Advances in Entomology
Vol. 1 No. 2 (2013) , Article ID: 38593 , 4 pages DOI:10.4236/ae.2013.12008
Post-intervention assessment of long-lasting insecticide nets (LLINs) distributed in the Kano metropolis, Kano State, Nigeria
![]()
Department of Biological Science, Bayero University, Kano, Nigeria; *Corresponding Author: zamah09@gmail.com
Copyright © 2013 Gobir Zainab, Tukur Zainab. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 19 June 2013; revised 24 August 2013; accepted September 13, 2013
Keywords: LLINs; Cone Bioassay; Mortality; Knockdown; Nigeria
ABSTRACT
Kano state has distributed about 4,137,464 Long Lasting Insecticide Nets (LLINs) in 2009 being one of the main malaria vector control strategy developed by the Nigeria Federal Ministry of Health (FMOH) in line with Roll Back Malaria. The objective of the study was to evaluate the effectiveness of LLINs in use, the knowledge, attitude and practices of some net users in the Kano metropolis. A Cone bioassay with laboratory reared Anopheles was performed. Knockdown after 60 minutes and mortality after 24 hours followed with a 3 minutes exposure were evaluated. A total of 210 households were administered with a structured questionnaire on two hundred and five (205) respondents (97.6%) indicated knowledge about LLINs while five (5) respondents (2.4%) were not aware. Very high and consistent knockdown and mortality in all 5 replicates were found. Respondent still holds some reservation on the use of LLINs, and one hundred and five respondents (54.8%) believed it causes heat. The respondents replied that they did not rely mostly on LLINs, despite their beliefs in the efficacy of it rather. 41.4% of the people that participated in the research still resorted to use of aerosols and 26.2% use smoke screens to prevent mosquito bites. It can be concluded from the findings that respondents were aware of long lasting insecticide net and agreed on its effectiveness against the vector of malaria parasite and other insects, with some having reservations on the use of smoke screens and indoor residual insecticide sprays to prevent mosquito bites. Considering that the nets are expected to be effective for three years or more years, it is reasonable to conclude that the nets were effective in preventing mosquito bites based on the knock-down and exposure mortality results obtained during this study.
1. INTRODUCTION
Insecticide-treated nets (ITNs) have been shown to be the most cost-effective prevention method against malaria and are part of WHO’s Millennium Development Goals (MDGs) [1]. ITNs are the most powerful malaria control tool to be developed since the advent of indoor residual spraying (IRS) and chloroquine in the 1940s, and as such they have been an important component of global and national malaria control policies since the mid-1990s [2]. Only 3% of African children are currently sleeping under ITNs, and only about 20% are sleeping under any kind of net [3]. So, while progress with increasing coverage to date has been slow, there is now global support for the rapid scale-up of ITNs among vulnerable groups by integrating ITNs delivery with maternal and child health programmes (and immunization in particular), at the same time working with the private sector in a complementary and supportive manner to ensure that coverage can be maintained for future generations of African children [2].
An insecticide-treated net is a mosquito net that repels disables and/or kills mosquitoes coming into contact with insecticide on the netting material. There are two categories of ITNs: conventionally treated nets and long-lasting insecticidal nets [4]. A conventionally treated net is a mosquito net that has been treated by dipping in a WHO recommended insecticide. To ensure its continued insecticidal effect, the net should be re-treated after three washings, or at least once a year. A long-lasting insecticidal net is a factory treated mosquito net made with netting material that has insecticide incorporated within or bound around the fibres [4]. The net must retain its effective biological activity without re-treatment for at least 20 WHO standard washings under laboratory conditions and three years of recommended use under field conditions. One of the main factors which affect the efficacy of ITNs is their retreatment every 6 to 12 months with insecticides [4]. Most malaria-carrying mosquitoes bite at night. Mosquito nets, if properly used and maintained, can provide a physical barrier to hungry mosquitoes. If treated with insecticide, the effectiveness of nets is greatly improved, generating a chemical halo that extends beyond the mosquito net itself [4]. This tends to repel or deter mosquitoes from biting or shorten the mosquito’s life span so that she cannot transmit malaria infection. Often people who are unfamiliar with ITNs, or who are not in the habit of using them, need to be convinced of their usefulness and persuaded to re-treat the nets with insecticide on a regular basis. In response to the low retreatment rates of the bed nets, especially in Africa, Long-Lasting Insecticide Nets (LLINs) have been developed which require no further treatment throughout their expected life span of about three years or even more, making them more convenient and preferred over the conventional ones [5].
LLINs are polyethylene nets with 2% permethrin incorporated within the fibres. Over time, insecticide migrates to the surface of the yarn, replacing the one that has been removed by washing [5]. These are the LLINs recommended by the WHO and distributed in Nigeria by the Malaria Control Programme. Some mosquito species, such as Aedesaegypti [6] and Anopheles arabiensis [6], were found to be resistant to permethrin in some studies. This raised concerns about the resistance of Anopheles mosquitoes to permethrin. There are also concerns about the effectiveness of LLINs a year or more after their distribution.
Nigeria has renewed its commitment through National Malaria Control Program and the Roll-Back Malaria partners to reducing the malaria burden by half by the end of the year 2010. One of its strategies is to distribute 63 million long-lasting insecticide nets known as LLINs, to 32 million households in all the 36 states and the Federal Capital Territory (FCT). The largest campaign is the largest distribution of LLINs in the world [7].
2. MATERIAL AND METHODS
2.1. Study Area
Kano State is located in the North Western geopolitical zone of Nigeria. Historically, Kano State has been a commercial and agricultural state which is known for the production of ground nuts, as well as having mineral deposits. This study was a multi-centred study that comprised of eight (8) Local Government Areas randomly sampled within the Kano metropolis.
2.2. Sampling
30 by 7 cluster sampling technique described by the WHO [8] were used in this study, because of its appropriateness. As a two-stage cluster sampling process, firstly, 30 clusters were selected from a total of 88 wards in Kano metropolis where bed nets had been distributed more than one year ago. In each cluster, the first household was selected randomly from the list of houses. The other 6 houses within each cluster were then selected starting from the closest house to the first moving to the next closest and until the last household. A total of 210 bed nets were enumerated from household sampled.
2.3. Data Collection Procedure
Households were randomly selected from the list until a total of 210 households were obtained in the eight (8) local government areas in which the occupants still possess at least one LLINs during the questionnaire administration. All the households selected, would have received one or more LLINs, and if a household selected did not have LLINs, the next household was selected. Consent of the household were obtained to carry out the study, after which a proper explanation of the study was given to the household and questionnaire administered. Bioassay was carried out for the evaluation of the effectiveness of long lasting insecticide net (LLINs) using the WHO cone test: In this method, non-blood-fed Anopheles mosquitoes 2 - 3-day-old was exposed to netting materials under standard WHO plastic cones for 3 minutes and clipped to it to prevent mosquitoes escaping through the nets. Batches of only 20 females were introduced into each of the five cones that are applied to the same net sampled to minimize the chances of mosquitoes disturbing each other during the short exposures. Mosquitoes exposed to untreated nets was used as controls. After exposure, females Anopheles were transferred into 150-ml plastic cups, by aspiration, containing 10% sucrose and maintained in a bioassay cylinder for 24 hours at ambient condition. The number knocked down after 60 minutes was recorded and percentage mortality after 24 hours was calculated [9].
2.4. Data Analysis
Descriptive statistics was used to analyze the frequency, percentage, mean and standard deviation. Inferential statistics such as chi square (χ2) was used SPSS version 15.0 was used for analyses of all data and a probability level (P < 0.05) was regarded as significance.
3. RESULT
A total of 210 households were administered with a structured questionnaire. Households’ characteristics of sex, age, marital status and occupation served as the major parameters or determinant variables in the questionnaire. By sex, the males constituted 18.1% (38 respondents) of the sampled population compared to the females with 81.9% (172 respondents). Age ranges from 15 and 55 years with a mean age 39 ± 7.6.
Table 1 below indicates the full awareness of LLINs with two hundred and five (205) respondents 97.6% indicated the knowledge while five (5) respondents 2.4% were not aware.
Table 2 below shows that, 42 (20%) were children were infected with malaria and others cut across pregnant women mothers and everybody.
Table 3 shows that, 98 (46.7%) respondents used LLINs as mode of treatment of malaria while others cut across IRS and Anti malaria drugs.
Table 4 shows statistical description of knockdown after 60 minutes and mortality after 24 hours of Anopheles mosquitoes.
4. DISCUSSION
Two hundred and ten (210) households were sampled. Household findings show that respondents were fully aware LLINs as shown in Table 1. In the study from Western Ethiopia, the possession of bed net, the willingness to pay for the nets and their actual use were associated with wealth status [10]. Furthermore, the mean number and use of LLINs in the current study were influenced by the education level of the head of household as in Table 1. This finding confirms results from [11], who observed that higher education attainment was associated with a higher likelihood of household purchasing both treated and untreated bed nets, although in a study from Western Cote d’lvoire, [12] found that the education level of the respective head of household had no influence.
42 (20%) children were exposed to malaria and others cut across everybody, pregnant women and women as shown in Table 2. The cause of the malaria may be due to non use of bed nets and may also give the impression that bed nets are simply luxury items and not a priority for malaria control in endemic areas [13,14]. This may put the community at more risk of malaria infection mainly because the relatively perceived low vector density may be efficient enough in infecting people and transmitting the plasmodium parasite among the population. 98 (46.67%) respondents used LLINs as a mode of treatment of malaria while others cut across IRS and anti malaria drugs as shown in Table 3. This is in concor
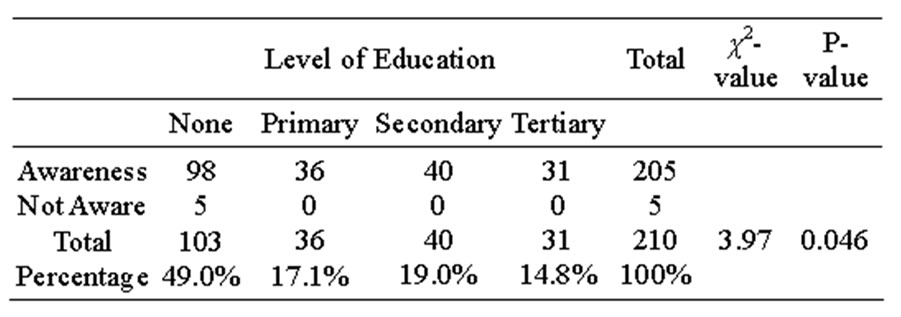
Table 1. Awareness on the use of LLINs in relation to level of education.
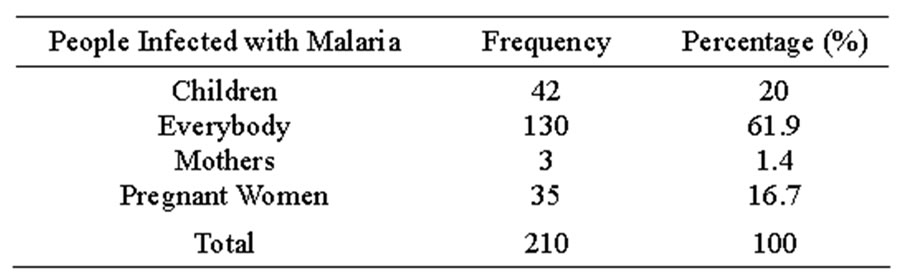
Table 2. Malaria incidence.
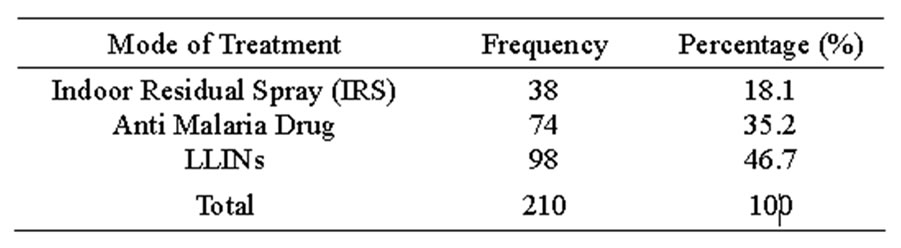
Table 3. Mode of treatment of malaria.
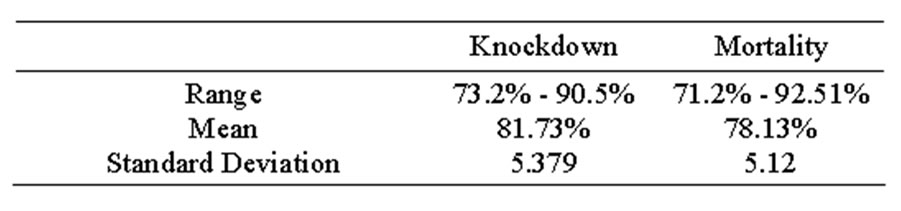
Table 4. Descriptive statistics showing the knockdown rate of mosquitoes after 60 minutes and mortality after 24 hours.
dance with Berman’s study in Africa who studied effective use of LLINs in reducing malaria [15]. Between 1986 and 2002, at least 81 trials and over 30 descriptive studies carried out in every type of malaria setting worldwide have documented the positive impact of LLINs on child and adult morbidity and mortality [16]. Most of these studies were summarized by Lengeler in 2004.
LLINs are now important methods of controlling malaria. The protective effect will be stronger if they are used by a high proportion of the population at risk.
Table 4 shows that the LLINs are still effective after three years of distribution in the study area. The result of the present study is in concordance with the study in Sudan [17] where both show that Olyset were very efficacious 70% and 92.1% reduction, respectively.
The tendency for mosquitoes to avoid touching the Olyset fibre might be partially caused by irritation to mosquitoes due to permethrin. [18] emphasized the irritant effects of permethrin to Anopheles mosquitoes and it is this pyrethroid which is incorporated into Olyset nets during manufacture. Tests in Cote d’lvoire of efficacy of Olyset nets showed deterrence to hut entry of An. gambiae [18].
5. CONCLUSION
It can be concluded from the findings that respondents were fully aware of long lasting insecticide net and they agreed that it is effective against the vector causing malaria parasite and other insects though some of them have reservation on the use of smoke and indoor residual spray to prevent mosquitoes bite. Considering that the nets are expected to be effective for three years or more years, it is reasonable to conclude that the nets were effective in preventing mosquito bites based on the knockdown and exposure mortality results.
REFERENCES
- World Health Organization (2002) World health report: Reducing risks, promoting healthy life. World Health Organization, Geneva. http://www.who.int/whr/2002/en/whr02_en.pdf
- Hill, J., Lines, J. and Rowland, M. (2006) Insecticidetreated nets. Advances in Parasitology, 61, 77-128. http://dx.doi.org/10.1016/S0065-308X(05)61003-2
- Himeidan, Y.E., Chen, H., Chandre, F., Donnelly, M.J. and Yan, G. (2007) Permethrin and DDT resistance in the malaria vector Anopheles arabiensis from eastern Sudan. American Journal of Tropical Medicine and Hygiene, 77, 1066-1068.
- Lengeler, C. (2004) Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database System Revision. http://dx.doi.org/10.1002/14651858.CD000363.pub2
- World Health Organization (2007) Insecticide-treated mosquito nets: A WHO position statement. www.who.int/malaria/publications/atoz/itnspospaperfinal/en/index.html
- Prapanthadara, L., Promtet, N., Koottathep, S., Somboon, P., Suwonkerd, W., Mc Carroll, L. and Hemingway, J. (2002): Mechanisms of DDT and permethrin resistance in Aedesaegypti from Chiang Mai, Thailand. Dengue Bulletin, 26, 185-189.
- UNICEF Nigeria (2010) UNICEF says malaria is still number one killer of children underfive in Nigeria. www.unicef.org/Nigeria/media
- Hoshaw-Woodard, S. (2001) Description and comparison of the methods of cluster sampling and lot quality assurance sampling to assess immunization coverage. WHO— Department of Vaccines and Biological, Geneva.
- Kroeger, A., Mancheno, M., Alarcin, J. and Pessek, L. (1995) Insecticide-impregnated bed nets for malaria control varying experiences from Ecuador, Colombia and Peru concerning acceptability and effectiveness. America Journal Tropical Medicine and Hygiene, 53, 313-323.
- Legesse, Y., Tegegn, A., Belachew, T. and Tushune, K. (2007) Households willingness to pay for long-lasting insecticide treated nets in three urban communities of Assosa zone, western Ethiopia. Ethiopia Medicine Journal, 45, 353-362.
- Dike, N., Onwujekwe, O., Ojukwu, J., Ikeme, A., Uzochukwu, B. and Shu, E. (2006) Influence of education and knowledge on perceptions and practices to control malaria in southeast Nigeria. Society of Science and Medicine, 63, 103-106. http://dx.doi.org/10.1016/j.socscimed.2005.11.061
- Fürst, T., Raso, G., Acka, C.A., Tschannen, A.B., N’Goran, E.K. and Utzinger, J. (2009) Dynamics of socioeconomic risk factors for neglected tropical diseases and malaria in an armed conflict. PLoS Neglected Tropical Diseases, 3, 513. http://dx.doi.org/10.1371/journal.pntd.0000513
- Klein, R.E., Weller, S.L., Zeissig, R., Richards, F.O. and Reubush, T.K. (1995) Knowledge, beliefs and practices in relation to malaria transmission and vector control in Guatemala. America Journal Tropical Medicine and Hygiene, 52, 383-388.
- Schellenberg, J.R., Abdulla, S. and Nathan, R. (2001) Effect of large-scale social marketing of insecticidetreated nets on child survival in rural Tanzania. Lancet, 357, 1241-1247. http://dx.doi.org/10.1016/S0140-6736(00)04404-4
- Berman, J.D. (1997) The effectiveness of insecticide treated net in reducing cases of malaria infections. America Journal of Tropical Medicine and Hygiene, 52, 377- 382.
- World Health Organization (1998) Test procedures for insecticide resistance monitoring in malaria vectors, bioefficacy and persistence of insecticides on treated surfaces. WHO Informal Consultation, Geneva, 28-30 September 1998, 46p.
- Hassan, S.El-D.H., Malik, E.M., Okoued, S.I. and Eltayeb, E.M. (2008) Retention and efficacy of long-lasting insecticide-treated nets distributed in eastern Sudan: A two-step community-based study. Malaria Journal, 7, 85. http://dx.doi.org/10.1186/1475-2875-7-85
- Miller, J.E., Jones, C.O.H., Ndunguru, S., Curtis, V. and Lines, J. (1999) A new strategy for treating nets. Part 2: Users’ perceptions of efficacy and washing practices and their implications for insecticide dosage. Tropical Medicine and International Health, 4, 167-174.

