Open Journal of Stomatology
Vol.2 No.3(2012), Article ID:22988,6 pages DOI:10.4236/ojst.2012.23036
Prevalence of oral lesions and the effects of HAART in adult HIV patients attending a tertiary hospital in Lagos, Nigeria
![]()
1Department of Preventive Dentistry, College of Medicine, University of Lagos, Lagos, Nigeria
2Department of Oral Pathology/Oral Biology, College of Medicine, University of Lagos, Lagos, Nigeria
Email: *Htolaeweka@yahoo.com
Received 13 April 2012; revised 14 May 2012; accepted 3 June 2012
Keywords: HIV; Oral Lesions; Prevalence; HAART
ABSTRACT
Background: Oral lesions have been reported to be early clinical features of HIV infection. The objective of this study was to establish the prevalence of oral lesions and the management outcome using HAART in HIV Seropositive patients attending a tertiary hospital in Lagos, Nigeria. Methods: This was a prospective study in 114 newly diagnosed adult HIV infected patients (not on antiretroviral therapy), who attended the PEPFAR clinic at Lagos University Teaching Hospital. They were assessed for oral lesions which were evaluated using EEC/WHO—Classification on the diagnostic criteria for oral lesions in HIV. Data were collected using an interviewer administered questionnaire. Oral examination was carried out and oral lesions detected were recorded. Presence or absence of oral lesions was evaluated following 3 months use of HAART. Results: 114 patients were enrolled into the study, 49 (43.0%) males and 65 (57.0%) females, with age range of 18 - 63 years. 42 (36.8%) presented with oral lesions, 19 (45.2%) of which had multiple lesions. Oral Candidiasis which accounted for 47.7% was the most common oral lesion observed followed by Oral Hairy Leukoplakia (21.6%) and oral hyperpigmentation (10.8%). Pseudomembraneous Candidiasis was the most common variant of oral Candidiasis seen. Prevalence of oral lesions was significantly associated with low CD4 count and high viral load. Eighty four percent (84%) of oral lesions disappeared following 3 months of HAART treatment. Conclusion: Oral lesions are common features of HIV and a marker for progression of the disease to AIDS. There was significant reduction in oral lesions following 3 months treatment with HAART.
1. INTRODUCTION
Acquired Immune-Deficiency Syndrome (AIDS) is a complex of symptoms and infections caused by the Human Immunodeficiency Virus (HIV) as it impacts the immune system [1]. South Africa has the largest population of HIV patients in the world, followed by Nigeria and India [2].
Oral lesions have been reported to be early clinical features of HIV infection and are associated with disease progression [3]. These lesions are often indicators of immune suppression and can be used for early testing, diagnosis and management of patients with HIV/AIDS. Oral lesions contribute to patients’ morbidity, affecting the psychological and economic functioning of the individual and community [4]. These lesions can cause pain, discomfort and other symptoms and in the most cases warrant treatment [5,6].
It has been shown in various studies that the prevalence of HIV-related oral lesions reduces significantly with HAART. These studies examining the effect of HAART on the prevalence of individual oral manifestations mainly reported on oral candidiasis, oral hairy leukoplakia, HIV-related periodontal diseases, Kaposi’s sarcoma (KS), oral papilloma, and HIV-related salivary gland disease showed reduction in the prevalence [7-9].
Several studies carried out in the various geopolitical regions of Nigeria have shown the high prevalence of oral lesions amongst infected patients. Yet in Lagos (a densely populated, cosmopolitan city with different ethnic groups and social classes of people), few studies have been carried out to determine the prevalence of oral lesions in HIV infected patients, their relationship with the clinical stages of the disease and the effect of HAART on the oral lesions, hence the need for this study.
2. METHODOLOGY
This was a prospective study in which 114 newly diagnosed adult HIV infected patients (not on antiretroviral therapy) who attended the Presidents Emergency Programme for AIDS Relief (PEPFAR) clinic at the Lagos University Teaching Hospital (LUTH), Lagos State, Nigeria were assessed for oral lesions. The oral lesions were evaluated using EEC-WHO (EC-Clearinghouse, 1993) [10]—Classification on the diagnostic criteria for oral lesions in HIV. Furthermore, clinical staging, CD4 count and viral load values were determined in all the patients and increase/reduction of oral lesions were evaluated following 3 months use of HAART.
Data was collected using an interviewer administered questionnaire. Relevant information such as demography, oral complaints, medical and drug history were documented. Oral examination was carried out and oral lesions detected and clinically characterized as direct manifestations of HIV were diagnosed based on their clinical presentation and recorded. The patients were clinically staged based on WHO guidelines (2005) [11], and clinical photographs were taken.
The values of the CD4 count and viral load of each patient at presentation and 3 months recall visit were recorded.
Some of the oral lesions seen were treated, while others did not require treatment. Patients were recalled 3 months later to review their response to HAART treatment.
Data was analyzed using Epi info 2000 series for windows (Microsoft Corp). Chi-square statistical analysis of the strength of association between types of oral manifestations and the CD4 counts were carried out. Pvalues < 0.05 were accepted as being statistically significant. Frequency tables were generated for nominal and ordinal variables.
3. RESULTS
A total of 114 patients were seen. Age range was 18 - 63 years (mean 35.4 ± 9.8 years). 49 (43.0%) were males and 65(57.0%) were females with male to female ratio 1:1.3 (Table 1).
Forty two (36.8%) of the patients presented with oral lesions, 72 (63.2%) patients did not present with oral lesions characterized as manifestation of HIV/AIDS. Table 2 shows the distribution of the different types of lesions and their prevalence in the study group.
The most common oral lesion observed was Oral Candidiasis (OC) seen in 31 (47.7%) of all lesions seen, followed by Oral hairy leukoplakia (OHL) which was 14 (21.6%), and hyperpigmentation seen in 7 (10.8%). Other lesions seen were presented in Table 2. Some of the patients had multiple lesions bringing the total number of lesions seen to 65. 23 (54.8%) of them had single lesions, 10 had two lesions (23.7%), 7 had three lesions (16.7%) and 2 had four lesions (4.8%) Table 3. Pseudomembraneous Candidiasis (PC) was the commonest variant of Candidiasis seen accounting for 29 (59%) cases. Erythematous Candidiasis (EC) was seen in 10 (25.6%) cases and Angular Cheilitis (AC) in 6 (15.4%).
Observation in this study shows a significant association between gender and occurrence of oral lesions, 26 (61.9%) from the 42 patients presenting with oral lesions in males, while 16 (38.1%) presented in females, (P < 0.05). Age group 31 - 40 accounted for the highest number of oral lesions seen in the study. This is summarized in Tables 4(a) and (b).
The highest number of oral lesions recorded was observed in patients with CD4 count lower than 200 cells/ mm3. Also the number of oral lesions in patients with viral load greater than 55,000 copies/ml is significantly higher than the number of oral lesions in the group < 55,000 copies/ml (Tables 4(c) and (d)). Most of the patients with oral lesions were observed in clinical stage III of the disease (more than 30 lesions). Table 4(e).
A total of 84.2% of the oral lesions cleared with use of HAART. Table 5(a) demonstrates the effect of HAART on individual lesions seen in the 10 patients on HAART who presented initially with oral lesions. All cases of Candidiasis responded to HAART, they all cleared (100%), most of the other lesions seen also cleared (OHL: 100%, hyperpigmentation: 66.7%), while others present were reducing (15.8%) showing good response to treatment. On the contrary, 80% of patients that were not on HAART had persistent oral lesions after 3 months assessment (Table 5(b)).
4. DISCUSSION
The oral cavity is an important and frequently undervalued source of diagnostic and prognostic information in patients with HIV infection [12]. Oral disease is frequently the first indicator of progression of symptomatic disease of HIV infection [13].
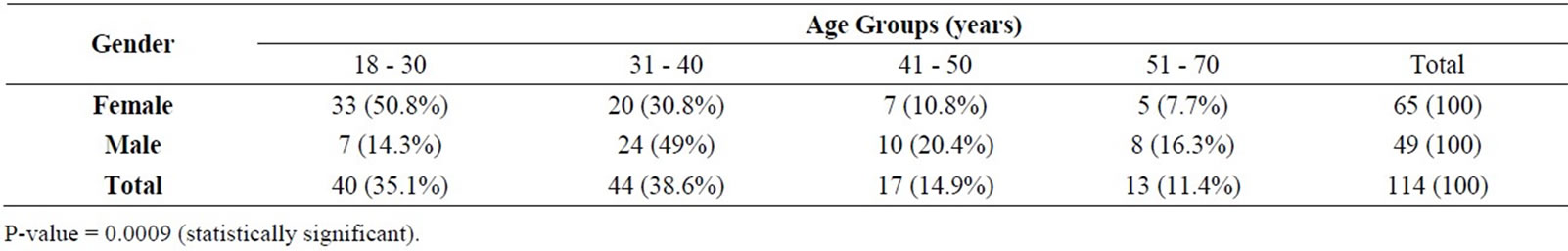
Table 1. Age and gender distribution of 114 respondents.
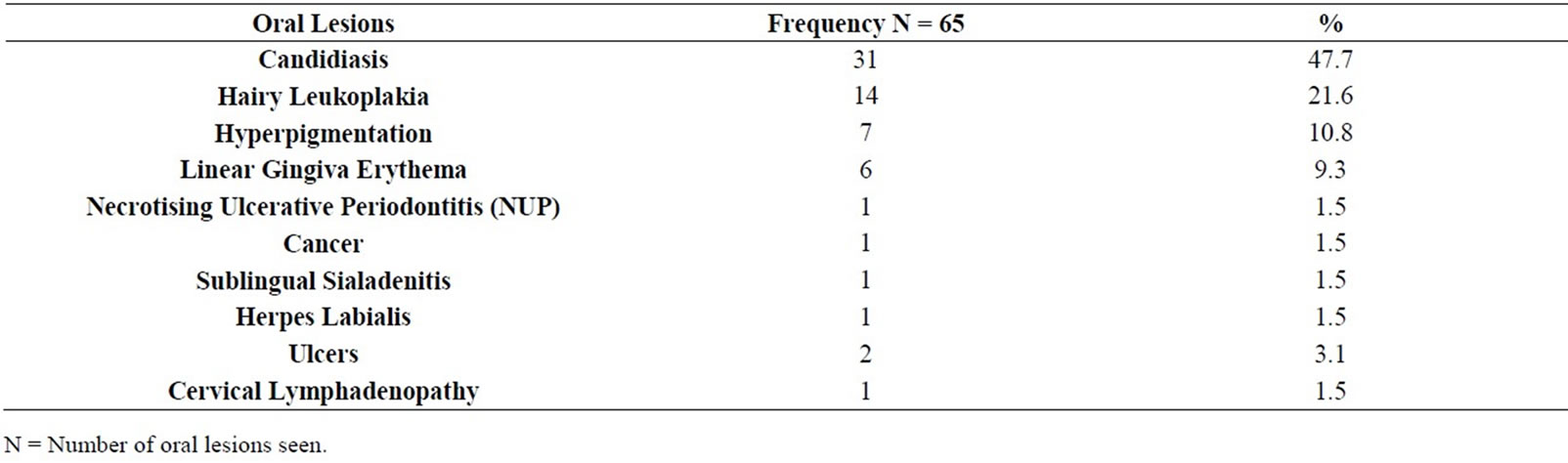
Table 2. Distribution of different types of lesions seen in patients who presented with oral lesions.
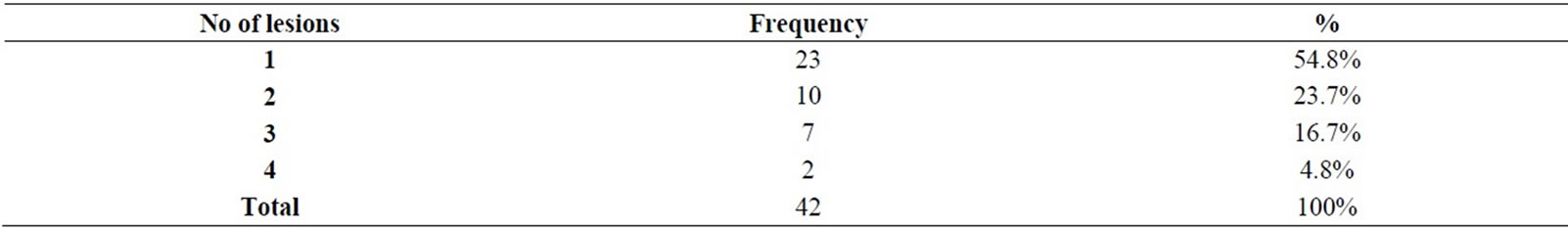
Table 3. Distribution of multiple lesions in 42 HIV/AIDS patients with oral lesions.
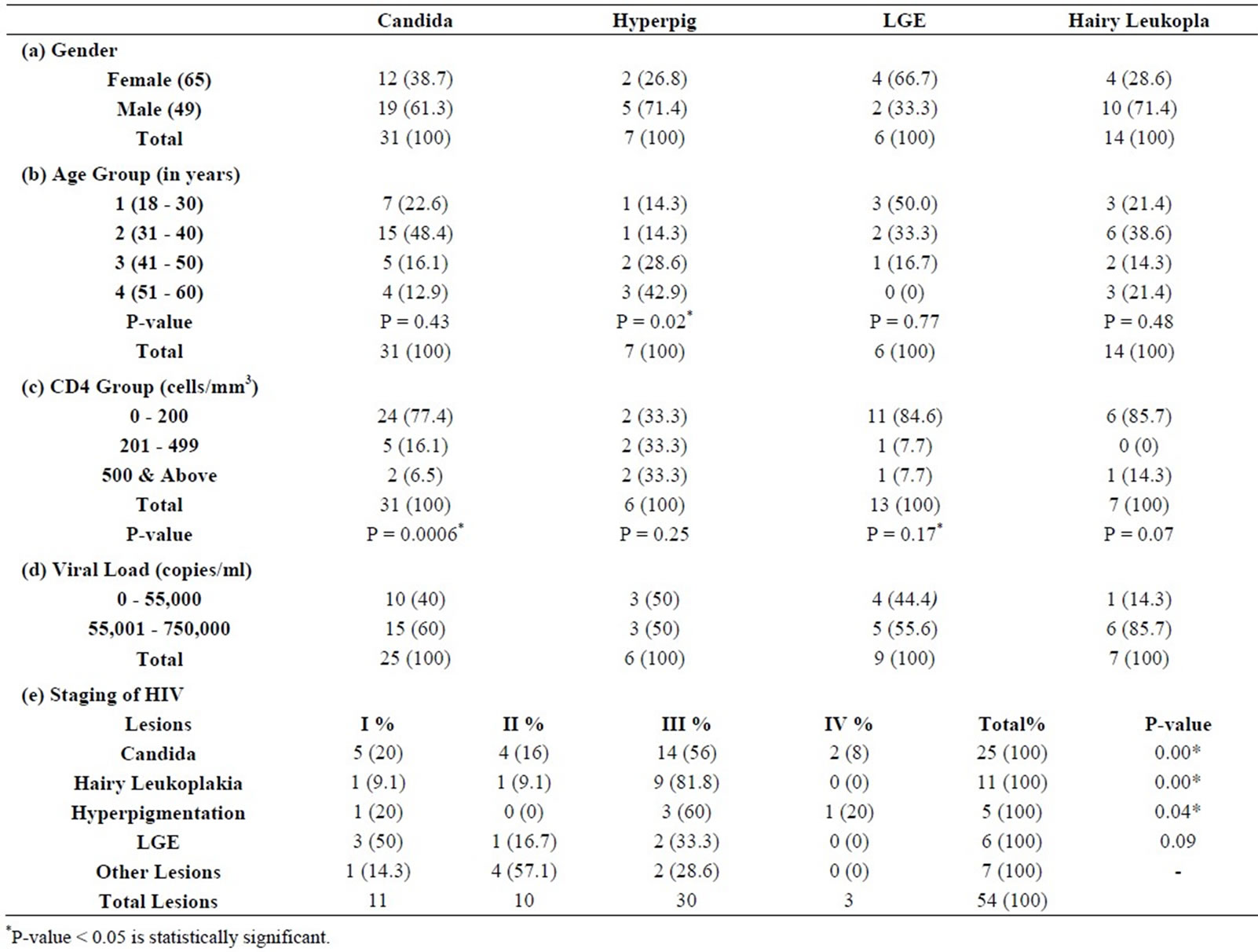
Table 4. Association between specific oral Lesions with gender, age groups, CD4 count, viral load and clinical staging.
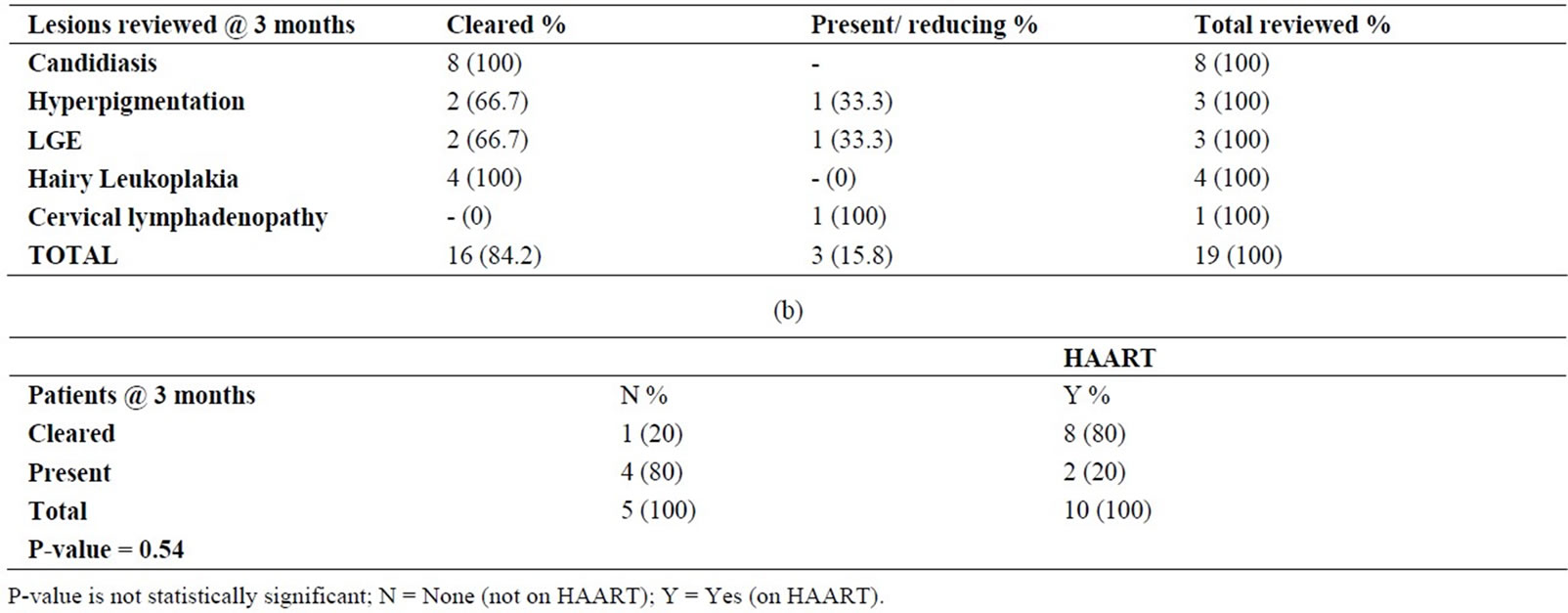
Table 5. (a) Effect of HAART on individual oral lesions at 3 months review; (b) Effect of HAART on patients with oral lesions reviewed at 3 months.
At least one oral lesion was present in each of the 42 (36.8%) patients in the series of 114 HIV infected patients. The prevalence of 36.8% of oral lesions in this study is consistent with findings in the study by Matee et al. (2000) [14] who also found a prevalence of 36.8% among 227 HIV infected patients in Tanzania. The totals of 65 oral lesions were observed in the 42 patients because 19 (45.1%) patients presented with multiple lesions, with a maximum number of 4 lesions seen in 2 patients (4.8%). In line with the reasoning of Glick et al. (1994) [15] that the presence of specific oral manifestations and the number of different concurrent intra-oral lesions among HIV infected persons are associated with severe immune suppression and AIDS, it is suggested that multiple oral lesions observed in the series is a feature of severe immunosuppression in HIV infected patients.
A relatively higher prevalence of oral lesions has been reported in Nigerian studies, 63.8% in Kano (Arotriba et al. 2005) [16], 43.9% and 41.8% in Jos (Taiwo et al., 2005 and 2006 respectively) [6,17]. 45% in Ibadan (Arotiba et al., 2006) [18], 84% in Ile-Ife (Adedigba et al., 2007) [19], 48% in Benin (Onunu et al., 2002) [20] and 70% in Lagos (Wright et al., 2005) [21].
The relatively low rate of oral lesions in this series compared to previously reported Nigerian studies may be due to the fact that the present study reports oral lesions from a population with less than 50% proportion of full blown AIDS cases, whereas, previous studies reported oral lesions in a population with relatively higher proportion of AIDS cases.
Report in this series of oral lesions presenting mostly in patients aged between 31 and 40 years is consistent with report of study in Lagos by Wright et al. (2005) [21]. However, Taiwo et al. (2005) [6] reported peak occurrence in a lower age group of 21 - 30 years. Children and adolescents have been reported to share similar oral manifestation with adults, although oral Kaposi sarcoma occurred less frequently while parotid enlargement, xerostomia and herpes infections occurred more frequently in children [22,23].
Significantly higher occurrence of oral lesions in HIV infected males than females in this study, contrast with general trend of HIV occurring more in females than males, also observed in this study. Although reason for this is not known, it could be postulated that the general habit of late presentation of males for treatment and early presentation of females may be attributed to the trend observed in this study.
Our finding that Candidiasis was the most common oral lesion observed in HIV/AIDS in this series is consistent with findings reported in Nigerian studies 17, 20, 24, 25, although the frequencies reported varied.
Pseudomembraneous Candidiasis was the most common variant of Candidiasis observed in this series, whereas an earlier study from the same centre by Agbelusi et al. (2005) [25] reported Erythematous Candidiasis as being the most common variant of oral Candidiasis in HIV/ AIDS patients. Some reports in scientific literature agree with the observation of Pseudomembranous Candidiasis being the most frequent variant of oral Candidiasis in HIV/AIDS patients [17,26-28].
Oral Hairy Leukoplakia (OHL) observed to be the second most prevalent oral lesion in this series is consistent with findings in a Tanzanian study by Matee et al. [14] and an Italian study by Campisi et al. [28], while the present series reports 21.6% prevalence of OHL, a Thai study [29] reports 26%, and Nigerian studies reported 5% [30] and 1.3% [19]. The higher frequency of occurrence of OHL reported in this study compared with low frequencies reported in earlier Nigerian studies could be due to improved knowledge of diagnosis of OHL. Observation that Oral Hairy Leukoplakia which was seen more in males (71.4%) is consistent with observations by Kerdpon et al. [30] who also recorded a high prevalence in males. EBV has been strongly associated with OHL [12,31]. It could be argued that the preponderance of OHL in males may be due to the mode of expression of Ebstein Barr Virus in oral epithelium which has been reported by Schiboski et al. [32] as being gender specific in favour of males.
Hyperpigmentation, which was the third most commonly observed oral lesion in this series was also observed to be associated with significant immunosuppression. This observation is consistent with that of Schiodt et al. [33] who also observed a correlation between oral hyperpigmentation and severe immunosuppression in HIV infected patients.
Low occurrence of oral ulcers and herpes labialis observed in this series is consistent with findings by Taiwo et al. [6] in Jos, Campisi et al. [28] in Tanzania and Ranganathan [34] in India.
Other oral lesions commonly reported in the scientific literature such as Kaposi’s sarcoma, xerostomia, herpes zoster e.t.c. were not observed in this series. The rarity of Kaposi Sarcoma in this study may be attributed to heterosexual transmission group investigated, whereas, Kaposi sarcoma is commonly found among homosexual men [35].
Observation in this series that in spite of cessation of local treatment, oral lesions cleared following 3 months HAART treatment in 80% of cases. This is consistent with studies cited in scientific literature [7-9,36] which reported absence of oral lesions after HAART initiation. However, 80% of patients not on HAART had persistent oral lesions following 3 months evaluation which suggests the importance and effectiveness of HAART on reduction of oral lesions in HIV infected patients.
5. CONCLUSIONS
In all of these studies, prevalence of oral lesions was over 30% which buttresses the importance of oral lesions as a clinical manifestation of HIV and AIDS infection. With progression of HIV disease indicated by low CD4 count, high viral load and late HIV stage of the disease, oral lesions were frequently seen. There was also significant reduction in oral lesions following 3 months treatment with HAART.
Integrated multidisciplinary management of HIV infected and AIDS patients should be encouraged to improve the well being of the affected patients. Oral examination should also be made compulsory in the management of all HIV/AIDS patients, and patients with greater risks of infection.
REFERENCES
- Centers for Disease Control and Prevention (1993) Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recommendation and Reports, 41, 1-19.
- McNeil, D.G. Jr. (2007) U.N. agency to say it overstated extent of HIV cases by millions. New York Times.
- Greenspan, J.S., Barr, C.E., Sciubba, J.J. and Winkler, J.R. (1992) Oral manifestations of HIV infection. Oral Surgery, Oral Medicine, Oral Pathology, 73, 142-144. Hdoi:10.1016/0030-4220(92)90185-S
- Kaminu, H.N. and Naidoo, S. (2002) Oral HIV lesions and oral health behaviour of HIV-positive patients attending the Queen Elizabeth II Hospital, Maseru, Lesotho. Journal of the South African Dental Association, 57, 479- 482.
- Pindborg, J.J. (1989) Classification of oral lesions associated with HIV infection. Oral Surgery, Oral Medicine, Oral Pathology, 67, 292-295. Hdoi:10.1016/0030-4220(89)90358-7
- Taiwo, O., Okeke, E.N., Otoh, E.C. and Danfillo, I.S. (2005) Prevalence of HIV-related oral lesions in Nigerian women. Nigerian Journal of Medicine, 14, 132-136.
- Patton, L.L. (2000) Sensitivity, specificity and positive predictive value of oral opportunistic infections in adults with HIV/AIDS as markers of immune suppression and viral burden. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 90, 294-298.
- Schmidt-Westhausen, A.M., Priepke, F., Bergman, F.J. and Riechart, P.A. (2000) Decline in the rate of Oral opportunistic infections following introduction of HAART. Journal of Oral Pathology & Medicine, 29, 336-341. Hdoi:10.1034/j.1600-0714.2000.290708.x
- Tappuni, A.R. and Fleming, G.J.P. (2001) The effect of antiretroviral therapy on the prevalence of oral manifestations in HIV-infected patients: A UK study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 92, 623-628. Hdoi:10.1067/moe.2001.118902
- EEC-Clearinghouse (1993) EEC-Clearinghouse on oral Problems Related to HIV Infection and WHO Collaboration Center on oral manifestations of the immunodeficiency Virus. Classification and diagnostic criteria for oral lesions in HIV infection. Journal of Oral Pathology & Medicine, 22, 289-291.
- World Health Organization (2005) Interim WHO clinical staging of HIV/ AIDS and HIV/AIDS case definitions for surveillance: African region. 1-42.
- Iain, L.C. and Hamburger, J. (2000) The significance of oral health in HIV disease. Sexually Transmitted Infections, 76, 236-243.
- Butt, F.M.A., Vaghela, V.P., Chindia, M.L. and Mandalia, K. (2001) Oral manifestation of HIV/AIDS in Kenyan Provincial Hospital. East African Medical Journal, 78, 389-401. Hdoi:10.4314/eamj.v78i8.8988
- Matee, M., Scheutz, F. and Moshy, J. (2000) Occurrence of oral lesions in relation to clinical and immunological status among HIV infected adult Tanzanians. Oral Diseases, 6, 106-111. Hdoi:10.1111/j.1601-0825.2000.tb00110.x
- Glick, M., Muzyka, B.C., Lurie, D. and Salkin, L.M. (1994) Oral manifestations associated with HIV-related disease as markers for immune suppression and AIDS. Oral Surgery, Oral Medicine, Oral Pathology, 77, 344- 349. Hdoi:10.1016/0030-4220(94)90195-3
- Arotiba, J.T., Adebola, R.A., Iliyasu, Z., Babashani, M., Shokunbi, W.A., Ladipo, M.M.A. et al. (2005) Oral manifestations of HIV/AIDS infection in Nigerian patients seen in Kano. Nigerian Journal of Surgical Research, 7, 176-181.
- Taiwo, O.O., Okeke, E.N., Jalo, P.H. and Danfillo, I.S. (2006) Oral manifestation of HIV/AIDS in Plateau state indigenes, Nigeria. West African Journal of Medicine, 25, 32-37.
- Arotiba, J.T., Arowojolu, M.O., Fasola, A.O., Denloye, O.O. and Obiechina, A.E. (2006) Oral manifestation of HIV/AIDS. African Journal of Medicine and Medical Sciences, 35, 13-18.
- Adedigba, M.A., Ogunbodede, E.O., Jeboda, S.O. and Naidoo, S. (2008) Patterns of oral manifestation of HIV/ AIDS among 225 Nigerian patients. Oral Diseases, 4, 314-316.
- Onunu, A.N. and Obueke, N. (2002) HIV-related oral diseases in Benin City, Nigeria. West African Journal of Medicine, 21, 9-11.
- Wright, A.A. and Agbelusi, G.A. (2005) Group II and III lesions in HIV positive Nigerians attending the general Hospital Lagos, Nigeria. OdontoStomatologie Tropicale, 28, 19-23.
- Katz, M.H., Mastrucci, M.T., Leggott, P.J., Westenhouse, J., Greenspan, J.S. and Scott, G.B. (1993) Prognostic significance of oral lesions in children with perinatally acquired HIV infection. American Journal of Diseases of Children, 147, 45-48.
- Hamza, O.J., Matee, M.I., Simon, E.N., Kikwilu, E., Moshi, M.J., Mugusi, F. et al. (2006) Oral manifestations of HIV infection in children and adults receiving highly active anti-retroviral therapy [HAART] in Dar es Salaam, Tanzania. BMC Oral Health, 6, 12. Hdoi:10.1186/1472-6831-6-12
- Anteyi, K.O., Thacher, T.D., Yohanna, S. and Idoko, J.I. (2003) Oral manifestation of HIV/AIDS in Nigerian patients. International Journal of STD & AIDS, 14, 395-398. Hdoi:10.1258/095646203765371286
- Agbelusi, G.A. and Wright, A.A. (2005) Oral lesions as indicators of HIV infection among routine dental patients in Lagos, Nigeria. Oral Diseases, 11, 370-373. Hdoi:10.1111/j.1601-0825.2005.01132.x
- Greenspan, D. and Greenspan, J.S. (1996) HIV-related oral disease. The Lancet, 348, 729-733. Hdoi:10.1016/S0140-6736(96)02308-2
- Arendorf, T.M. Bredekamp, B. and Cloete, C.A.C. (1998) Oral manifestations of HIV infection in 600 South African patients. Journal of Oral Pathology & Medicine, 27, 176-179.
- Campisi, G., Pizzo, G., Mancuso, S. and Margiotta, V. (2001) Gender differences in HIV-related oral lesions: An Italian study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 91, 546-551.
- Nittayananta, W., Chanowanna, N., Slipapojakul, K., Rodklal, A., Jaruratanasirikul, S. and Liewchanpatana, K. (2002) Co-existence between oral lesions and opportunity systemic diseases among HIV-infected subjects in Thailand. Journal of Oral Pathology & Medicine, 31, 163-168. Hdoi:10.1034/j.1600-0714.2002.310307.x
- Kerdpon, D., Pongsiriwet, S., Pangsomboon, K., Lamrooz, A. and Kampoo, K. (2004) Oral Manifestation of HIV infection in relation to clinical and CD4 immunological status in Northern and Southern Thai patients. Oral Diseases, 10, 138-144. doi:10.1046/j.1601-0825.2003.00990.x
- Greenspan, D., Greenspan, J.S. Conant, M., Peterson, V., Silverman, S. and De Sonza, Y. (1984) Oral “Hairy” leukoplakia in male homosexuals: Evidence of association with both papilloma virus and a herpes group virus. The Lancet, 324, 831-834. Hdoi:10.1016/S0140-6736(84)90872-9
- Shiboski, C.H., Hilton, J.F. Neuhaus, J.M., Canchola, A. and Greenspan, D. (1996) HIV-related oral manifestations and gender. A longitudinal analysis. Archives of Internal Medicine, 156, 2249-2254. Hdoi:10.1001/archinte.1996.00440180113014
- Schiodt, M., Bakilana, P.B., Haza, F.R. et al. (1990) Oral candidiasis and hairy leukoplakia correlate with HIV infection. Oral Surgery, Oral Medicine, Oral Pathology, 69, 591-596. Hdoi:10.1016/0030-4220(90)90242-K
- Ranganathan, K., Reddy, B., Kumarasamy, N., Solomon, S., Viswanathan, R. and Johnson, L. (2000) Oral lesions and conditions associated with HIV infection in 300 South Indian patients. Oral Diseases, 6, 152-157. Hdoi:10.1111/j.1601-0825.2000.tb00326.x
- Holms, H.K. and Stephen, L.X.G. (2002) Oral lesions of HIV infection in developing countries. Oral Diseases, 8, 40-43. Hdoi:10.1034/j.1601-0825.2002.00010.x
- Cauda, R., Tacconelli, E., Tumbarelo, M., Morace, G., De Bernadis, F., et al. (1999) Role of protease inhibitor in preventing recurrent oral candidosis in patients with HIV infection: A prospective case-control study. Journal of Acquired Immune Deficiency Syndromes, 21, 20-25. Hdoi:10.1097/00126334-199905010-00003H
NOTES
*Corresponding author.

