity was rated at 99%. Authorisation from both institutions’ Ethics Committees was obtained.
4. Results
With respect to the self-monitoring booklets, only measures relating to worries and hypervigilance were retained as dependent variables (DV), to establish baseline levels for patients and observe their progression during the course of the intervention (IV). These variables have previously been associated with the development and maintenance of syncope, as well as with impaired functioning. With the exception of results for the repeated measures analysis of variance, the results are presented on an individual basis.
4.1. Daily Self-Observations
Figures 2-5 present the fluctuations in the levels of hypervigilance to physical sensations reported by participants throughout the study. The raw data was smoothed by calculating a mean of the seven daily measures for a given week. Visual analysis revealed a positive baseline trend for three participants (P2, P3 and P4), which reflects a moderate increase in hypervigilance to physical sensations during the two weeks prior to the beginning of the intervention. For P1, although hypervigilance to physical sensations seemed to decrease prior to treatment, a separate measure of the intensity of worry about the consequences of future syncope showed an ascending trend, making this patient eligible for the study. The data regarding worry is similar to that related to hypervigilance. We did not consider it essential to include these charts, given their similarity.
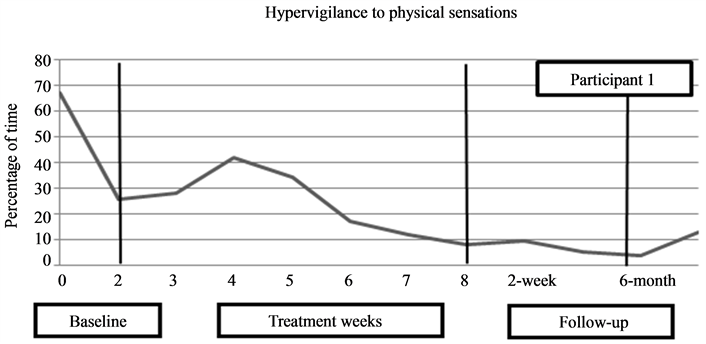
Figure 2. Fluctuations in the level of hypervigilance to physical sensations reported by P1.
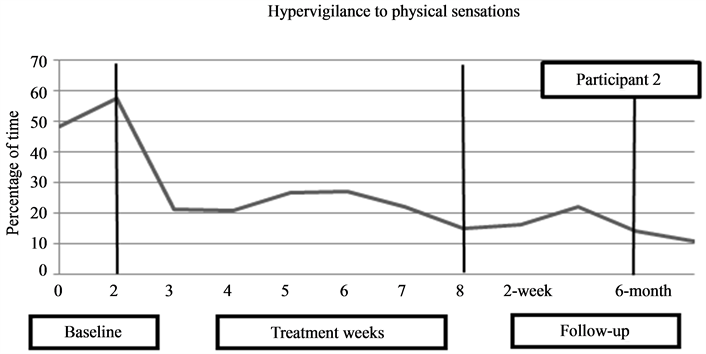
Figure 3. Fluctuations in the level of hypervigilance to physical sensations reported by P2.
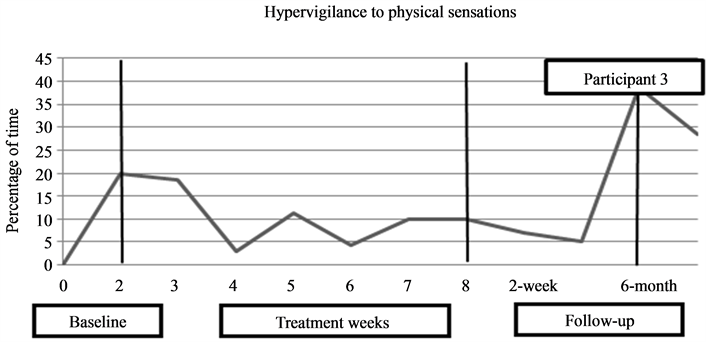
Figure 4. Fluctuations in the level of hypervigilance to physical sensations reported by P3.
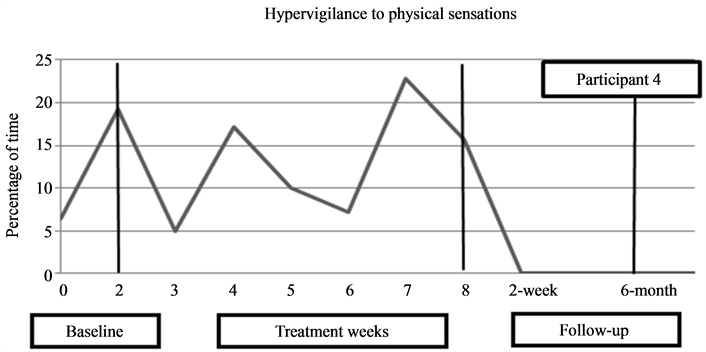
Figure 5. Fluctuations in the level of hypervigilance to physical sensations reported by P4.
Visual observation indicated a significant reduction in the duration of hypervigilance to physical sensations in all participants, with the exception of P3, who showed an increase by the 6-month follow-up despite modest reductions initially observed during the post-test. For P1, the mean duration of time spent being hypervigilant was 47% at pre-test and fell to 7% at post-test, and to 9% at 6-month follow-up. For P2, the mean duration of hypervigilance was recorded at 54% at pre-test, 19% at post-test, and 13% at 6-month follow-up. As for P3, the mean duration of hypervigilance was 10% at pre-test, 6% at post-test and 34% at the 6-month follow-up. Finally, P4 presented a mean duration of 13% at pre-test, and of 0% at both post-test and 6-month follow-up. The general trend showed clinical improvement in the duration of time spent being hypervigilant to physical sensations.
4.2. Number of Syncope and Presyncope
The self-monitoring booklets indicate, that for 3 out of the 4 participants (P1, P2 and P4), there was a notable reduction in the number of syncope and pre-syncope experienced post-treatment and at 6 month follow-up. No significant change was observed for P3 (see Table 2).
4.3. Self-Report Questionnaires
Clinical change index (CCI). The scores obtained at post-test and at 6-month follow-up for all five self-report questionnaires (ASI, BAI, BDI, CFE, SF-12) were used to create a C index [41] (see Table 3). A cut-off point
Table 2 . Number of syncope and presyncope at pretest, post-test and 6-month follow-up (N = 4).
Note. P1 = Participant 1; P2 = Participant 2; P3 = Participant 3; P4 = Participant 4.
Table 3. Cutoff point C for each questionnaire, reliable change index and results obtained for each of the five secondary measures.
Note. ASI = Anxiety sensibility index; PSF-12 = SF-12 physical health composite scale; MSF-12 = SF-12 mental health composite scale; BDI-II = Beck depression inventory II; BAI = Beck anxiety inventory; P1 = Participant 1; P2 = Participant 2; P3 = Participant 3; P4 = Participant 4. aThreshold for a value to be considered non-clinical was reached. bThreshold for a change score (compared to baseline) to be considered statistically reliable was reached.
was used to determine whether a level of improvement was clinically significant in relation to the pre-test score. The cut-off point for a particular questionnaire was defined on the basis of score distributions obtained by functional and dysfunctional populations on that same questionnaire. Table 3 presents participants’ results for all measures at pre-test, post-test, and 6-month follow-up. P1, P2 and P4 reached a nonclinical level of functioning on two measures at post-test, and on three to four measures at the 6-month follow-up. P3 only showed significant improvement on the ASI. It should be noted that at pre-test, P3 and P4 showed nonclinical levels on the BAI and ASI respectively, and as such, no significant improvement could be observed on either of these measures.
Reliable change index (RCI). This index makes it possible to evaluate, for each questionnaire, whether the change recorded by the CCI is considered statistically reliable when a comparison is made between the post-test/follow-up and the pre-test [42] (see Table 3).
The cut-off point used for this study is 1.54, which corresponds to a unilateral 95% confidence interval. Table 3 presents the results obtained for each of the five secondary measures. Statistically significant improvements were observed at post-test for one to two questionnaires, and for three to four questionnaires at the 6-month follow-up for P1, P2 and P4. With the exception of the ASI at follow-up, no statistically significant improvement was noted for P3.
Global functioning index. In order to calculate the global functioning index at post-test and at follow-up, a composite score was obtained based on seven pre-selected criteria: 1) 50% reduction in the number of syncope and presyncope; 2) at least 50% reduction in self-observation data concerning hypervigilance to physical sensations; 3) presence of nonclinical level or significant change on the ASI; 4) presence of nonclinical level or significant change on the BAI; 5) presence of nonclinical level or significant change on the BDI-II; 6) presence of nonclinical level or significant changes in the physical aspects of health on the SF-12; 7) presence of nonclinical level or significant change in the mental aspects of health on the SF-12. The number of items for which a specific criterion is attained determines the level of global functioning: low (0 - 1 item), moderate (2 - 3 items), high (4 - 5 items), very high (6 - 7 items). Taking these criteria into account, results indicated a high level of functioning at post-test for P1, P2 and P4. This improvement was even more marked at 6-month follow-up for P1 and P4, who achieved a very high level of functioning, and a high level of functioning was sustained for P2. However, for P3, the level of functioning remained low at the two testing periods, with a composite score of zero at post-test and a score of one at the 6-month follow-up.
Variance analysis. Repeated measures analyses of variance (ANOVA) were performed to evaluate the scores obtained at the different testing periods. Despite the small number of participants, the BAI showed a significant effect. Trends for the treatment effect were also observed for the ASI, SF-12, BDI and CFE. The Eta-squared coefficients were found to be between 0.32 and 0.62, values indicating large effect sizes according to Cohen [42] . Table 4 presents the means and standard deviations for participants at pre-test, post-test and 6-month follow-up, as well as values for the analyses of variance.
Table 4 indicates a marked decrease in symptoms of anxiety and depression reported by patients from pre-test to post-test. This decrease was slightly more pronounced at the 6-month follow-up for the ASI and the BDI. With regard to global functioning and quality of life, participants showed improvement for both the CFE and the SF-12 at post-test, and improved further at 6-month follow-up. In summary, the proposed multimodal intervention appears to have produced significant therapeutic gains over time.
Table 4. Means, standard deviations and analyses of variance results obtained for each questionnaire (N = 4).
Note. ASI = Anxiety sensibility index; SF-12 = Health-related quality of life questionnaire; BDI-II = Beck depression inventory; BAI = Beck anxiety inventory; CFE = Current functioning evaluation; P1 = Participant 1; P2 = Participant 2; P3 = Participant 3; P4 = Participant 4. *p < 0.05.
5. Discussion
To our knowledge, this is the first study to evaluate the efficacy of an innovative multimodal treatment adapted to both VVS with or without a prodromal phase, and to US. In regards to our hypothesis, the results show that three out of the four participants improved the following treatment. First, they showed a significant decrease in the number of syncope or presyncope that they experienced. Furthermore, their distress levels decreased and their level of functioning improved both statistically and clinically after the intervention. Participants attained either high or very high levels of global functioning.
Moreover, this treatment resulted in a significant decrease in hypervigilance to physical sensations and in worry related to loss of consciousness. The changes observed at post-test were sustained at the 6-month follow-up, except for P3. It must be noted that this participant had lost his job a short time prior to the 6-month assessment, and this event had probably affected the participant’s level of psychological distress and level of functioning. Moreover, several interpersonal difficulties mentioned by the participant during the therapeutic intervention were not addressed directly in therapy and may have contributed to his poorer outcome.
Our findings compare rather favourably to those studies evaluating the efficacy of education and applying tension for VVS [23] . In fact, our results show a reduction of nearly 65% in the occurrence of syncope in three of the four study participants, compared to a 35% to 60% reduction in previous studies. The intervention used in the current study was specifically adapted to individuals presenting significant psychological distress related to their syncope, and individuals who may typically show greater resistance to conventional treatment. Out of the 22 patients referred to the researchers, 15 patients, that is, 68%, reported significant psychological distress at initial contact. This percentage is comparable to findings of previous studies in this and other settings [9] [11] [32] . It is important to note that treatment adherence was very high: the four participants were committed to the daily home exercises, participated during the intervention sessions, and indicated using the strategies on a regular basis.
To our knowledge, no study reviewed in the literature has measured the clinical impact of the intervention strategies used to relieve psychological distress and improve global functioning across different domains of functioning in the patients [23] . These studies have typically focused on evaluating the number of syncope and presyncope before and after treatment and, in a few cases, evaluated the functioning of participants based on whether or not they returned to work/school after treatment [23] [29] [30] [43] . Our study is innovative in that it examines the evolution across time of several difficulties associated with the recurrence of fainting episodes, namely hypervigilance, worries and avoidance behaviours.
Despite these promising results, the individual case protocol used in this study presents certain limitations. Since participants are used as their own controls, the protocol is considered pre-experimental [44] [45] . Starting treatment after a 14-day baseline period makes it possible to draw certain inferences regarding the efficacy of the intervention on the different variables of interest in this study [44] [45] . However, the chosen protocol has reduced validity and does not rule out the role of factors related to maturation, simple reassurance, and the natural fluctuation of symptoms. In addition, the protocol allows little generalisation of results, given the small number of participants. Moreover, the recruitment process employed limits the conclusions we can draw regarding our participants and our results. We had a notable number of refusals (23%), withdrawals, and exclusions from the study. Moreover, no data is available on the number of patients that had been approached by the cardiologists at the two recruitment sites, or on the initial level of distress noted in the target population at the time of solicitation. Therefore, the 22 patients initially referred to us, or solicited by consulting medical records, may not be entirely representative of the intended target population for the present study.
Nonetheless, this study presents certain methodological strengths, which include: continuous and prospective measures, the use of a manual for participants, the use of a standardised treatment protocol, evaluation of the treatment, and the use of valid clinical measurements, as well as the inclusion of a 6-month follow-up. It should be noted that the considerable improvements noted on the global functioning index are based on criteria considered conservative. Moreover, at post-test, patients evaluated the relevance of the strategies used to reduce their syncope-related difficulties at 90%. In fact, these patients reported having particularly benefited from psychoeducation, applied tension, and from strategies of cognitive restructuring and gradual exposure.
Given the exploratory nature of the present study, further research should be conducted to support these findings, and to provide confirmation of the efficacy of the multimodal intervention. Depending on recruitment possibilities, individual case protocols with multiple baseline periods, or semi-experimental and experimental studies with larger cohorts will make it possible to evaluate the relative efficacy of the intervention. To be prioritised are “no treatment”, “waiting list”, or “active single modality treatment (e.g., applied tension, education control groups)”. This would facilitate the evaluation of influences from variables that are not specific to the intervention as well as the assessment of the relative contribution of each strategy to the overall efficacy of the intervention. In this regard, it would be of interest to compare intervention strategies based on the specific needs of patients, in order to provide the shortest and most suitable treatment possible (e.g., target hypervigilance in patients who are acutely aware of physical sensations, promote exposure for patients whose preferred adaptive strategy is avoidance). We must point out that these recommendations apply to a setting in which participant recruitment is satisfactory. However, given that the present study encountered several obstacles at the level of recruitment, larger-scale studies will undoubtedly experience similar difficulties.
Nonetheless, the results of the present study are encouraging, and suggest that innovative and appropriate treatment approaches could provide additional therapeutic options for clinicians. For a number of patients with little or no psychological distress, conventional treatment using psychoeducation and applied tension may be sufficient, and has demonstrated good efficacy in various studies on the subject. Several of the participants that had been solicited for this study and who either withdrew from treatment at the beginning, or who were excluded during initial telephone contact, may have belonged to this category of patients.
However, certain patients experience more serious difficulties despite the conventional treatments offered in hospital settings; these patients need complementary treatment. While one participant (P2) did show consistently reduced hypervigilance following the psychoeducation component of our study, it is impossible to determine whether this change was a result of the education component, or rather from other aspects of the intervention, such as self-observation, reassurance from the therapist, or the knowledge that she would receive care tailored to her needs over several months to come. Moreover, we have previously shown that education regarding syncope provided by a medical practitioner following head-up tilt testing is not sufficient to significantly reduce the psychological distress reported by many patients with VVS or US [11] .
Distressed patients present certain characteristics which ideally need to be recognised by the treating physician, such as fear of the possible consequences of syncope, hypervigilance to physical sensations, behavioural restrictions related to fainting, as well as symptoms of anxiety and depression. For these patients, additional strategies more commonly associated with cognitive and behavioural therapies may be useful, as suggested here, in conjunction with medical treatment.
However, patients are not always aware of the psychological and functional impact of syncope episodes in their daily lives. They may underestimate the cognitive and behavioural changes that occur following the onset of syncope, and thus remain unaware of the additional effects of these factors. In the current study, despite a high level of distress observed at the initial interview, a number of potential participants refused to participate in the research due to unwillingness to commit to a seven session treatment that addresses, most notably, the functional aspects of the problem. These participants judged their distress level insignificant compared to the required commitment to the program. This highlights the need for medical professionals not only to be attentive to possible psychological and functional distress in patients with VVS and US, but also the important role they may need to play in educating their patients about the importance of this distress to their health problem. It would be ideal to offer (refer to) complementary interventions when additional psychological or functional difficulties contribute to maintaining the patient’s problem.
In addition, some patients seen in a hospital setting may have additional difficulties (e.g., relationship or family problems) that could contribute to the onset of fainting episodes or, in turn, be aggravated by these episodes. In these cases, referring patients to psychological resources that are better able to address these additional issues becomes highly pertinent, as an adjunct to medical treatment.
It is worth mentioning that psychologists working in both public and private sectors are also little informed of the psychological dimension of syncope. Psychologists frequently teach their clients that loss of consciousness and the presence of anxiety disorders, particularly panic attacks, are incompatible [23] . This information is clearly erroneous, at least in a subgroup of anxious patients. It is imperative that psychologists recognize that they may encounter patients for whom VVS or US may contribute to, complicate, maintain, or accompany mental illness or other acute psychological difficulties. In such cases, we encourage mental health professionals to use one or several of the therapeutic approaches examined in the study to complement their own interventions.
At present, patients experiencing syncope are rarely referred for psychological consultation, even when significant psychological distress is present [11] . The present study demonstrates the positive impact of cognitive and behavioural interventions in reducing distress and improving the global functioning of participants, in addition to reducing syncope. It is hoped that further research concerning the efficacy of interventions for VVS and US patients will lead to the elaboration of improved guidelines for their treatment.
Acknowledgements
This research was made possible as a result of an education grant offered by Biotronik to T. K. and B. D.A., as well as financial support provided by the Fondation de l’Institut de Cardiologie de Montréal (FICM) awarded to B.DA. F. B. was a recipient of a doctoral award from the Fonds de la recherche sur la santé et de la culture (FQRSC), while B.D.A. was a recipient of a Chercheur Boursier Junior 2 award from the Fonds de la recherche en santé du Québec (FRSQ). Finally, we wish to acknowledge the collaboration of the various cardiologists specializing in electrophysiology at the Montreal Heart Institute and the Hôpital Sacré-Coeur de Montréal for their implication in this project.
References
- Sheldon, R., Koshman, M.L., Wilson, W., Kieser, T. and Rose, S. (1998) Effect of Dual-Chamber Pacing with Automatic Rate-Drop Sensing on Recurrent Neurally Mediated Syncope. The American Journal of Cardiology, 81, 158-162. http://dx.doi.org/10.1016/S0002-9149(97)00891-6
- Olde Nordkamp, L.R.A., van Dijk, N., Ganzeboom, K.S., Reitsma, J.B., Luitse, J.S.K., Dekker, L.R.C., et al. (2009) Syncope Prevalence in the ED Compared to General Practice and Population: A Strong Selection Process. The American Journal of Emergency Medicine, 27, 271-279. http://dx.doi.org/10.1016/j.ajem.2008.02.022
- Savage, D.D., Corwin, L., McGee, D.L., Kannel, W.B. and Wolf, P.A. (1985) Epidemiologic Features of Isolated Syncope: The Framingham Study. Stroke, 16, 626-629. http://dx.doi.org/10.1161/01.STR.16.4.626
- Mathias, C.J., Deguchi, K. and Schatz, I. (2001) Observations on Recurrent Syncope and Presyncope in 641 Patients. Lancet, 357, 348-353. http://dx.doi.org/10.1016/S0140-6736(00)03642-4
- Krahn, A.D., Klein, G.J., Norris, C. and Yee, R. (1995) The Etiology of Syncope in Patients with Negative Tilt Table and Electrophysiological Testing. Circulation, 92, 1819-1824. http://dx.doi.org/10.1161/01.CIR.92.7.1819
- Krahn, A.D., Klein, G.J., Yee, R. and Norris, C. (1998) Final Results from a Pilot Study with an Implantable Loop Recorder to Determine the Etiology of Syncope in Patients with Negative Noninvasive and Invasive Testing. The American Journal of Medicine, 82, 117-119.
- Calkins, H., Byrne, M., el-Atassi, R., Kalbfleisch, S., Langberg, J.J. and Morady, F. (1993) The Economic Burden of Un-Recognized Vasodepressor Syncope. American Journal of Medicine, 95, 473-479.http://dx.doi.org/10.1016/0002-9343(93)90329-N
- Sun, B.C., Emond, J.A. and Camargo Jr., C.A. (2005) Direct Medical Costs of Syncope-Related Hospitalizations in the United States. American Journal of Cardiology, 95, 668-671. http://dx.doi.org/10.1016/j.amjcard.2004.11.013
- Linzer, M., Pontinen, M., Gold, D.T., Divine, G.W., Felder, A. and Brooks, W.B. (1991) Impairment of Physical and Psychosocial Function in Recurrent Syncope. Journal of the American College of Cardiology, 44, 1037-1043.
- St-Jean, K., Kus, T., Dupuis, G., Levesque, K., Thibault, B. and D’Antono, B. (2009) Quality of Life in Patients with Re-Current Vasovagal or Unexplained Syncope: Influence of Sex, Syncope Type and Illness Representations. Applied Quality of Life Research, 3, 235-249. http://dx.doi.org/10.1007/s11482-009-9058-x
- D’Antono, B., Dupuis, G., St-Jean, K., Lévesque, K., Nadeau, R., Guerra, P. and Thibault, B. (2009) Prospective Evaluation of Psychological Distress and Psychiatric Morbidity in Re-Current Vasovagal and Unexplained Syncope. Journal of Psychosomatic Research, 67, 213-222. http://dx.doi.org/10.1016/j.jpsychores.2009.03.012
- Giada, F., Silvestri, I., Rossillo, A., Nicotera, P.G., Manzillo, G.F. and Raviele, A. (2005) Psychiatric Profile, Quality of Life and Risk of Syncopal Recurrence in Patients with Tilt-Induced Vasovagal Syncope. EP Europace, 7, 465-471. http://dx.doi.org/10.1016/j.eupc.2005.05.008
- Romme, J.J.C.M., van Dijk, N., Go-Schon, I.K., Casteelen, G., Wieling, W. and Reitsma, J.B. (2001) Association between Psychological Complaints and Recurrence of Vasovagal Syncope. Clinical Autonomic Research, 21, 373-380. http://dx.doi.org/10.1007/s10286-011-0125-7
- Kapoor, W.N., Fortunato, M., Hanusa, B.H. and Schulberg, H.C. (1995) Psychiatric Illnesses in Patients with Syncope. The American Journal of Medicine, 99, 505-512. http://dx.doi.org/10.1016/S0002-9343(99)80227-7
- Hupert, N. and Kapoor, W.N. (1997) Syncope: A Systematic Search for the Cause. Journal of Psychosomatic Research, 31, 136-139, 143-146, 149-150.
- Linzer, M., Felder, A., Hackel, A., Perry, A.J., Varia, I., Melville, M.L. and Krishnan, K.R. (1990) Psychiatric Syncope: A New Look at an Old Disease. Psychosomatics, 31, 181-188. http://dx.doi.org/10.1016/S0033-3182(90)72192-5
- Engel, G.L. (1978) Psychologic Stress, Vasodepressor (Vasovagal) Syncope, and Sudden Death. Annals of Internal Medicine, 89, 403-412. http://dx.doi.org/10.7326/0003-4819-89-3-403
- Gracie, J., Baker, C., Freeston, M.H. and Newton, J.L. (2004) The Role of Psychological Factors in the Aetiology and Treatment of Vasovagal Syncope. Indian Pacing and Electrophysiology Journal, 4, 79-84.
- Gracie, J., Newton, J.L., Norton, M., Baker, C. and Freeston, M. (2006) The Role of Psychological Factors in Response to Treatment in Neurocardiogenic (Vasovagal) Syncope. EP Europace, 8, 636-643. http://dx.doi.org/10.1093/europace/eul073
- Bonk, V.A., France, C.R. and Taylor, B.K. (2001) Distraction Reduces Self-Reported Physiological Reactions to Blood Donation in Novice Donors with a Blunting Coping Style. Psychosomatic Medicine, 63, 447-452.
- Steptoe, A. and Wardle, J. (1988) Emotional Fainting and the Psychophysiologic Response to Blood and Injury: Autonomic Mechanisms and Coping Strategies. Psychosomatic Medicine, 50, 402-417.
- Brignole, M., Alboni, P., Benditt, D.G., Bergfeldt, L., Blanc, J.J., Bloch Thomsen, P.E., et al. (2004) Guidelines on Management (Diagnosis and Treatment) of Syncope. Revue Espanola de Cardiologia, 58, 175-193.
- Bedard, F., Marchand, A., Kus, T. and D’Antono, B. (2010) Vasovagal Syncope and Unexplained Syncope: Concepts, Treatments, and Future Perspectives. Canadian Psychology/Psychologie Canadienne, 51, 257-268.
- Wieling, W., Colman, N., Krediet, C.T. and Freeman, R. (2004) Nonpharmacological Treatment of Reflex Syncope. Clinical Autonomic Research, 14, i62-i70. http://dx.doi.org/10.1007/s10286-004-1009-x
- Aydin, M.A., Mortensen, K., Salukhe, T.V., Wilke, I., Ortak, M., Drewitz, I., et al. (2012) A Standardized Education Protocol Significantly Reduces Traumatic Injuries and Syncope Recurrence: An Observational Study in 316 Patients with Vasovagal Syncope. EP Europace, 14, 410-415. http://dx.doi.org/10.1093/europace/eur341
- Croci, F., Brignole, M., Menozzi, C., Solano, A., Do-nateo, P., Oddone, D., Puggioni, E. and Lolli, G. (2004) Efficacy and Feasibility of Isometric Arm Counter-Pressure Manoeuvres to Abort Impending Vasovagal Syncope during Real Life. EP Europace, 6, 287-291. http://dx.doi.org/10.1016/j.eupc.2004.03.008
- Sabin, N. (2001) The Use of Applied Tension and Cognitive Therapy to Manage Syncope (Common Faint) in an Older Adult. Aging and Mental Health, 5, 92-94. http://dx.doi.org/10.1080/13607860020020690
- Alboni, P., Brignole, M., Menozzi, C., Raviele, A., Del Rosso, A., Dinelli, M., Solano, A. and Bottoni, N. (2001) Diagnostic Value of History in Patients with Syncope with or without Heart Disease. Journal of the American College of Cardiology, 37, 1921-1928. http://dx.doi.org/10.1016/S0735-1097(01)01241-4
- McGrady, A.V., Bush, E.G. and Grubb, B.P. (1997) Outcome of Biofeedback-Assisted Relaxation for Neurocardiogenic Syncope and Headache: A Clinical Replication Series. Applied Psychophysiology and Biofeedback, 22, 63-72. http://dx.doi.org/10.1023/A:1026241826589
- McGrady, A.V., Kern-Buell, C., Bush, E., Devonshire, R., Claggett, A.L. and Grubb, B.P. (2003) Biofeedback-Assisted Relaxation Therapy in Neurocardiogenic Syncope: A Pilot Study. Applied Psychophysiology and Biofeedback, 28, 183-192. http://dx.doi.org/10.1023/A:1024664629676
- Newton, J.L., Kenny, R.A. and Baker, C.R. (2003) Cognitive Behavioural Therapy as a Potential Treatment for Vasovagal/Neurocardiogenic Syncope: A Pilot Study. EP Europace, 5, 299-301.http://dx.doi.org/10.1016/S1099-5129(03)00030-8
- Koenig, D., Linzer, M., Pontinen, M. and Divine, G.W. (1992) Syncope in Young Adults: Evidence for a Combined Medical and Psychiatric Approach. Journal of Internal Medicine, 232, 169-176.http://dx.doi.org/10.1111/j.1365-2796.1992.tb00567.x
- Reiss, S., Peterson, R.A., Gursky, D.M. and McNally, R.J. (1986) Anxiety Sensitivity, Anxiety Frequency and the Prediction of Fearfulness. Behavior Research and Therapy, 24, 1-8. http://dx.doi.org/10.1016/0005-7967(86)90143-9
- Beck, A.T., Epstein, N., Brown, G. and Steer, R.A. (1988) An Inventory for Measuring Clinical Anxiety: Psychometric Properties. Journal of Consulting and Clinical Psychology, 56, 893-897.http://dx.doi.org/10.1037/0022-006X.56.6.893
- Beck, A.T. and Steer, R.A. (1993) Manual for the Beck Anxiety Inventory. 2nd Edition, Psychological Corporation, San Antonio.
- Beck, A.T., Steer, R.A. and Brown, G.K. (1996) Manual for the BDI-II. 2nd Edition, Psychological Corporation, San Antonio.
- Bouvard, M. and Cottraux, J. (2005) Protocoles et échelles d’évaluation en psychiatrie et en psychologie. 4th Edition, Masson, Paris.
- Freeston, M. (1998) Questionnaire sur l’évaluation du fonctionnement actuel. Unpublished Manuscript, Centre de recherche Fernand-Seguin de l’Hôpital Louis-H. Lafontaine, Montréal.
- Ware, J.E., Kosinski, M. and Keller, S.D. (1996) A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Medical Care, 34, 220-233.http://dx.doi.org/10.1097/00005650-199603000-00003
- Brazier, J.E., Harper, R., Jones, N.M., O’Cathain, A., Thomas, K.J., Usherwood, T. and Westlake, L. (1992) Validating the SF-36 Health Survey Questionnaire: New Outcome Measure for Primary Care. British Medical Journal, 305, 160-164. http://dx.doi.org/10.1136/bmj.305.6846.160
- Jacobson, N.S. and Truax, P. (1992) Clinical Significance: A Statistical Approach to Defining Meaningful Change in Psychotherapy Research. In: Kazdin, A.E., Ed., Methodological Issues and Strategies in Clinical Research, American Psychological Association, Washington DC, 631-648. http://dx.doi.org/10.1037/10109-042
- Cohen, J. (1988) Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaumm, Hillsdale.
- Ware, J.E., Kosinski, M. and Keller, S.D. (1996) A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Medical Care, 34, 220-233.http://dx.doi.org/10.1097/00005650-199603000-00003
- Cook, T.D. and Campbell, D.T. (1979) Quasi-Experimentation: Design & Analysis Issues for Field Setting. Rand Mc-Nally College Publishing Company, Chicago.
- Ladouceur, R. and Bégin, G. (1986) Protocoles de recherche en science appliquée et fondamentale [Research Protocols in the Applied and Fundamental Sciences]. Edisem, St-Hyacinthe.
NOTES

*Corresponding author.


