Open Access Library Journal
Vol.03 No.04(2016), Article ID:69167,7 pages
10.4236/oalib.1102118
Successful Treatment of a Supralethal Dose Paraquat Poisoning and Follow-Up Report
Fahuan Yuan, Feng Chen, Yiqin Wang, Daihong Wang
Department of Nephrology, Xinqiao Hospital, Chongqing, China

Copyright © 2016 by authors and OALib.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 21 March 2016; accepted 4 April 2016; published 7 April 2016

ABSTRACT
Serious exposure to paraquat (more than 10 ml 20% paraquat) usually results in death due to progressive pulmonary fibrosis. We report successful treatment of an 83-year-old male who ingested 50 ml 20% paraquat and the follow-up result after 19 months. Our successful treatment might due to early and enough gastric lavage, superhigh dose of steroids and ambroxol, and early and long process of blood purification. At follow-up, the patient’s general condition, laboratory reports, pulmonary function, and chest radiography remain relatively normal. This successful case suggested that paraquat caused pulmonary fibrosis was reversible, and that paraquat had no long- time side effect to lung, liver, kidney, heart, and marrow if the patient received enough and perfect therapy in time.
Keywords:
Paraquat Poisoning, Steroids, Ambroxol, Blood Purification
Subject Areas: Toxicology

1. Introduction
1.1. Primary Treatment Process in Local Hospital
A 83-year-old male (a peasant in Lianpin County of Chongqing, China) was admitted to Lianpin Traditional Chinese Medicine Hospital at 11:10 July 26th 2011, because he ingested 50 ml of 20% paraquat (produced by the Planck bio-chemical industry Co. LTD) 10 minutes ago. The patient ingested paraquat in a building close to the hospital due to dispute and fell down immediately without coma and convulsion, and then was sent to the hospital. In Lianpin Traditional Chinese Medicine Hospital, the gastric lavage with 15,000 ml physiological saline was performed, then 60 g activated charcoal and 20 g magnesium sulfate were dissolved and injected from the gastric tube, and then hemodialysis (B Braun Co. LTD Lops15 dialyser) plus hemoperfusion (Zhuhai Jianfan Co. LTD HA130 neutral resina cask) for 4 hours by the right internal jugular venous catheter were carried out. When admission, the physical examination and the laboratory tests, including urinalysis, blood routine, liver function, renal function, blood glucose, blood lipid, thrombin test, electrolytes, total CO2 and electrocardiogram were normal. After hemodialysis, the patient was transferred to Nephrology Department of Xinqiao Hospital of Third Military Medical University.
1.2. The Treatment Process in Nephrology Department of Xinqiao Hospital
The patient was admitted to Xinqiao Hospital (ID 03679470) at 00:19, July 27th 2011.
Chief complaint
The patient suffered from palpitation and weak, with only 600 ml urine and without defecation in 14 hours.
Physical Examination
His temperature was 36.8˚C, pulse rate 87/minute, respiratory rate 20/ minute, blood pressure 139/87mmHg. The patient lied down in bed with active position, looked ill but remained conscious with good orientation of time, place and person. Skin and Lymph nodes was normal. There was no eyelid edema or icteric sclera. The pupils were symmetric. The chest showed normal with symmetrical expansion, without pulmonary rales. The heart border and rhythm were normal without murmur. Liver and spleen were not touched. Spine, limbs, neuromuscular system were normal.
Laboratory Findings
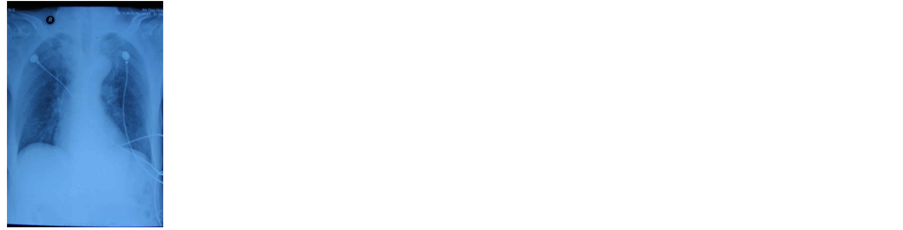
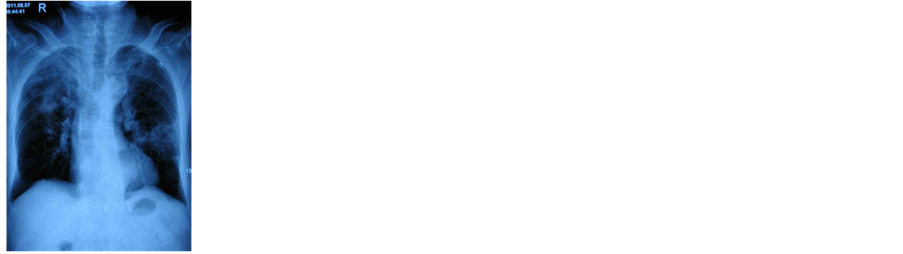
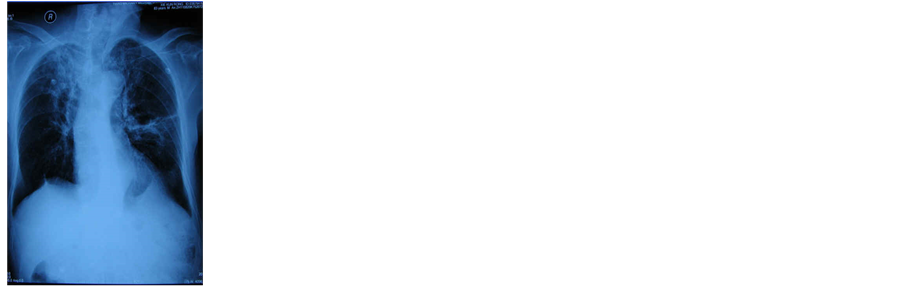
Blood routine: WBC11.98 × 109/L, N93.8%, the rest was normal. Urinalysis: protein (+), blood (+), glucose (+), specific gravity 1.010, pH 7.5. Renal function: Serum creatinine 76 μmol/L (0.85 mg/dl), serum urea 5.9 mmol/L (UN16.5 mg/dl), cystatin C 1.59 mg/L. Electrolytes: Serum sodium 129.6 mmol/L, the rest electrolytes were normal. Myocardial enzymes: lactic dehydrogenase(LDH) and alpha-hydroxybutyric dehydrogenase (α- HBDH) slightly increased, ischemia modified albumin, aspartate aminotransferase(AST), creatine phosphate kinase (CPK) and creatine kinase isoenzyme MB (CK-MB) were normal. Heart failure markers: b-type natriuretic peptide (B-NP) and troponin T (cTnT) were significantly increased. Electrocardiogram: sinus rhythm, heart rate was 81/min. Chest radiography: Aorta was dilated, the lungs had no obvious abnormality (Figure 1). Abdominal ultrasound: Liver, gall bladder, spleen, pancreas and kidney showed normal.
Diagnosis
Paraquat poisoning (Supralethal dose).
Treatment
The patient received 80 mg methylprednisolone and 1000 mg ambroxol each day for 20 days. Then, the methylprednisolone and ambroxol were gradually decreased, and stopped 28 days after poisoning. Twelve hours continuous venous-venous hemodialysis filtration(CVVHDF, with 1500 ml/h pre-dilution, 500 ml/h post-dilu- tion, and 2000 ml/h dialysis solutions, Gambro M100 filter) plus 2-hours hemoperfusion (Zhuhai Jianfan Co. LTD HA130 neutral resina cask) was performed each day for 20 days.
2. Results
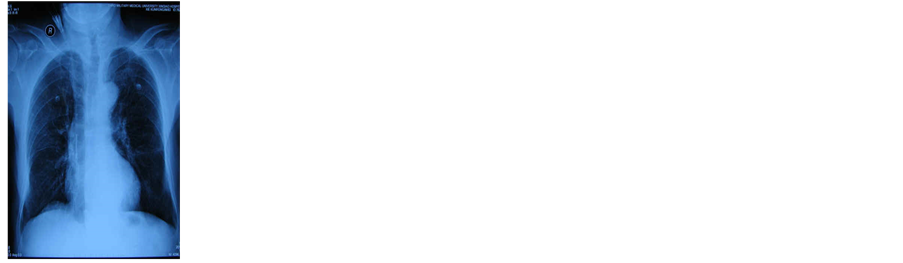
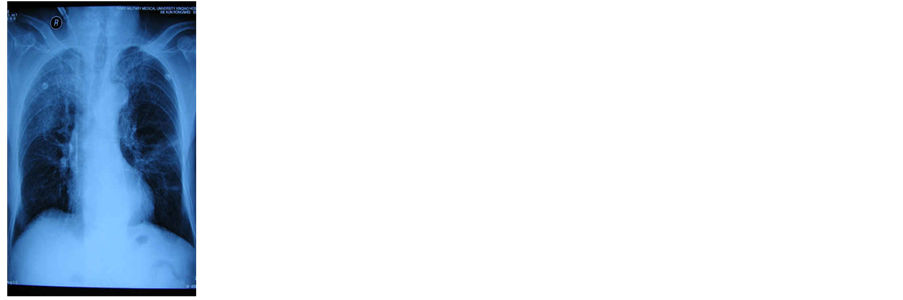
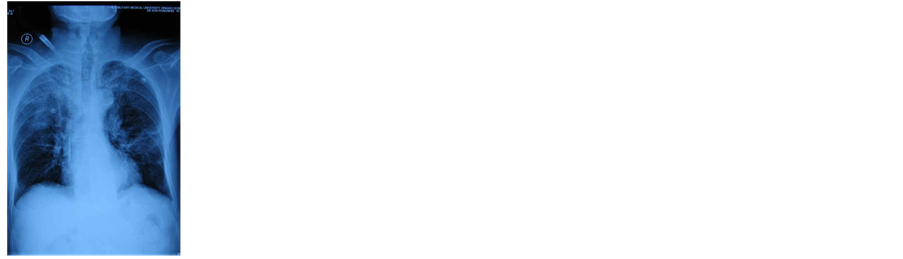
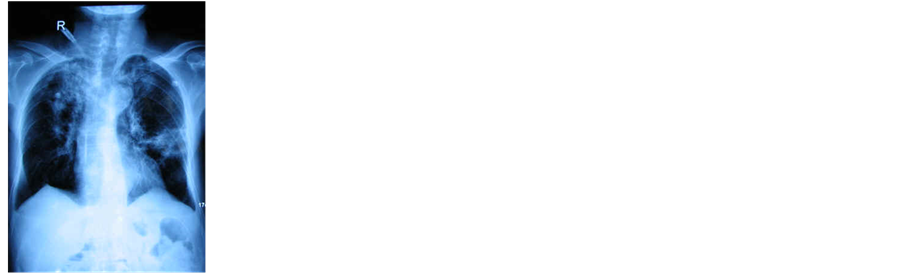
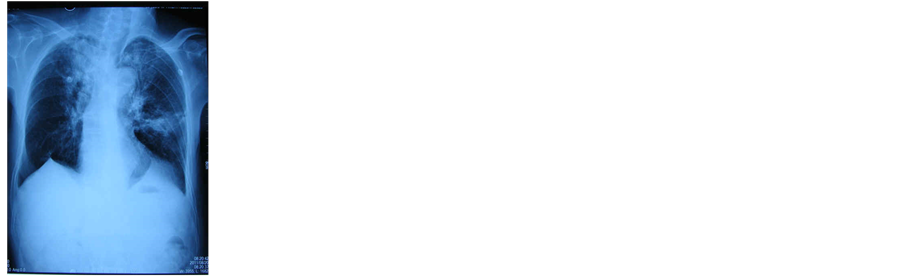
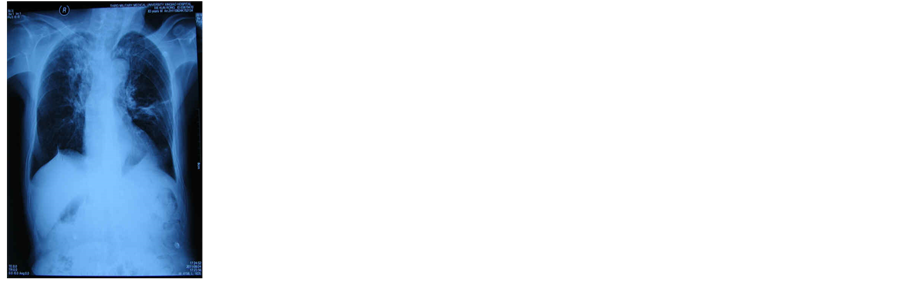
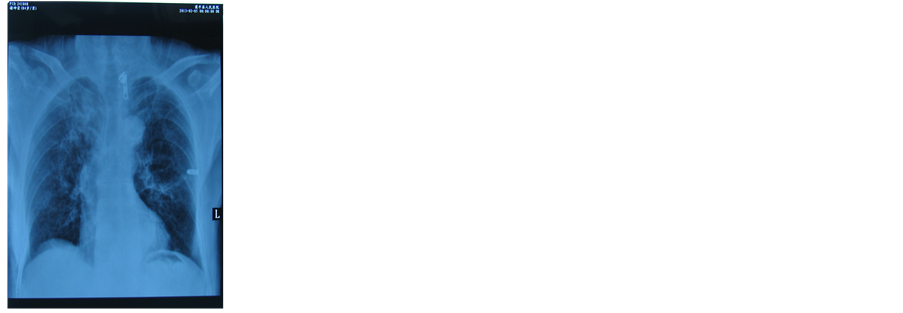
On the second day after admission (July 28th 2011), blood creatinine elevated to 188 μmol/L (2.1 mg/dl), and persisted to August 6th 2011(about 10 days). The heightened myocardial enzymes and heart failure markers persisted until August 25th 2011 (about 19 days). The laboratory assay results variation was shown in Table 1. On the 5th day after admission (August 2th 2011) both upper longs appeared interstitial lesion looked like ground glass (Figure 2), and showed gradual aggravation until August 7th 2011 (Figures 3-5), and relieved from August 12th 2011(about 16 days post poisoning, Figures 6-8). On August 29th 2011 (33 days post poisoning) only little pulmonary fibrotic lesion existed (Figure 9). The patient was discharged from hospital 34 days after admission with good feeling, and normal results of physical and biological examination.
3. Follow-Up
On February 5th 2013 (about 19 months after paraquat poisoning), the patient was in a good physical condition, and could do farm work. Chest X-ray film showed both lung marking increased slightly (Figure 10). Pulmonary function test showed that forced expiratory volume (FEV) was normal (4.1 L), maximal voluntary ventilation (MVV) slightly decreased (46.6 L/min), forced expiratory volume in 1 second (FEV1) moderately decreased (0.9 L), and the FEV1/FEV obviously decreased (21.8%). Laboratory tests: Blood routine and urinalysis were
Figure 1. The patient was admitted to Xinqiao hospital on July 27th 2011. The chest radiography showed that the lungs had no obvious abnormality.
Figure 2. The chest radiography on August 2nd 2011 showed that both upper lungs developed interstitial lesion which looked like ground glass.
Figure 3. The chest radiography of the patient from August 4th 2011 showed gradual aggravation of the lesion.
Figure 4. The chest radiography of the patient on August 5th 2011.
Figure 5. The chest radiography on August 7th 2011.
Figure 6. The chest radiography of the patient from August 12th 2011 showed that the lesion started to relieve.
Figure 7. The chest radiography of the patient on August 20th 2011.
Figure 8. The chest radiography of the patient on August 24th 2011.
Figure 9. The chest radiography on August 29th 2011 showed that only little pulmonary fibrotic lesion existed.
Figure 10. The chest radiography on February 5th 2013 showed both lungs marking increased slightly.
Table 1. The patient’s assay results in hospital.
normal. Blood glucose was slightly high (7.5 mmol/L, or 135 mg/dl). Blood creatinine was 88.5 μmol/L(1 mg/dl). Liver function and blood lipid were normal.
4. Discussion
Paraquat (l-l-dimethyl-4-4'-bipyridine) is a non-selective and quick-acting killer to green plant. Commercial paraquat usually presented as 20% aquatic solution. Molecular formula of paraquat is C12H14Cl2N2 and molar mass is 257.2. Paraquat was most widely used as herbicide in the world. Paraquat, when ingested, is highly toxic to mammals, including human without specific antidotes. The mortality is more than 90% when one ingested more than 10 ml of 20% paraquat aquatic solution. In spite of being prohibited or restricted use in more than 20 countries, paraquat is still widely used in 89 countries including China today.
Paraquat can be absorbed by human skin, digestive tract and respiratory tract, and quickly distributes to every tissues and organs especially the lungs. Paraquat hardly degrades in human body, and is usually discharged from the urine. Ingested paraquat can cause extensive system damage. Lungs are superlatively easily attacked [1] . Liver, kidney, heart and brain can also be attacked [2] - [5] . Although the patients can die due to multiple organ failure induced by paraquat in 1 week, but usually die due to progressive pulmonary fibrosis at 2 - 3 weeks post poisoning. The mechanisms of paraquat inducing tissue injury have not been fully understood. It is most suggested that excessive oxidative stress was related [1] [5] .
There is no specific antidote for paraquat poisoning. The most important intervention is as early as possible to discharge the toxin including vomiting, catharsis and gastric lavage [6] . There are some reports showing that the lysine acetylsalicylate [7] , steroid [8] and ambroxol [9] can reduce the injury of animal lungs caused by paraquat, but it is not verified in human. No reports have found that patient who ingested more than five times of lethal dose paraquat was successfully cured.
It was verified by the surveillance tap that this patient ingested paraquat. The positive urine glucose, hematuria, proteinuria, and progressively increasing serum creatinine after poisoning proved that the patient suffered from acute kidney injury (AKI). The increased LDH, BNP, α-HBDH and cTnT indicated obvious myocardial damage. The interstitial damage (ground-glass lesion) of both upper lungs appeared on the 5th day, and progressively aggravated, which conformed to the pulmonary fibrosis. All these clinical processes were compatible with severe paraquat poisoning. It is a miracle that 83-years old man who suffered from serious damages of lungs, kidney and heart caused by superlethal paraquat poisoning can survive due to successful treatment.
The successful treatment might be attributed to the following points: (1) Eliminating poison from gastrointestinal tract in time. The patient received gastric lavage for 15,000 ml in 20 minutes after poisoning, which eliminated most paraquat in stomach. The activated charcoal infused adsorbed the rest poison in intestinal system. (2) Enough and long-time blood purification. The patient received hemodialysis, filtration and hemoperfusion 12 hours per day for 20 days, which eliminated the blood paraquat dissociated from tissue gradually. There was no report about that which kind of blood purification and how long should be given to cure paraquat poisoning, and there was also no acknowledged indicators about when the blood purification should be stopped. The patient received blood purification until the assay results of cardio-renal damages became normal. The blood purification treatment for this patient lasted much longer than that for other patients with acute kidney injury. It was not certain whther such long-time blood purification was necessary. However, successful treatment of this patient suggested that enough and long-time blood purification was beneficial to the recovery of cardio-renal and pulmonary injury caused by paraquat. (3) Large dose of steroids and ambroxol. The pulmonary fibrosis induced by paraquat had similar pathological feature to severe acute respiratory syndrome (SARS) induced by the coronavirus in 2003. According to the successful experience to treat SARS in XiaoTangShan Hospital of Beijing in 2003, we gave the patient 80 mg methylprednisolone each day. There were some reports showing that the ambroxol has a special affinity with lung. The concentration of ambroxol in the lung was 20 times higher than that in the blood. In addition to the antitussive and expectorant function, the ambroxol also has antioxidant and stabilizing effects on lung cells. Large dose (990 mg/day) of ambroxol could relieve the pulmonary damage of patient who suffered from cervical spinal cord injury [10] . The paraquat also concentrates in the lung and damages the lung through overoxidation [5] . Inspired by the literature, we used large dose of ambroxol (1000 mg/d, which was 30 times to normal dose). The pulmonary fibrosis induced by paraquat was usually inreversible. Anyhow, this patient’s pulmonary fibrosis was under control on the 10th day after poisoning, relieved on the 15th day, and became normal on the 30th day. The healing of this patient suggested that the pulmonary fibrosis induced by the paraquat could be cured by the large dose of steroids and ambroxol. But the mechanism of large dose steroids and ambroxol treating pulmonary fibrosis caused by paraquat needs further research.
The patient’s blood glucose was normal without hand tremor while in hospital. But 19 months later, the patient’s blood glucose increased to 7.5 mmol/L (135 mg/dl) with obvious hand tremor. It is not sure whether these changes were primary disease or late effect of paraquat poisoning. During follow-up, the patient still worked in farm, his chest X-ray film and pulmonary function test showed stable, and his blood routine, urinalysis, hepatic and renal function test were normal. These follow-up results suggested that paraquat had not long-time side effect to lung, liver, kidney, heart, and marrow if the patient received enough and perfect therapy promptly.
Cite this paper
Fahuan Yuan,Feng Chen,Yiqin Wang,Daihong Wang, (2016) Successful Treatment of a Supralethal Dose Paraquat Poisoning and Follow-Up Report. Open Access Library Journal,03,1-7. doi: 10.4236/oalib.1102118
References
- 1. Dong, X.S., Hu, X.B., Liu, W., et al. (2012) Effects of RNA Interference-Induced Smad3 Gene Silencing on Pulmonary Fibrosis Caused by Paraquat in Mice. Experimental Biology and Medicine, 237, 548-555.
http://dx.doi.org/10.1258/ebm.2011.011280 - 2. Li, Q., Peng, X., Yang, H., et al. (2011) Deficiency of Multidrug and Toxin Extrusion 1 Enhances Renal Accumulation of Paraquat and Deteriorates Kidney Injury in Mice. Molecular Pharmaceutics, 8, 2476-2483.
http://dx.doi.org/10.1021/mp200395f - 3. Mandel, J.S., Adami, H.O. and Cole, P. (2012) Paraquat and Parkinson’s Disease: An Overview of the Epidemiology and a Review of Two Recent Studies. Regulatory Toxicology and Pharmacology, 62, 385-392.
http://dx.doi.org/10.1016/j.yrtph.2011.10.004 - 4. Litteljohn, D., Nelson, E., Bethune, C., et al. (2011) The Effects of Paraquat on Regional Brain Neurotransmitter Activity, Hippocampal BDNF and Behavioural Function in Female Mice. Neuroscience Letters, 502, 186-191.
http://dx.doi.org/10.1016/j.neulet.2011.07.041 - 5. Rappold, P.M., Cui, M., Chesser, A.S., et al. (2011) Paraquat Neurotoxicity Is Mediated by the Dopamine Transporter and Organic Cation Transporter-3. Proceedings of the National Academy of Sciences of the United States of America, 108, 20766-20771.
http://dx.doi.org/10.1073/pnas.1115141108 - 6. Gawarammana, I.B. and Buckley, N.A. (2011) Medical Management of Paraquat Ingestion. British Journal of Clinical Pharmacology, 72, 745-757.
http://dx.doi.org/10.1111/j.1365-2125.2011.04026.x - 7. Huang, W.D., Wang, J.Z., Lu, Y.Q., et al. (2011) Lysine Acetyl-salicylate Ameliorates Lung Injury in Rats Acutely Exposed to Paraquat. Chinese Medical Journal (Engl), 124, 2496-2501.
- 8. Zerin, T., Kim, Y.S., Hong, S.Y., et al. (2012) Protective Effect of Methylprednisolone on Paraquat-Induced A549 Cell Cytotoxicity via Induction of Efflux Transporter, P-Glycoprotein Expression. Toxicology Letters, 208, 101-107.
http://dx.doi.org/10.1016/j.toxlet.2011.10.019 - 9. Zhi, Q.M., Yang, L.T. and Sun, H.C. (2011) Protective Effect of Ambroxol against Paraquat-Induced Pulmonary Fibrosis in Rats. Internal Medicine, 50, 1879-1887.
http://dx.doi.org/10.2169/internalmedicine.50.5407 - 10. Li, Q., Yao, G. and Zhu, X. (2012) High-Dose Ambroxol Reduces Pulmonary Complications in Patients with Acute Cervical Spinal Cord Injury after Surgery. Neurocritical Care, 16, 267-272.
http://dx.doi.org/10.1007/s12028-011-9642-4