World Journal of Cardiovascular Diseases
Vol.3 No.1A(2013), Article ID:29041,8 pages DOI:10.4236/wjcd.2013.31A021
Comparative analysis of the quality of life of heart failure patients in South Western Nigeria
![]()
1Department of Medicine, College of Medicine, University of Lagos, Lagos, Nigeria
2Department of Psychiatry, College of Medicine, University of Lagos, Lagos, Nigeria
3Department of Medicine, Lagos University Teaching Hospital, Lagos, Nigeria
Email: ambakwem@hotmail.com
Received 9 January 2013; revised 12 February 2013; accepted 19 February 2013
Keywords: Comparative; Quality of Life; Heart Failure; South Western Nigeria
ABSTRACT
Background: Heart failure (HF) is a common, chronic clinical syndrome with appreciable impact on both prognosis and lifestyle of patients. Two main aims of management include preventing disease progression and improving quality of life (QoL). Not much work has been done in this area in Sub-Saharan Africa and most of the available disease specific instruments were developed using the Caucasian population. Aim: We therefore evaluated the QoL of stable HF patients attending the cardiology clinic of the Lagos University Teaching Hospital using a disease specific instrument, Kansas City Cardiomyopathy Questionnaire (KCCQ) and a generic one, the WHOQOLBREF. Method: Consenting, stable HF patient were recruited from the cardiology clinic of the Lagos University Teaching Hospital. Relevant clinical data and echocardiographic parameters were retrieved from their clinical notes and the subjects filled out the questionnaires, the KCCQ and the WHOQOL-BREF. The QoL and four main domains in the WHOQOLBREF were compared with scores on the KCCQ for relationships. Result: Data set of 190 patients was analysed. There were 91 (47.9%) males and 99 (52.1%) females with a mean age 51.90 ± 13.21 yrs. Only 52 (27.4%) had college education and 143 (75.2%) had very poor personal resources. About 104 (54.7%) were paying their medical bills themselves. The mean QoL score using the KCCQ score was 59.61 ± 23.80. With The KCCQ, 6.9% felt their QoL was poor and 20% felt it was fair while 11.6% and 20.5% felt their QoL was poor and fair respectively with the WHOQOL-BREF. There was positive correlation, p < 0.0001, between the KCCQ QoL and WHO-BREF QoL scores and the four domains assessed; physical health, psychological, social relationships, environment. Conclusion: Over 25% of HF patients in our environment have unacceptable levels of quality of life which has to be addressed in their management. The generic WHOQOL-BREF would suffice in our environment if the specific HFQoL instruments are not available.
1. INTRODUCTION
Heart failure (HF) is a common, chronic clinical syndrome with appreciable impact on both prognosis and lifestyle of patients [1]. Prevalence in developed countries is approximately 1% - 2% in the adult population and this rises to ≥10% in individuals older than 70 yrs [2]. Two main aims of management include preventing disease progression (hospitalisation, deterioration of left ventricular function and mortality) and alleviating patients suffering which will include the symptoms and signs [3]. Evaluating the latter treatment goals will require use of health-related quality of life (HRQoL) instruments. Information from this type of assessment which is patient centred most times differ from what is obtained from the functional status assessment like the New York Heart Association (NYHA) criteria, which is physician centred [4,5]. The achievements of the latter goals which are of utmost importance to patients have not been the primary outcomes in most trials [6]. Reasons alluded to for this has been difficulty with measurement of these outcomes and that some treatments previously shown to improve these parameters also decreased survival [7,8]. HF may impair health-related QoL as a result of physical symptoms, psychological problems, adverse effects of treatment and social limitations [9].
Although there is no internationally accepted definition for QoL as it pertains to health, it is usually regarded as existing relative to individual and/or cultural expectations and goals [10,11]. The World Health Organisation has defined health as “a state of complete physicalmental and social well being and not merely the absence of disease” [12].
The use of formal measurements for QoL to evaluate treatment effectiveness began around 1994 when the Agency for Health Care Policy and Research published recommendations to practitioners to begin routinely assessing patients’ QoL and use the result to determine future management [13]. Several studies have shown that QoL indices provide additional predictive value with respect to both mortality and HF related hospitalization above and beyond the predictive power of variables like ejection fraction, age, treatment and New York Heart Association Classification (NYHA) [14,15].
Several instruments have been used to evaluate QoL in HF. Some are disease specific like the Kansas City Cardiomyopathy Questionnaire (KCCQ) [16], Minnesota Living with Heart Failure (MLHF) questionnaire [17], Patient Global Evaluation (PGA) [18,19], Physicians Global Evaluation (PhysGA) [18,19] while others are generic like the WHOQOL-BREF [20], SF-36 [21]. Studies continue to evaluate the combination that maximises sensitivity to the aspects of the condition understudy [22].
Not much work has been done in this area in Sub-Saharan Africa and most of the available disease specific instruments were developed using the Caucasian population. We therefore evaluated the QoL of our stable heart failure patients using two instruments, one generic (WHOQOL-BREF) and one specific (Kansas City Cardiomyopthy Questionnaire—KCCQ) health related quality of life instruments. The objectives were to investigate the frequency of poor QoL in our HF patients and the reliability of using a generic instrument when the disease specific instruments are not available.
2. METHOD
Consecutively consenting adult HF patients aged ≥18 yrs who were attending the cardiology clinic of the Lagos University Teaching Hospital were recruited. Patients were eligible for enrolment if they had not been hospitalised in the last three months prior to enrolment, could read and understand the items on the questionnaire and gave written informed consent.
Patients were excluded if they refused to participate, had been recently hospitalised (at least three months before the recruitment visit) and not literate enough to understand the items on the questionnaire.
The study was approved by the hospital’s health research ethics committee.
Patients’ demographic data and clinical data retrieved from their clinical notes were entered into a standard proforma. The patients then filled out the KCCQ and WHOQOL-BREF at the same sitting.
2.1. KCCQ [16]
The KCCQ is a 23-item, self administered disease specific questionnaire for assessing HRQOL in patients with congestive heart failure. It quantifies in a disease specific fashion patients’ QoL. It comprises seven domains (physical limitation, symptom stability, symptom burden, symptom frequency, self efficacy, QoL and Social limitation). Responses are arrayed on an adjectival (Likert) scale with clinically meaningful gradations between categories.
It is scored by assigning each response an ordinal value, beginning with 1 for the response that implies the lowest level of functioning and summing items within each domain. Missing values within each domain are assigned the average of the answered items within that same domain. Scale scores are transformed to a 0 to 100 range by subtracting the lowest possible scale score, dividing by the range of the scale and multiplying by 100. Two summary scores functional and clinical summary scores are calculated from the domain scores. The functional status score is calculated by combining the physical limitation and symptom domains (excluding symptom stability) while the clinical summary score is calculated by combing the functional status scores with the QoL and social limitation domains.
2.2. WHOQOL-BREF [20]
This is a 26-item self administered (could be interviewer assisted) generic HRQoL questionnaire. It provides a short form quality of life assessment that looks at domain level profiles using data from the pilot WHOQOL assessment and all available data from the field trial of the WHOQOL-100. Four domain scores are derived from the responses. Two items are examined separately: question 1 which asks about an individuals’ overall perception of the quality of life and question 2 which asks about an individual’s overall perception of their health. The four domain scores denote an individuals’ perception of the quality of life in each particular domain. The four domains assessed by this instrument are physical health, psychological, social relationships and environment.
Domain scores are scaled in a positive direction i.e. higher scores denote higher quality of life the mean score of items within each domain is used to calculate the domain score. Mean scores are then multiplied by 4 in order to make domain scores comparable with scores used in the WHOQOL-100. This converts the scores to range between 4 - 20. A second transformation converts domain scores to a 0 - 100 scale.
When more than 20% of data from an assessment is missing, the assessment is discarded. Where an item is missing, the mean of the other items in the domain is substituted. Where more than two items were missing from the domain score, the domain was not calculated except for domain 3 which is not calculated when ≤1 item is missing.
Data was analysed using SPSS version 16. Continuous variables are presented as mean ± SD while categorical variables are presented as percentages. Comparison between means was tested with the student t-test and chi square statistics was used to compare proportions. Pearson’s correlation coefficient was used to test for relationship between the quality of life and some evaluated clinical parameters and also between the two instruments used in the study. Statistical significance was set at p ≤ 0.05.
3. RESULT
Complete data set of 190 patients out of 216 was analysed. There were 91 (47.9) males and 99 (52.1) females with a mean age of 51.90 ± 13.21 years. Only 52 (26.4%) had college education and 143 (75.2%) had very poor personal resources (pensioners, artisans, traders and unemployed). Most, 155 (81.6%) were married. The mean NHYA class was 2.56 ± 0.73 and about 105 (55.6%) were paying their medical bills themselves. The mean duration of heart failure was 35.82 ± 44.56 months and number of hospitalisations was 1.22 ± 1.99 and 87 (45.8%) had been hospitalised at least once. More than half of the patients, 106 (55.8%) were in NYHA class II. The mean ejection fraction was 42.28 ± 17.84 and 139 (73.16%) had heart failure with reduced ejection fraction. Details of the demographic and clinical profile of the study population are shown in Table 1. The patients with incomplete data were similar in age, sex distribution and NYHA class but had a significantly higher duration of their heart disease, p = 0.001.
The mean QoL score using the KCCQ instrument was 59.61 ± 23.80 and 52 (27.37%) had scores below 50. The domain and summary scores for the KCCQ instruments are shown in Table 2. They are highest for symptom burden 85.52 ± 19.28 and lowest for self efficacy 44.37 ± 23.01. The QoL scores for the WHO-BREF was 3.72 ± 0.90 and 22 (11.6%) had scores below the midway value of 3. The general health assessment score was 3.28 ± 1.11 and 80 (31.5%) had scores below the midway score of 3. The domain scores score for the WHO BREF are shown in Table 2. The highest score was for psychological health 66.72 ± 39.38 and lowest for physical health 59.28 ± 18.22.
Table 3 shows the gender comparison of selected clinical parameters and domain scores of the two instruments used for the study. The females had a significantly longer duration of heart failure than the males, 43.48 ± 55.41 vs 27.47 ± 26.14 months, p = 0.01. There was no difference in the QoL scores between the males and females using both the KCCQ and WHO-BREF instrumentsTable 1. Demographic and clinical characteristics of the study population.
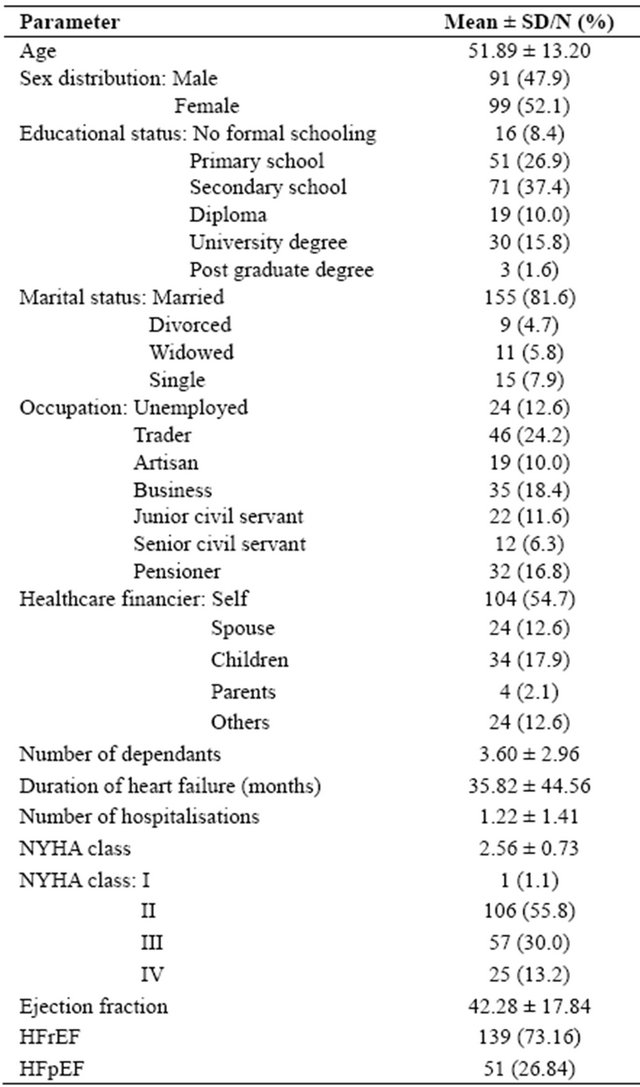
Table 2. KCCQ and WHO-BREF quality of life scores of the study population.
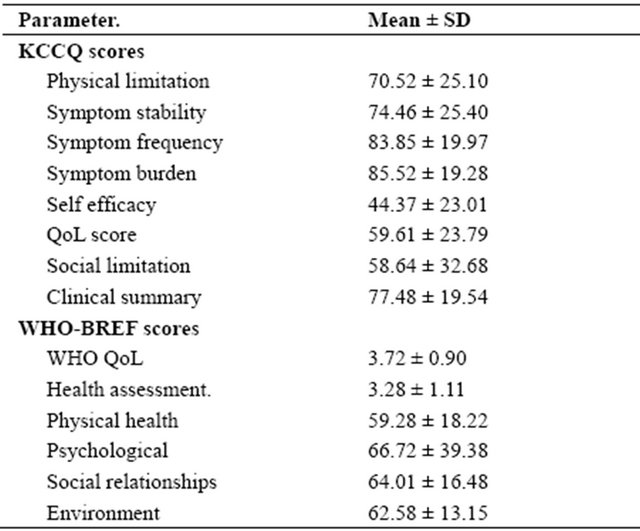
Table 3. Gender comparison of selected clinical parameters and domain scores of both the KCCQ and WHO-BREF instruments.

p = 0.57 and 0.46 respectively. The females felt more socially limited on the KCCQ, 54.04 ± 33.69 vs 63.65 ± 30.94, p = 0.04. However the males had a significantly lower score than the females on the social relationship domain on the WHO-BREF, 61.26 ± 16.45 and 66.86 ± 16.11, p = 0.03. They also felt more affected by their environmental issues than the females, 60.62 ± 12.68 and 64.36 ± 13.38, p = 0.05.
Table 4 shows the categorisation of the scores using quartiles of final scores obtained from the instruments. Physical limitation and social limitation were severe and moderate in about 34 (18%) and 67 (35.30%) of the subjects respectively using the KCCQ instrument. With the WHO-BREF disturbances in physical health and social relationships was severe to moderate in 43 (22.61%) and 32 (16.85%) respectively. With the KCCQ, 13 (6.84%) felt their QoL was poor and 39 (20.52%) felt it was fair while 22 (11.6%) and 39 (20.5%) felt their QoL was poor and fair respectively with the WHOQOL-BREF. The general health assessment was poor and fair in 60 (31.58%) and 26 (13.68%) respectively.
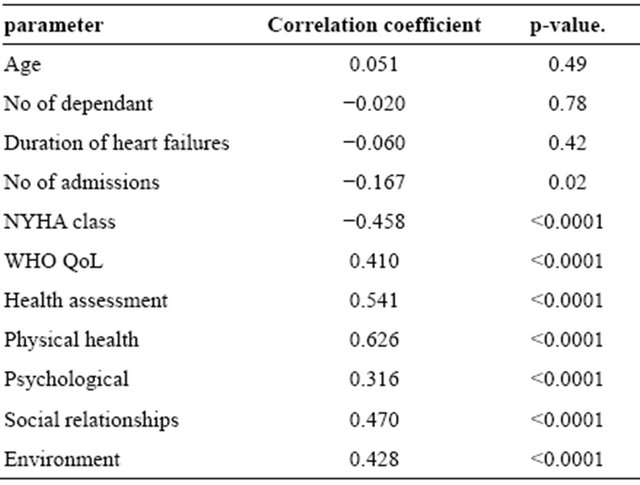
Correlation between QoL scores and some selected parameters is as shown in Table 5. There was significant positive correlation between the QoL scores on the KCCQ and WHO-BREF instruments, p < 0.0001, and the health assessment scores, p < 0.0001. Significant positive correlation was also observed between the QoL score on the KCCQ instrument and the four domains of the WHOQOL-BREF; physical health, psychological, social relationships and environment, p < 0.0001. A negative correlation was observed between the KCCQ QoL scores and the number of previous hospitalisations, p = 0.02 and NYHA class, p < 0.0001.
4. DISCUSSION
The health related quality of life in this study as perceived by the patients was suboptimal in about a 27% of the patients surveyed when the KCCQ instrument was used and 22% using the WHOQOL-BREF. The WHOQOL-BREF though not a disease specific QoL instrument was able to demonstrate to a comparable degree the poor quality of health in these patients with heart failure. Poor quality of life in patients with heart failure has been demonstrated by many investigators and in the large drug trials [23-25]. It has been suggested that this should become an important end point in treatment strategies [26]. This has become imperative as some of the newer treatment measures that improve survival may not necessarily improve the QoL of the patients [24]. It has been demonTable 4. Categorisation of the QoL and some domain scores.
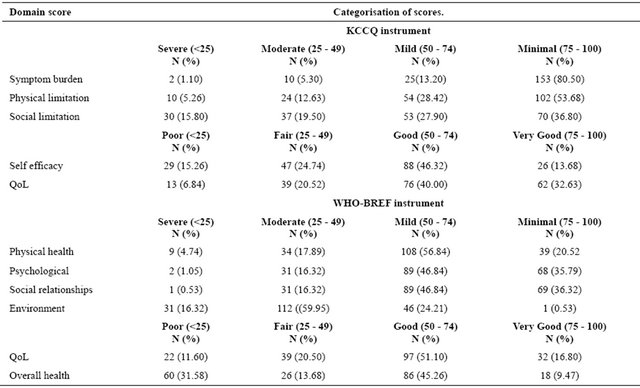
Table 5. Pearson’s correlation between KCCQ QoL score, selected clinical parameters and WHO BREF domain scores.
strated in some surveys that some patients may be willing to trade survival for an improvement in their QoL [27,28].
The patients also showed low to average scores in some of the domains evaluated. The KCCQ yielded low to average scores in the self efficacy and social limitation domains. More than a third of the patients felt they had moderate to severe limitations in these domains when the scores were categorised using 25 percentiles. However the mean scores in the domains of physical limitation, symptom frequency, symptom burden and the clinical summary were quite good. The domain scores may appear discordant but it is important to note that the majority of the patients evaluated were in NYHA II and may not have had a heavy symptom burden. However this study demonstrated a negative correlation between the NYHA class and the QoL scores with the KCCQ. The WHO-BREF on the other hand showed more limitation in the environment and physical health domains than the psychological and social relationships and there was no correlation with the NYHA class. This finding is in agreement with most studies that have suggested that the physical limitation in HF is a major contributor to the poor QoL experienced by these patients [29]. The differences between the two instruments most likely would have originated from the peculiarities of the two instruments. While the KCCQ is disease specific and focuses on the effect of heart failure on the quality of life, the WHO-BREF is a generic instrument taking a more global look at the persons HRQoL.
It is important to note however that there is more to HRQoL in heart failure than just the physical limitation of the disease. It has also been established that when compared with other diseases like COPD, the heart failure patient has a poorer quality of life for the same level of exercise limitation [23]. It is how these diseases interact with other aspects of an individual’s social, psychological and environmental issues that determine their QoL. Quality of life has been defined as “an individual’s perception of their position in life in the context of the culture and value system in which they live and in relation to goals, expectations, standards and concerns. It is a broad ranging concept affected in a complex way by the person’s physical health, psychological state, personal beliefs, social relationships and their relationships to salient features of their environment” [11,12].
The patients in the present study had very good scores in the symptom frequency, stability and burden domains of the KCCQ and above average for the similar domains in the WHO-BREF. The discordance may be from the fact that our patient population is quite young (51.89 ± 13.20 yrs) when compared with usual mean ages of patients seen in most heart failure studies, which is usually above 60 years [25,30,31]. So the social aspect of the disease may play a more important role in this middle aged population. It is important to note that most of our patients were paying their medical bills themselves without any insurance cover or support and most were in the low income cadre. Most of these patients being young will still have a number of dependants that they are financially responsible for. Inability to meet these social obligations will further worsen their perception of life despite not being very symptomatic. The social burden on these patients is reflected on the low scores in these domains on the KCCQ (social limitation, self efficacy). However most studies from the developed world have shown that age has minimal influence on QoL scores [25].
There was no gender differences noted in the patients’ assessment of their quality of life with the two instruments used. This is similar to the findings of the Norwegian follow up study of HF patients [31]. On the other hand previous studies have suggested that females with HF tend to have a poorer QoL [28]. However the females in this study felt more socially limited than the men on the KCCQ but this trend was reversed in the WHOBREF. This agrees with the findings in the CARE-HF study where the females reported a greater problem in all five domains of the EQ-5SD QoL instrument [25]. The worse profile of the men on the WHO-BREF agrees with the findings of Hobbs et al, who reported poorer QoL in men with significant differences in role limitations due to emotional problems, lack of energy and pain [23]. The reason for this discordant trend is most likely instrument based. The study by Hobbs used a generic HRQoL instrument, SF-36. The males also felt more affected by the environmental factors using the WHO-BREF.
A positive correlation was seen between the QoL scores of the instruments. This is quite interesting despite some differences noted in the trend of domain scores and the gender issues as it relates to these domains between the two instruments. The positive correlation persisted between the KCCQ sores and the different domains of the WHO-BREF. This will suggest that despite its generic nature and obvious limitations, that this instrument can be used in the absence of a disease specific instrument to assess the HRQoL of heart failure patients at least in our environment. This is an important practice and health economic issue as most of the disease specific instruments are copy righted and may not be affordable for the cardiologist in a resource challenged environment. A negative correlation was also seen between the QoL scores on the KCCQ and the number of hospitalisation. This is not unexpected as frequent hospitalisation will mean frequent disruption of the individual’s level of function in all domains, physical, emotional, social and psychological.
5. LIMITATIONS
The major limitation with this study is the use of disease specific instrument developed for a Caucasian population. This is because the aspects of living that make up quality life may differ between cultures, groups and social strata. We believe that an indigenous instrument with more locally relevant items may actually show a much lower QoL than has been demonstrated in this study. A direct comparison of the scores could not also be done because the item questions for each instrument are worded differently.
6. ACKNOWLEDGEMENTS
The authors gratefully acknowledge Dr. John A. Spertus and his team for the provision of the KCCQ instrument used for this study at no cost to the investigators. We also would like to acknowledge the excellent job done by Miss Anne Okpi and Modinat Kilasho in entering the data.
![]()
![]()
REFERENCES
- Lloyd-Jones, D., Adams, R., Carnethon, M., et al. (2009) Heart disease and stroke statistics—2009 update: A report of the American Heart Association Statistics Committee and stroke statistics subcommittee. Circulation, 119, e21- e181. doi:10.1161/CIRCULATIONAHA.108.191261
- Mosterd, A. and Hoes, A.W. (2007) Clinical epidemiology of heart failure. Heart, 93, 1137-1146. doi:10.1136/hrt.2003.025270
- Task force for the diagnosis and treatment of acute and chronic heart failure (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal, 33, 1787-1847. doi:10.1093/eurheartj/ehs104
- Feinstein, A.R., Fisher, M.B. and Pigeon, J.G. (1989) Changes in dyspnoea-fatigue ratings as indicators of quality of life in the treatment of congestive heart failure. American Journal of Cardiology, 64, 50-55. doi:10.1016/0002-9149(89)90652-8
- Guyatt, G.H., Thompson, P.J., Berman, L.B., Sullivan, M.J., Townsend, M., Jones, N.L. and Pugsley, S.O. (1985) How should we measure function in patients with chronic heart and lung disease. Journal of Chronic Diseases, 18, 517-524. doi:10.1016/0021-9681(85)90035-9
- Ekman, I., Cleland, J.G., Andersson, B. and Swerdberg, K. (2005) Exploring symptoms in chronic heart failure. European Journal of Heart Failure, 7, 699-703. doi:10.1016/j.ejheart.2005.07.003
- Packer, M., Narahara, K.A., Elkayam, U., Sullivan, J.M. and Hampton, J.R. (1993) Double-blind, placebo controlled study of flosequinan in patients with chronic heart failure. Principal investigators of the REFLECT study. Journal of the American College of Cardiology, 22, 65- 72. doi:10.1016/0735-1097(93)90816-J
- Cowley, A.J., Stainer, K., Wynne, R.D., Rowley, J.M. and Hampton, J.R. (1989)Comparison of the effects of captopril and enoximone in patients with severe heart failure: A placebo-controlled double-blind study. International Journal of Cardiology, 24, 311-316. doi:10.1016/0167-5273(89)90010-7
- Tate, C.W., III, Robertson, A.D., Zolty, R., Shakar, S.F., Lidenfield, J., Wolfel, E., Bristow, M.R. and Lowes, B.D. (2007) Quality of life and prognosis in heart failure: Result of the Beta-Blocker Evaluation survival trial (BEST). Journal of Cardiac Failure, 13, 732-737. doi:10.1016/j.cardfail.2007.07.001
- Bowling, A. (1995) What things are important in people’s lives? A survey of public’s judgement to inform scales of health related quality of life. Social Science & Medicine, 41, 1447-1462. doi:10.1016/0277-9536(95)00113-L
- Cella, D.F. and Tulsky, D.S. (1990) Measuring quality of life today: Methodological aspects. Oncology, 4, 29-38.
- World Health Organization (19-22 June 1946) Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference. New York.
- Heart Failure Guideline Panel (1994) Heart failure: Evaluation and care of patients with left ventricular dysfunction. AHCPR Publication, Silver Spring.
- Konstan, V., Salem, D., Pouluer, H., Kostis, J., Gorkin, L., Shumaker, S., et al. (1996) Baseline quality of life as a predictor of mortality and hospitalisation in 5025 pateints with congestive heart failure. American Journal of Cardiology, 78, 890-895. doi:10.1016/S0002-9149(96)00463-8
- Soto, G.E., Jones, P., Weintraub, W.S., Krumholz, H.M. and Spertus, J.A. (2004) Prognostic value of health status in patients with heart failure after acute myocardial infarction. Circulation, 110, 546-551. doi:10.1161/01.CIR.0000136991.85540.A9
- Green, P.C., Porter, C.B., Bresnahan, D.R. and Spertus, J.A. (200) Development and evaluation of the Kansas City cardiomyopathy questionnaire: A new health status measure for heart failure. Journal of the American College of Cardiology, 35, 1245-1255. doi:10.1016/S0735-1097(00)00531-3
- Rector, T.S., Kubo, S.H. and Cohn, J.N. (1987) Patient’s self-assessment of their congestive heart failure: Content, reliability and validity of a new measure: The Minnesota living with heart failure questionnaire. Heart Failure, 3, 198-219.
- Colluci, W.S., Packer, M., Bristow, M.R., Gilbert, E.M., Cohn, J.N., Fowler, M.B., et al. (1996) Carvedilol inhibits clinical progression in patients with mild symptoms of heart failure. Circulation, 94, 2800-2806. doi:10.1161/01.CIR.94.11.2800
- Bristow, M.R., Gilbert, E.M., Abraham, W.T., Adams, K.F., Fowler, M.B., Hershberger, R.E., et al. (1996) Congestive heart failure/myocardial disease: Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. Circulation, 94, 2807-2816. doi:10.1161/01.CIR.94.11.2807
- The World Health Orgainisation Quality of Life (WHOQOL). http//www.who.int/evidence/assessmentinstrument/qol/q11. htm
- McHorney, C., Ware, J. and Raczek, A. (1993) The MOS-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31, 247-263. doi:10.1097/00005650-199303000-00006
- Berry, C. and McMurray, J. (1996) A review of qualityof-life evaluations in patients with congestive heart failure. American Journal of Cardiology, 78, 890-895. doi:10.1016/S0002-9149(96)00463-8
- Hobbs, F.D.R., Kengre, J.E., Roalife, A.K., Davis, R.C., Hare, R. and Davies, M.K. (2002) Impact of heart failure and left ventricular systolic dysfunction on quality of life. A cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population. European Heart Journal, 23, 1867-1876. doi:10.1053/euhj.2002.3255
- Hjalmarson, A., Goldstein, S., Fagerberg, B., Wedel, H., Waagstein, F., Kjekshus, J., et al. (2000) Effects of controlled-release metoprolol on total mortality, hospitalisations and well being in patients with heart failure: The Metoprolol CR/XL Randomised Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group, JAMA, 283, 1295-1302. doi:10.1001/jama.283.10.1295
- Calvert, M.J., Freemantle, N. and Cleland, J.G.F. (2005) The impact of chronic heart failure on health-related quality of life data acquired in the baseline phase of the CARE-HF study. European Journal of Heart Failure, 7, 243-251.
- Mc Donagh, T.A., Blue, L., Clark, A.L., Dahlstrom, U., Ekman, L., Lainsack, M., McDonald, K., Ryder, M., Stromberg, A. and Jaarsma, T. (2011) European Society of Cardiology Heart Failure Association Standards for delivering heart failure care. European Journal of Heart Failure, 13, 235-241. doi:10.1093/eurjhf/hfq221
- Lewis, E.F., Johnson, P.A., Johnson, W., Collins, C., Griffin, L. and Stevenson, L.W. (2001) Preferences for quality of life or survival expressed by patients with heart failure. The Journal of Heart and Lung Transplantation, 20, 1016-1024. doi:10.1016/S1053-2498(01)00298-4
- Rector, T.S., Tscumperin, L.K., Kobo, S.H., Bank, A.J., Francis, G.S., McDonald, K.M., et al. (1995) Using the living with heart failure questionnaire to ascertain patients’ perspective on improvement of in quality of life versus risk of drug induced death. Journal of Cardiac Failure, 1, 201-206. doi:10.1016/1071-9164(95)90025-X
- Witte, K.K. and Clark, A.L. (2007) Why does chronic heart failure cause breathlessness and fatigue? Progress in Cardiovascular Diseases, 49, 366-384. doi:10.1016/j.pcad.2006.10.003
- Comin-Colt, J., Lainscak, M., Dickstein, K., Fillipatos, G.S., Johnson, P., Luscher, T.F., Mori, C., Willenheimer, R., Ponikowski, P. and Anker, S. (2013) The effect of intravenous ferric carboxymaltose on health-related quality of life in patients with chronic heart failure and iron deficiency: A subanalysis of the FAIR-HF study. European Heart Journal, 34, 30-38. doi:10.1093/eurheartj/ehr504
- Hole, T., Grundtvig, M., Flonaes, B. and Westheim, A. (2010) Improved quality of life in Norwegian heart failure patients after follow-up in outpatient heart failure clinics: Results from the Norwegian heart failure registry. European Heart Journal, 12, 1247-1252. doi:10.1093/eurjhf/hfq156

