Open Access Library Journal
Vol.02 No.03(2015), Article ID:68123,8 pages
10.4236/oalib.1101393
Treatment of Children with Anorectal Malformations―10-Year Review
Sejdi Statovci1, Hysen Heta2, Nexhmi Hyseni1, Salih Grajçevci1, Murat Berisha1, Gani Çeku1
1University Clinical Centre of Kosovo, Clinic of Pediatric Surgery, Prishtina, Kosovo
2Hospital University Centre of Tirana “Mother Teresa” Albania, Tirana, Albania
Email: sejdistatovci@yahoo.com
Copyright © 2015 by authors and OALib.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 20 February 2015; accepted 8 March 2015; published 16 March 2015
ABSTRACT
Introduction: Anorectal malformations include a wide spectrum of congenital defects of the anus, anal canal and rectum, which are often combined with urogenital tract defects. They are often associated with congenital anomalies of other organ systems such as genitourinary, cardiovascular, digestive, skeletal, etc. Objectives: This study aimed to review the patients with anorectal malformations, diagnosis, different types of associated anomalies and their frequency, modalities of treatment, results of treatment and complications. Materials and Methods: Since 2010, we have performed a combined retrospective and prospective analysis of a total of 76 patients with anorectal malformations which were diagnosed and treated at our clinic between 2005 and 2014. Results: Of 76 patients with anorectal malformations, 48 were male (63.16%) and 28 female (36.84%). Anal stenosis was the commonest type (30.26%) followed by ARM without fistula (25.00%) and rectourethral fistula (18.42%). The most common associated anomalies were urogenital (49.12%), cardiovascular (21.05%), gastrointestinal (15.79%), and bone malformations (5.26%). 34 patients (44.74%) were treated primarily without colostomy. In 40 patients (52.63%) colostomy was performed after birth. PSARP was the procedure of choice in 76.92% of patients. 7 patients (9.21%) died in total. Constipation was present in 52.38% of all patients. Patients older than 3 years of age totally continent were 30.91%. Redo operations were performed in 5 patients (7.94%). Conclusion: Early diagnosis of anorectal malformations is very important. Some malformations such as anal stenosis are sometimes diagnosed beyond the neonatal age. Challenging problem still remains high percentage of children that suffer from fecal incontinence and constipation.
Keywords:
Anorectal Malformations, Anal Stenosis, Colostomy, Bowel Management, Children
Subject Areas: Surgery & Surgical Specialties

1. Introduction
Anorectal malformations include a wide spectrum of congenital defects of the anus, anal canal and rectum with an incidence of 1 per 4000 - 5000 live birth [1] - [3] , which mainly are diagnosed in the early neonatal period although some malformations like anal stenosis or vestibular fistula sometimes are diagnosed with delay. There is a wide spectrum of clinical presentation ranging from low types with no need for colostomy to high type anomalies requiring complex management, according to Wingspread classification ARM used to be classified into low, intermediate, or high type, depending upon whether the blind end of the bowel is located below, within, or above the levator sling [4] . Since 2005, the Krickenbeck classification of ARM has been used widely [3] [4] . Associated malformations of other organ systems are identified in 30% - 70% of children with ARM [5] [6] . The most common ones are those of urinary tract 20% - 54% [7] [8] , followed by vertebral 30% - 35%, cardiovascular anomalies 12% - 22% [9] [10] , gastrointestinal 10% [11] , etc. The presence of associated anomalies, their type, number of affected organs in the same patient play a crucial role in the survival rate and prognosis of treatment. Associated anomalies can be twice more frequent in patients with higher anomalies than those with lower lesions [12] .
Very important decision to be made in a neonate with ARM is whether the patient needs a colostomy or not. Surgical treatment of low type anomalies can be done at neonatal age with a single act without colostomy, while high type anomalies require surgical treatment in three stages beginning with colostomy. Various pediatric surgeons have reported treatment of high type anomalies with a single act without colostomy [13] . Posterior sagittal approach (PSARP), introduced by Alberto Pena became widely accepted as the standard approach for all types of imperforate anus [14] . This approach allowed surgeons to see directly the complex anatomy and relations of the rectum and genitourinary system and also made them possible to repair these defects under direct vision. Despite all advances in operative techniques and improvements of survival rate of these patients, there is a high incidence of postoperative fecal incontinence and constipation that occurs even after an excellent surgical repair. These complications are manageable by additional procedures such as the bowel management protocol, continent appendicostomy procedure and sometimes redo operations [15] - [17] .
2. Materials and Methods
Since 2010 we performed a combined retrospective and prospective analysis of 76 patients with anorectal malformations, diagnosed and treated at University Clinical Centre of Kosovo between 2005 and 2014. Retrospective part of this study was completed using patients’ records and database of Clinic of Pediatric Surgery and Clinic of Neonatology. Patients from that period were invited for evaluation of their postoperative functional outcome. In prospective part of study we recorded new patients, gathering more qualitative data especially intraoperative details. We have classified ARMs into high, intermediate and low according to Wingspread classification, but we used also Krickenbeck classification of ARM for defining the type of malformations, associated anomalies and postoperative functional outcome. Data for postoperative constipation were collected in a group of 63 patients starting as early as possible in life, since the parents reported it. Voluntary bowel movements and soiling were evaluated in a group of 55 patients older than 3 years of age.
3. Results
The incidence of ARM in our study was 1 per 4351 live births. Of 76 patients with anorectal malformations, 48 were male (63.16%) and 28 female (36.84%). Male-female ratio was 1.7:1. High type anomalies were present in 36.84%, intermediate 19.74% and low type were 43.42%. High ARMs were found in 47.92% of males and 17.86% of females. Intermediate ARMs were found in 18.75% of males and 21.43% of females. Low ARMs were observed in 33.33% of males and 60.71% of females. Anal stenosis was the most common type (30.26%) followed by ARM without fistula (25.00%) and recto-urethral fistula (18.42%) (Table 1).
In total 57 associated anomalies were seen in 40 patients (52.63%). 58.33% of male patients, and 42.86% of female patients were diagnosed with associated anomalies. Of all associated anomalies, 50.88% were found in patients with high type ARM, 19.30% in intermediate type and 29.82% in patients with low type (Chart 1). 12 patients (15.79%) had two or more associated anomalies. One patient with recto-urethral fistula had multiple associated anomalies (myelomeningocoela, gluteal cystic formation, hypospadia, undescended testis, penoscrotal transposition).
Table 1. Types of ARM according to Crickenbeck classification.
Chart 1. Distribution of associated anomalies in different types of ARM.
The most common associated anomalies were urogenital (49.12%) including hypospadia (7 patients), undes- cended testis (6), VUR (5), megaureter (3), hydronephrosis (3), ureter duplex (2), renal agenesis (1) and penoscrotal transposition (1). Cardiovascular anomalies (21.05%) presented with VSD (6), ASD (3) and Tetralogia Fallot (2). Gastrointestinal anomalies (15.79%) including oesophageal atresia with T-E fistula (8) and Meckel’s Diverticulum (1). Bone malformations were (5.26%) including pesequinovarus (1), pescalcaneovalgus (1) and agenesio tibiae (1). Sacrococcygealteratoma (1), Down’s syndrome (1), Myelomeningocele (1), Gluteal cystic formation (1), Inguinal Hernia (1) (Chart 2).
In 65 patients (85.53%) surgical treatment has been completed. Among them, 52.31% (N = 34) were treated primarily without colostomy and 47.69% (N = 31) with divided colostomy. Of patients without colostomy, PSARP or minimal PSARP was the procedure of choice in 20 patients (58.82%). 11 other patients (32.35%) were operated with Cut Back procedure. 3 patients (8.82%) underwent membrane excision and anoplasty. 30 of 31 patients with divided colostomy were treated with PSARP (96.77%). Only one patient was treated with laparascopic colo-anal pulthrough (3.23%). In total, PSARP or minimal PSARP was the procedure of choice in 50 patients (76.92%).
Group of 9 other patients with colostomy (not included in 65 finally treated patients) consist of 3 patients (3.95%) actually at colostomy stage waiting for final treatment, 2 “missing patients” (2.63%) with divided colostomy didn’t return to our clinic for further treatment and 4 patients (5.26%) that died after colostomy.
7 patients (9.21%) died in total. Two of them prior to any surgical treatment, one patient after minimal PSARP
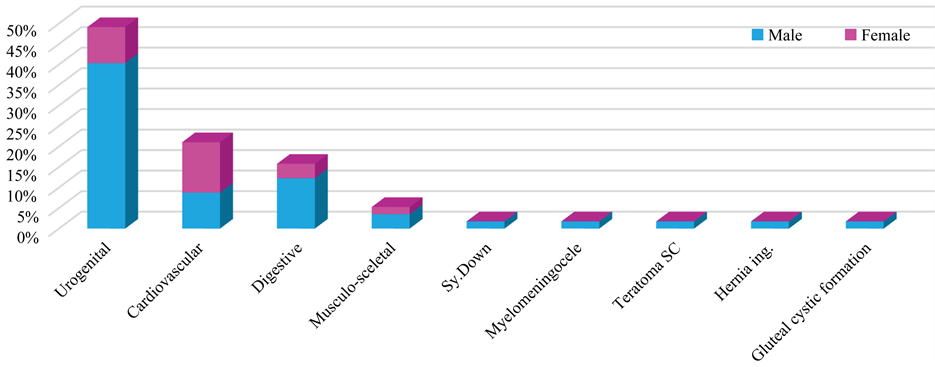
Chart 2. Distribution of associated anomalies in ARM.
and 3 patients with colostomy and one patient with colostomy and gastrostomy.
Postoperative complications (N = 10) happened in 9 patients (12.16%) as follows: prolapse of colostomy (2), wound dehiscence at the sight of colostomy (1) partial wound dehiscence after PSARP (2), adhesive ileus after colostomy (1), prolapse of rectal mucosa (2), anal stenosis (1) and urethral stenosis (1).
Postoperative constipation was present in 33 (52.38%) of 63 analyzed patients. Constipation was found 47.37% of male patients and 60% of female patients. Constipation of grade 1 was present in 10 patients (30.30%), grade 2 in 13 patients (39.39%), while the third grade constipation was found in 10 patients (30.30%).
Voluntary bowel movements and soiling were analyzed in a group of 55 patients older than 3 years of age. Voluntary bowel movements were present in 37 patients (67.27%). 20 of them (36.36%) still have soiling occasionally (grade 1 or 2), therefore totally continent are 17 patients (30.91%). 19 patients (34.55%) underwent bowel management procedures with daily enemas.
Five patients (7.94%) underwent redo operations because of poor outcome. 2 patients (3.18%) because of constipation, megarectum and overflow incontinence and 3 other patients (4.76%) because of fecal incontinence due to incorrect anorectal angle and misplaced anus and rectum. 7 other patients (9.21%) underwent redo opera- tions because of complications we mentioned above.
4. Discussion
The incidence of ARM in our study was 1 in 4351 live births, which is similar to the reported incidence in the literature [1] [2] . The male-female ratio in our study was 1.7:1 and matches the reported range of 1.2:1 to 2:1 in the literature [6] [18] [19] . In our study, high type lesions were more frequent in males (47.92% of male) than in females (17.86% of female) which is similar to other reports [6] [17] . Low ARMs were seen in 60.71% of female and in 33.33% of male patients. The rest percentage belongs to intermediate lesions.
Anal stenosis was found in 23 patients (30.26%) and it was the most common type in this study. Some of them have been treated for constipation, while their true diagnosis was not detected in time. Recto-urethral fistula is reported to be the most common lesion in male [20] . In our study the most common defect in male was Recto-urethral fistula equally as ARM without fistula (18.42%). In female, the most common lesion was anal stenosis―14 patients (18.42%). In this study there was one case of rectal atresia (1.32%) and one cloaca (1.32%) with 5 cm long common channel so we considered it as high type lesion.
The incidence of associated anomalies is reported to be 50% - 78% [21] - [23] . In our study we found them in 52.63% of patients. High ARMs are more frequently associated with other anomalies than low lesions [6] [12] [17] . Even in our study we found 50.88% of all other congenitalanomalies associated with high ARMs, 19.30% with intermediate and 29.82% associated with low ARMs (Chart 1). Urogenital defects were the most frequent (49.12%), similar to what is reported in literature about the frequency ranging from 26% to 59% of children with ARM [7] [8] [17] [18] . Consequently, all patients with ARM should undergo necessary investigations of kidneys, bladder and genitalia for early detection of additional anomalies. Hypospadias were the most common association (7 patients). Cardiovascular anomalies (ASD, VSD and Fallot tetralogy) were present in 21.05%. Echocardiography was done to all patients with ARM in Clinic of Neonatology. Their incidence in our study matches the reported incidence of 12% - 27% for cardiovascular anomalies [9] [10] [12] [17] [18] . The reported incidence of gastrointestinal anomalies ranges between 10% and 24% [11] [17] . In this study, they comprise 15.79% of all associated anomalies, represented by 8 patients with esophageal atresia (14.04%) and one patient with Meckels Diverticula. Esophageal atresia is also the most frequent anomaly throughout this study.
PSARP is the standard procedure in patients with high and intermediate type of ARM [14] [24] . In our study PSARP was the procedure of choice in 76.92% of patients (Figure 1). In patients without colostomy it was used in 58.82% (N = 20) but in patients with colostomy we used it in 96.77% (N = 30). Posterior sagittal approach, posterior plication of muscle complex and re-establishing of anorectal angle was used also in four redo operations while the fifth case was operated with abdomino-perineal approach (Figure 2). After redo operations we observed improvement in the functional outcome. Similar findings are reported also in literature [17] [25] [26] .
7 neonatal patients died during this study (9.21%). Similar percentage is reported in some of the literature [18] [27] [28] . Pneumonia, cardio respiratory failure, sepsis and acute renal failure were the causes of death. Two of them died prior to any surgical treatment, one after minimal PSARP, three after colostomy and the last one (with long gap esophageal atresia) after colostomy and gastrostomy was performed.
55 patients older than 3 years of age were analyzed for voluntary bowel movements and soiling using Krick- enbeck criteria for assessment of postoperative outcome [4] . Voluntary bowel movements were present in 67.27% but about half of them still have soiling occasionally therefore totally continent are considered 30.91%. Of 38 patients with soiling 27 had high ARMs, 19 patients (34.55%) underwent bowel management procedures with daily enemas. One enema daily resulted successful in 9 patients, making them able to remain most of the time clean. 5 patients need two enemas daily to remain completely clean. Three patients with fecal incontinence un- derwent redo PSARP, posterior plication of muscle complex and correction of anorectalangle. One patient still have soiling of grade 2 while the other has no more soiling but constipation occasionally. In the third patient,
Figure 1. Operative images of the Pena procedure.
Figure 2. Resection of megarectum and abdominoperineal pull through.
with poor developed muscle complex, the same procedures have been performed and the anterior plication with perineal body reconstruction. Results were not satisfying.
Postoperative constipation was present in 52.38% of 63 analyzed patients. Most of patients had the second grade constipation (39.39%). Twice more patients with low type anomalies were observed to have constipation than the patients with high ARM, which correlates with other reports [29] . Two patients (3.17%) with very resistant constipation with over-flow incontinence underwent redo operations due to a huge, dilated atonic rectum. Below we present details from suchcase: a female patient presented at the age of 14 years, with severe constipation and soiling of the third grade, despite regular enemas, laxatives and dietary modulation. She had been operated on four times previously, after being born with rectovestibular fistula; surgery included the formation and closure of a right upper quadrant colostomy. On examination she was found to have a normal sacrum, well-formed buttocks consistent with the subsequent intraoperative findings of good pelvic floor muscles. Her lower abdomen was distended with what appeared to be a huge fecaloma on bimanual examination, which also demonstrated a cavernous rectum. A barium study confirmed the megarectum. The patient underwent several enemas, despite which she had a large amount of rectal feces on examination under anesthetic. A laparotomy, with the intention of an abdominoperineal procedure, combined with rectal resection, was commenced. The huge rectum was resected than dissected down to the pelvic floor and a new anus was reconstructed via a posterior sagittal anorectoplasty, see Figure 2.
Of 9 patients with complications, 7 of them underwent reoperations. Colostomy revision was performed in 3 patients, redo anoplasty―2, laparotomy because of ileus―1, and one patient with anal and urethral stenosis was treated successfully with dilations of urethra and anus and actually is under close observation.
5. Conclusions
The clinical examination of patients with ARM is very important for the diagnosis of these anomalies. In our study, the most frequent defect was anal stenosis. As a result of careful search among patients who have been treated for constipation, their true diagnosis is not detected in time.
Associated anomalies are not often identified within the neonatal period, so research for them must continue even later in life.
According to our intraoperative findings during redo operations in patients with fecal incontinence, we have concluded that the correction of incorrect anorectal angle can give good results and significantly improve the patients’ quality of life.
Bowel management protocol when applied accurately, is very important in improving the quality of life of operated patients with ARM because it offers better opportunities for integration of the children in daily activities.
Conflict of Interest
There is no conflict of interests regarding the publication of this manuscript.
Cite this paper
Sejdi Statovci,Hysen Heta,Nexhmi Hyseni,Salih Grajçevci,Murat Berisha,Gani Çeku, (2015) Treatment of Children with Anorectal Malformations—10-Year Review. Open Access Library Journal,02,1-8. doi: 10.4236/oalib.1101393
References
- 1. Upadhyaya, V.D., Gangopadhyay, A.N., Srivastava, P., Hasan, Z. and Sharma, S.P. (2008) Evolution of Management of Anorectal Malformation through the Ages. The Internet Journal of Surgery, 17, 1.
- 2. Levitt, M.A. and Peña, A. (2010) Imperforate Anus and Cloacal Malformations. In: Holcomb III, G.W. and Murphy, J.P., Eds., Ashcraft’s Pediatric Surgery, 5th Edition, Saunders Elsevier, Philadelphia, 468-490.
http://dx.doi.org/10.1016/B978-1-4160-6127-4.00036-7 - 3. Gangopadhyay, A.N. and Pandey, V. (2015) Anorectal Malformations. Journal of Indian Association of Pediatric Surgeons, 20, 10-15.
http://dx.doi.org/10.4103/0971-9261.145438 - 4. Holschneider, A., Hutson, J., Peña, A., et al. (2005) Preliminary Report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. Journal of Pediatric Surgery, 40, 1521-1526.
http://dx.doi.org/10.1016/j.jpedsurg.2005.08.002 - 5. Peña, A. and Hong, A. (2000) Advances in the Management of Anorectal Malformations. The American Journal of Surgery, 180, 370-376.
http://dx.doi.org/10.1016/S0002-9610(00)00491-8 - 6. Endo, M., Hayashi, A., Ishihara, M., et al. (1999) Analysis of 1992 Patients with Anorectal Malformations over the Past Two Decades in Japan. Journal of Pediatric Surgery, 34, 435-441.
- 7. Goossens, W.J.H., de Blaauw, I., Wijnen, M.H., de Gier, R.P.E., Kortmann, B. and Feitz, W.F.J. (2011) Urological Anomalies in Anorectal Malformations in The Netherlands: Effects of Screening All Patients on Long-Term Outcome. Pediatric Surgery International, 27, 1091-1097.
http://dx.doi.org/10.1007/s00383-011-2959-4 - 8. Sabzehei, M.K., et al. (2011) Urogenital and Other Associated Anomalies in Patients with Anorectal Malformations. Nephro-Urology Monthly, 4, 388-390.
http://dx.doi.org/10.5812/numonthly.1678 - 9. Bãlãnescu, R.N., Topor, L. and Moga, A. (2013) Anomalies Associated with Anorectal Malformations. Chirurgia, 108, 38-42.
- 10. Kiely, E.M. and Peña, A. (1998) Anorectal Malformations. In: O’Neill, J.A., Rowe, M.I., Grosfeld, J.L., Fonkalsrud, E.W. and Coran, A.G., Eds., Pediatric Surgery, 5th Edition, St Louis, Mosby, 1425-1448.
- 11. Casaccia, G., Catalano, O.A. and Bagolan, P. (2009) Congenital Gastrointestinal Anomalies in Anorectal Malforma tions: What Relationship and Management? Congenital Anomalies, 49, 93-96.
http://dx.doi.org/10.1111/j.1741-4520.2009.00230.x - 12. Mittal, A., Airon, R.K., Magu, S., Rattan, K.N. and Ratan, S.K. (2004) Associated Anomalies with Anorectal Malformation (ARM). Indian Journal of Pediatrics, 71, 509-514.
- 13. http://dx.doi.org/10.1007/BF02724292
- 14. Albanese, C.T., Jennings, R.W. and Lopoo, J.B. (1999) One-Stage Correction of High Imperforate Anus in the Male Neonate. Journal of Pediatric Surgery, 34, 834-836.
http://dx.doi.org/10.1016/S0022-3468(99)90382-2 - 15. Devries, P.A. (2001) Posterior Sagittal Anorectoplasty. Journal of Pediatric Surgery, 17, 638-643.
- 16. Bischoff, A., Levitt, M.A. and Peña, A. (2009) Bowel Management for the Treatment of Pediatric Fecal Incontinence. Pediatric Surgery International, 25, 1027-1042.
http://dx.doi.org/10.1007/s00383-009-2502-z - 17. Har, A.F., Rescorla, F.J. and Croffie, J.M. (2013) Quality of Life in Pediatric Patients with Unremitting Constipation Pre and Post Malone Antegrade Continence Enema (MACE) Procedure. Journal of Pediatric Surgery, 48, 1733-1737.
http://dx.doi.org/10.1016/j.jpedsurg.2013.01.045 - 18. Brain, A.J. and Kiely, E.M. (2001) Posterior Sagittal Anorectoplasty for Reoperation in Children with Anorectal Malformations. British Journal of Surgery, 76, 57-59.
- 19. Hassink, E.A., Rieu, P.N., Hamel, B.C., Severijnen, R.S., vd Staak, F.H. and Festen, C. (1996) Additional Congenital Defects in Anorectal Malformations. European Journal of Pediatrics, 155, 477-482.
- 20. Cho, S., Moore, S.P. and Fangman, T. (2001) One Hundred Three Consecutive Patients with Anorectal Malformations and Their Associated Anomalies. Archives of Pediatrics and Adolescent Medicine, 155, 587-591.
http://dx.doi.org/10.1001/archpedi.155.5.587 - 21. Peña, A. (1995) Anorectal Malformations. Seminars in Pediatric Surgery, 4, 35-47.
- 22. Nah, S.A., Ong, C.C., Lakshmi, N.K., Yap, T.L., Jacobsen, A.S. and Low, Y. (2012) Anomalies Associated with Anorectal Malformations according to the Krickenbeck Anatomic Classification. Journal of Pediatric Surgery, 47, 2273-2278.
http://dx.doi.org/10.1016/j.jpedsurg.2012.09.017 - 23. Hamid, C.H., Holland, A.J. and Martin, H.C. (2007) Long-Term Outcome of Anorectal Malformations: The Patient Perspective. Pediatric Surgery International, 23, 97-102.
http://dx.doi.org/10.1007/s00383-006-1841-2 - 24. Stoll, C., Alembik, Y., Dott, B. and Roth, M.P. (2007) Associated Malformations in Patients with Anorectal Anomalies. European Journal of Medical Genetics, 50, 281-290.
http://dx.doi.org/10.1016/j.ejmg.2007.04.002 - 25. Rintala, R.J. (1996) Anorectal Malformations—Management and Outcome. Seminars in Fetal & Neonatal, 1, 219-230.
- 26. Peña, A. (2001) Posterior Sagittal Anorectoplasty as a Secondary Operation for the Treatment of Fecal Incontinence. Journal of Pediatric Surgery, 18, 762-773.
- 27. Dewan, P.A., Hrabovszky, Z. and Mathew, M. (2000) Redo Anorectoplasty in the Management of Anorectal Anomaly Patients. Australian and New Zealand Journal of Surgery, 70, A109.
- 28. Van den Hondel, D., Sloots, C., Meeussen, C. and Wijnen, R. (2014) To Split or Not to Split: Colostomy Complications for Anorectal Malformations or Hirschsprung Disease: A Single Center Experience and a Systematic Review of the Literature. European Journal of Pediatric Surgery, 24, 61-69.
http://dx.doi.org/10.1055/s-0033-1351663 - 29. Kumar, A., Argawala, S., Srinivas, M., Bajpai, M., Bhatnagar, V., Gupta, D.K., Gupta, A.K. and Mitra, D.K. (2005) Anorectal Malformations and Their Impact on Survival. Indian Journal of Pediatrics, 72, 1039-1042.
http://dx.doi.org/10.1007/BF02724407 - 30. Fabbro, M.A., Chiarenza, F., D’Agostino, S., Romanato, B., Scarpa, M., Fasoli, L., Iannucci, I., Pinna, V. and Musi, L. (2011) Anorectal Malformations (ARM): Quality of Life Assessed in the Functional, Urologic and Neurologic Short and Long Term Follow-Up. Pediatria Medica e Chirurgica, 33, 182-192.




