S. DHAPODKAR ET AL.
49
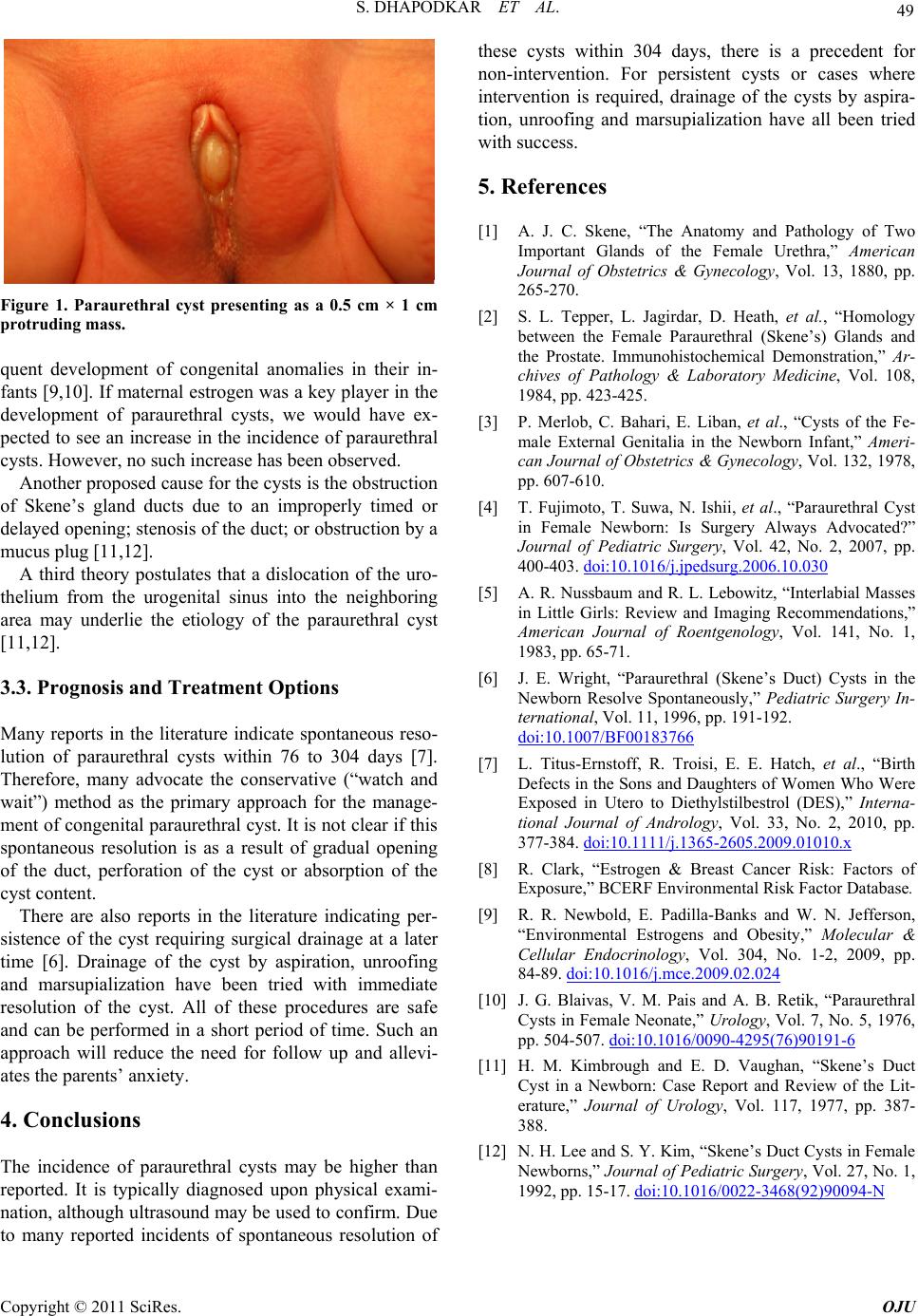
Figure 1. Paraurethral cyst presenting as a 0.5 cm × 1 cm
protruding mass.
quent development of congenital anomalies in their in-
fants [9,10]. If maternal estrogen was a key player in the
development of paraurethral cysts, we would have ex-
pected to see an increase in the incidence of paraurethral
cysts. However, no such increase has been observed.
Another proposed cause for the cysts is the obstruction
of Skene’s gland ducts due to an improperly timed or
delayed open ing; stenosis of the duct; or obstr uction b y a
mucus plug [11,12].
A third theory postulates that a dislocation of the uro-
thelium from the urogenital sinus into the neighboring
area may underlie the etiology of the paraurethral cyst
[11,12].
3.3. Prognosis and Treatment Options
Many reports in the literature indicate spontaneous reso-
lution of paraurethral cysts within 76 to 304 days [7].
Therefore, many advocate the conservative (“watch and
wait”) method as the primary approach for the manage-
ment of congenital p araurethral cyst. It is not clear if this
spontaneous resolution is as a result of gradual opening
of the duct, perforation of the cyst or absorption of the
cyst content.
There are also reports in the literature indicating per-
sistence of the cyst requiring surgical drainage at a later
time [6]. Drainage of the cyst by aspiration, unroofing
and marsupialization have been tried with immediate
resolution of the cyst. All of these procedures are safe
and can be performed in a short period of time. Such an
approach will reduce the need for follow up and allevi-
ates the parents’ anxiety.
4. Conclusions
The incidence of paraurethral cysts may be higher than
reported. It is typically diagnosed upon physical exami-
nation, although ultrasound may be used to confirm. Du e
to many reported incidents of spontaneous resolution of
these cysts within 304 days, there is a precedent for
non-intervention. For persistent cysts or cases where
intervention is required, drainage of the cysts by aspira-
tion, unroofing and marsupialization have all been tried
with success.
5. References
[1] A. J. C. Skene, “The Anatomy and Pathology of Two
Important Glands of the Female Urethra,” American
Journal of Obstetrics & Gynecology, Vol. 13, 1880, pp.
265-270.
[2] S. L. Tepper, L. Jagirdar, D. Heath, et al., “Homology
between the Female Paraurethral (Skene’s) Glands and
the Prostate. Immunohistochemical Demonstration,” Ar-
chives of Pathology & Laboratory Medicine, Vol. 108,
1984, pp. 423-425.
[3] P. Merlob, C. Bahari, E. Liban, et al., “Cysts of the Fe-
male External Genitalia in the Newborn Infant,” Ameri-
can Journal of Obstetrics & Gynecology, Vol. 132, 1978,
pp. 607-610.
[4] T. Fujimoto, T. Suwa, N. Ishii, et al., “Paraurethral Cyst
in Female Newborn: Is Surgery Always Advocated?”
Journal of Pediatric Surgery, Vol. 42, No. 2, 2007, pp.
400-403. doi:10.1016/j.jpedsurg.2006.10.030
[5] A. R. Nussbaum and R. L. Lebowitz, “Interlabial Masses
in Little Girls: Review and Imaging Recommendations,”
American Journal of Roentgenology, Vol. 141, No. 1,
1983, pp. 65-71.
[6] J. E. Wright, “Paraurethral (Skene’s Duct) Cysts in the
Newborn Resolve Spontaneously,” Pediatric Surgery In-
ternational, Vol. 11, 1996, pp. 191-192.
doi:10.1007/BF00183766
[7] L. Titus-Ernstoff, R. Troisi, E. E. Hatch, et al., “Birth
Defects in the Sons and Daughters of Women Who Were
Exposed in Utero to Diethylstilbestrol (DES),” Interna-
tional Journal of Andrology, Vol. 33, No. 2, 2010, pp.
377-384. doi:10.1111/j.1365-2605.2009.01010.x
[8] R. Clark, “Estrogen & Breast Cancer Risk: Factors of
Exposure,” BCERF Environmental Risk Factor Database.
[9] R. R. Newbold, E. Padilla-Banks and W. N. Jefferson,
“Environmental Estrogens and Obesity,” Molecular &
Cellular Endocrinology, Vol. 304, No. 1-2, 2009, pp.
84-89. doi:10.1016/j.mce.2009.02.024
[10] J. G. Blaivas, V. M. Pais and A. B. Retik, “Paraurethral
Cysts in Female Ne onate,” Urology, Vol. 7, No. 5, 1976,
pp. 504-507. doi:10.1016/0090-4295(76)90191-6
[11] H. M. Kimbrough and E. D. Vaughan, “Skene’s Duct
Cyst in a Newborn: Case Report and Review of the Lit-
erature,” Journal of Urology, Vol. 117, 1977, pp. 387-
388.
[12] N. H. Lee and S. Y. Kim, “Skene’s Duct Cysts in Female
Newborns,” Journal of Pediatric Surgery, Vol. 27, No. 1,
1992, pp. 15-17. doi:10.1016/0022-3468(92)90094-N
Copyright © 2011 SciRes. OJU