 Open Access Library Journal How to cite this paper: Hung, N.N., Tan, D. and Hien, N.D.N. (2014) Analysis of Two Different Techniques for Treatment of Patellar Dislocation Due to Fibrous Quadriceps Muscle in Children. Open Access Library Journal, 1: e1003. http://dx.doi.org/10.4236/oalib.1101003 Analysis of Two Different Techniques for Treatment of Patellar Dislocation Due to Fibrous Quadriceps Muscle in Children Nguyen Ngoc Hung1, Do Tan2, Nguyen Do Ngoc Hien2 1National Hospital for Pediatrics, Hanoi, Vietnam 2Hanoi Medical University, Hanoi, Vietnam Email: ngocyenhung@gmail.com, dotan20042005@yahoo.com, hienoph@yahoo.com Received 28 July 2014; revised 9 September 2014; accepted 12 October 2014 Copyright © 2014 by author and OALib. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Objective: To evaluate the clinical and functional results of two surgical treatments of patellar dislocation in children. Material and Methods: A prospective study was undertaken from January 1995 to December 2009. Pre-postoperatively, the clinical and roentgenographic examinations were performed. Patellar dislocation was classified according to Bensahel’s criteria. There were two surgical techniques performed: 1) the iliotibial tract passing through patella (ITT), and 2) transferring vastus medialis oblique muscle to superior border patella (VMO). Lateral retinacula were released to restore the tension of the medial retinacula and quadricepsplasty was used in all patients. The results of the operations were classified according to Kujala’s functional knee-s cor - ing systems. Results: 128 patients (132 knees) were operated. There were 20 males and 108 fe- males. 94 knees (71.2%) were Type 1, and 38 knees (28.8%) were Type 2. The ITT was in 74 pa- tients (76 knees), and VM was in 54 patients (56 knees). Clinical signs, imaging finding before and after the operation and operative results of these patients were operated with ITT and VM with no significant difference (p > 0.05). Overall, we attained excellent results in 95 knees (72.0%), good results in 30 knees (22.7%), and fair results in 7 knees (5.3%). There have been no poor results or recurrences so far. Conclusion: These techniques are simple, safe and effective in skeletally im- mature children. Long-term follow-up of these patients was operated ITT and these patien ts which were operated VMO were not different, but time for operation was: ITT: 65 minutes, and VMO: 55 minutes. Keywords Patella Instability, Habitual Dislocation of the Patella, Subluxation of the Patella, Developmental Dysplasia of Patella (DDP), Malformative Dislocation Subject Areas: Orthopedics, Pediatrics N. N. Hung et al. DOI:10.4236/oalib.1101003 2 October 2014 | Volume 1 | 1. Introduction Patellar dislocation is common in children, and many operations have been described for its treatment (Hauser [1]; Baker et al. [2]; Madigan, Wissinger and Donaldson [3]). Surgical treatments include both proximal and distal realignments of the extensor mechanism, and most involve considerable surgical trauma, a large scar and prolonged rehabilitation. However, there is no single procedure that is appropriate for all cases because of varia- tions am on g patient s [4]-[6]. Many factors contribute to patellar dislocation, including 1) congenital mechanisms (i.e., generalised liga- mentous laxity, dysplasia of the patella or the femoral condyles, genu valgum, tight lateral bands and patella alta [1]-[3]), and 2) a secondary mechanism, due to iatrogenic quadriceps fibrosis after intramuscular antibiotic(s) injections changed vector pull quadriceps, and fibrous vastus lateralis, vastus intermedius, and lateral retinacular patella; degeneration and contracture of rectus femoris and vastus medialis. This second etiology, patellar dislocation secondary to intramuscular injections, was the subject of our study. In 1961, Hnëvkovský [7] first stimulated an interest in this etiology by his report of progressive fibrosis of the vastus intermedius in young children who had received intramuscular antibiotic injections. Gunn 1964 [8] dem- onstrated a causal relationship between intramuscular injections and quadriceps contracture, which in turn led to the habitual dislocation of the patella. Although all the conditions we now associate with this contracture are well known, the importance of the underlying muscle condition in each case has not been stressed. Since 1995, our surgical team has treated dislocation of the patella in children by two procedures with 1) us- ing the iliotibia tract (ITT) past through pattela, and 2) transferring the vastus medialis oblique (VMO) to the superior border of the patella; those procedures have been combining capsulorraphy and quadricepsplasty. The purpose of this study was to evaluate and compare the long-term results of those procedures. 2. Material and Methods A prospective study was conducted; from January 1995 to August 2004, 74 patients (76 knees, two patients with bilateral dislocation), they have been operated according to ITT; and from September 2004 to December 2009, 54 patients (56 knees, two patients with bilateral dislocation), they have been operated according to VMO. For a total 128 patients with 132 knees (bilateral knee in 4 patients). Fifty-one right knees (39.8%) and seven- ty-three knees (57.1%) were affected; four patients (3.1%) had bilateral problems. 6 knees (4.6%) had persistent patellar dislocation, in which the patella rested laterally at all times, and the remaining 126 knees (95.4%) had recurrent patellar dislocation. There were twenty males (15.6%) and one hundred-eight females (84.4%) in this study. The mean age of the patients at surgery was 8 years - 4 months (range, 6 years - 4 months to 14 years - 5 months). With a documented past history of multiple intramuscular injections during the neonatal period and patellar dislocation due to fibrous quadriceps were recruited. The medical agents that had been injected were all antibio- tics: penicillin, gentamycine, linco mycin, streptomycin, clox acilin, etc. In these patients there was no history of trauma, or family history of patellar dislocation, genu valgum or other congenital diseases. All patients had had at least three complete lateral d islocations of the patella; the patella h ad been seen or felt to lie on the lateral as- pect of the femur. The cardinal physical sign was the lateral dislocatio n of the patella each time the knee flexed. With the patella held firmly in the femoral groove, we saw a limitation of knee flexion between 10˚ and 20˚ in 45 knees (34.1%), and of 30˚ in 81 knees (61.4%) and habitual in 6 knees (4.6%). When the patella had dislocated, full f lexion was possible. Palpable bands attaching to the lateral border of the patella were noted in all knees. There were 8 patients with opposite knee stiffness and 7 patients with other joint stiffness caused by post-injection of antibiotic(s) into fibrous muscles (elbow in three patients; abd uction of the scapula in three patients, and adduction contractur e of the shoulder in one patient). Exclusions: We excluded patients from the study who had undergone a previous operation for patellar insta- bility or an internal derangement; had suffered from major trauma to the knee; or had neuromuscular disease, Down syndrome, or other congenital conditions such as arthrogryposis multiplex congenita. Clinical and imaging examinations Patellar dislocation was determined based on clinical exam results and imagi n g findings a s des cribed below. Clinical examination: For a dislocation we wou ld expect to find the following clinical signs: 1) k nee defor- N. N. Hung et al. DOI:10.4236/oalib.1101003 3 October 2014 | Volume 1 | mation; 2) atrophy of the thigh compared to the opposite healthy thigh; 3) on knee flexion, a prominent lateral knee; the patellar medial glide test < 5 mm at 30 degrees of knee flexion [9]; and 4) the patient being unable to run. We also tested the following factor s : Q-angle [10], genu valgum, and the ligament laxity. Imaging findings Each patient had radiography according to Hugston [4], magnetic resonance imaging (MRI), computed tomo- graphy (CT) scan and ultrasound for the knee and thigh. Roentgenogram/X-ray Patella alta: Was diagnosed in the latera l view us ing the method of Isall and Salvati [11]. Lateral patellar t ilt: In the axial view, we measured the lateral patellofemoral angle according to Laurin et al. [12]. Abnormal tilt: The abnor mal tilt was als o calculated in the axial view according to Gre lsa mer et al. [13]. Magnetic resonance imaging (MRI) Shallow patellar gr o ove: The trochlear depth was assessed according to Seil et al. [14]. Computer tomography (CT scan) We used Dejour et al.’s classification of trochlear dysplasia in this study [15]: performing a CT scan of the distal femur sulcus lines were displayed in both the horizontal and sagittal planes. a) Normal trochlea: tip of lateral facet > sulcus line < tip of medial facet. b) Flat trochlea (crossing sign): tip of lateral facet = sulcus line = tip of medial facet. c) Lateral convexity (double contour): tip of lateral facet = sulcus line > tip of medial facet. Ultrasound We performed ultrasound of the muscles at distal thigh to evaluate the presence of fibrous muscles, which demonstrated fibrous muscles in the distal third of the thigh in all patients. Classification of patellar dislocation Our patients were classified accord ing to Bensahel et al.’s criteria [16]: Type 1: Dislocation of the patella without major radiographic abnormality. Type 2: Dislocation of the patella with major femoropatellar dysplasia, namely a patella alta and a flat or convex trochlea. Conservative treatment Conservative treatment was tried on patients (in the first 6 weeks the conservative treatment was performed with physiotherapy daily for 1 hour. The physiotherapist undertook a passive movement with flexion and exten- sion by holding the patella in the intercondylar groove and furthermore mobilized the knee in a superior-inferior and medial-lateral way). After physical therapy, the knee was placed in a plastic splint with knees flexed a maximum amount but without patellar dislocation. The knee flexion was gradually increased. Conservative treatment was considered to have failed if the patient had recurrent patellar dislocation when the knee was flexed; surgery was then indicated for these children. Any patients who had experienced recurrent pa- tellar dislocation, were indicated immediately for surgery witho ut conservative treatment. Surgical technique and procedure A single surgeon (the author) performed all of the patient operations. All pertinent clinical and operative records were prospectively reviewed. Patient positioning The patient was positioned supine on a standard operating table, placed under general anesthesia, with a sand bag behind the knee to keep it in between 5˚ and 10˚ of flexion; the anterolateral part of the thigh was exposed. We used the anterolateral approach that extended from the mid-third of the thigh to the tibial tuberosity, and a slightly curved lateral border of the patella (Figure 1). The subcutaneous tissues were undermined sufficiently to create a skin flap that would allow us to expose the quadriceps muscle, the medial and lateral retinaculum of the patella, the iliotibial tract, the patella, and the patellar tendon. This incision avoided penetration into the capsule and the infrapatellar nerve. The operation was performed in three procedural stages Procedure Stage 1—Releasing the lateral retinaculum and restoring the medial retinaculum The tight lateral bands were released from the patella and the incision continued proximally, lateral to the rectus femoris tendon, thus fully releas ing the vas tus late ralis and vastus medialis. A slightly curved longitudinal incision was made from the superolateral aspect of the patella proximally for 8 cm or more, as necessary. How-  N. N. Hung et al. DOI:10.4236/oalib.1101003 4 October 2014 | Volume 1 | Figure 1. Skin incision. ever, this procedure alone could not allow the stable reduction of the patella in the fully flexed knee. It was al- ways necessary to detach the insertion of the vastus lateralis fro m the patella, sep arating it fro m the rectus femo- ris medially and the iliotibial tract later a lly, then mobilizing it proximally (Figure 2). Releasing the lateral retinaculu m of the patella: we increased the tension of the medial retinaculum by divid- ing it into 2 parts, then used an imbricating stitch to link one part over the other, for 1.5 cm length, using No. 2 Ethibond sutures, while holding the patella in a normal position to attain 25% lateral translation with the knee flexed 60 de grees (Figure 3). Procedure Stage 2—Lengthening the rectus femoris and vastus intermedius We separated the adherence between the vastus imtermedius tendon and the rectus femoris tendon. Next we divided the vastus intermedius tendon at the musculo-tendinous junction, 5 cm above the patella. We performed knee flexion, if knee flexion of >90˚ was achieved, the vastus intermedius tendon (5 cm above the patella) was removed (Figure 4(a)), and the remaining vastus intermedius was sutured to the rectus femoris with knee flex- ion of 60˚ (Figure 4(b)). If knee flexion of >90˚ was not achieved, the rectus femoris was detached two centi- meters above the superior border of the patella, two tendons, the vastus intermedius and rectus femoris, being sewn together with using No. 2 Ethibond sutures while the knee flexed at 60˚ (Figure 5). Finally, the remaining vastus intermedius muscle was sutured to the rectus femoris. Procedure Stage 3 Transfering iliotibial tract past through patella (ITT) or the transfer of the vastus medialis oblique (VMO) to the superi or border of the patella. Transfering iliotibial tract past through patella (76 patients had been operated from January, 1994 to Au- gust, 200 4) The releasing the iliotibial tract 3 inchs above the superolateral border of the patella (Figure 6(a)), suturing the remaining proximal end to the fascial thigh, and creating a tunnel between the front face of the patella and the patellar aponeurosis from the superolateral border to the inferomedial border (Figure 6(b)). The iliotibial tract was passed through the tunnel, while the patella was translated medially and distally. The iliotibial tract was sutured to the patella, and the free end of the iliotib ial tract was su tured to the insertion of the semitendinosus muscle with the knee fexed 60 ˚, using No. 3 Ethibond sutures as shown in Figure 7. The transfer of the vastus medialis oblique (VMO) to the superior border of the patella (56 patients had been operated from Sept ember, 200 4 to December, 2010) We transferred and sutured the inferolateral corner VMO to the superolateral pole of the patella, and then transferred and sutured the inferomedial corner VMO to the superomedial pole of the patella, using No. 2 Ethibond with the knee flexed at 60˚. The vastus lateralis was su tured to the latera l side of the rectu s femoris (Figure 8(a)) or to the joint tendon (the rectus femoris and the vastus intermedius) (Figure 8( b)). The patella was then moved medially to check whether the release had been adequate (to ensure this, we checked that the patella was tracking normally and riding smoothly within the intracondylar groove; and that there was no tilting of the pa- tella, nor excessive tension at the suture line). The knee was f lexed and ex tend ed sev eral ti mes to see if the p a- tella was tracking normally in its groove. At this stage we expected that the patella should ride smoothly within  N. N. Hung et al. DOI:10.4236/oalib.1101003 5 October 2014 | Volume 1 | Figure 2. Detaching the insertion of the vastus lateralis and vastus medialis from the patella. Figure 3. Releasing the lateral retinaculum and restoring the medial retinaculum. (a) (b) Figure 4. (a) Separating two tendons of the vastus intermedius and rectus femoris tendon: (1) positional tenotomy at the musculo-tendinous junction 5 cm above the patella; (b) If knee flexion of >90˚ was achieved, tenotomy and removing the segmental tend on of the vastus intermedius.  N. N. Hung et al. DOI:10.4236/oalib.1101003 6 October 2014 | Volume 1 | (a) (b) Figure 5. (a) (1) Positional tenotomy at the musculo-tendinous junction of the vastus intermedius 5 cm above the patella. (2) If knee flexion of >90˚ was not achieved, tenotomy of the rectus femoris 2 cm above the patella; (b) Two tendons, the vastus intermedius and rectus femoris, being sewn together with knee flexion at 60˚. (a) (b) Figure 6. (a) Free tenotomy to create about 3 inchs iliotibial tract; (b) Created tunnel is between front of face of patella and patellar aponeurosis. Figure 7. This image belong to left knee during operation. Transfering Iliotibia l tract past through a tunnel between the front face of the patella and the patellar aponeurosis from the superolateral border to the inferomedial border. The iliotibial tract is sutured to the patella and the free end is sutured to the semitendinousus muscle insertion.  N. N. Hung et al. DOI:10.4236/oalib.1101003 7 October 2014 | Volume 1 | (a) (b) Figure 8. (a) If knee flexion of >90˚ was achieved, tenotomy and removing the segmental tendon of the vastus intermedius, the VMO transferred to the superior border of the patella and the vastus lateralis sutured to the lateral side of the rectus femoris; (b) If knee flexion of >90˚ was not achieved, tenotomy of the rectus femoris 2 cm above the patella, and the vastus intermedius and rectus femoris, being sewn together with knee flexion at 60˚. The VMO transferred to the superior border of the patella and the joint tendons. the intracondylar groove and there should be no tilting of the patella or excessive tension at the suture line. It was also important to b e certain that th e lateral bo rder of the pate lla was in lin e with the later al border of the lat- eral femoral condyle. Upon completion of the release, complete hemostasis was achieved by the coagulation of all sources of bleeding, especially the lateral superior geniculate artery at the superolateral border of the patella. The skin was closed without leaving drainage; the lower extremity was placed in a cast with the knee flexed at 60˚ (Figure 9). Intraoperative biopsy Biopsy specimens were taken of the muscular vastus lateralis, medialis, intermedius, rectus fermoris, fascia lata, and lateral, and medial retinaculum of the patella to find any potential tissue abnormalities such as fibrosis or degeneration of the muscles or fibrous band. Postoperative rehabilitation Postoperatively, the knee was placed in a double capsule cast with the knee flexed at 60˚. This was a long leg cast (Figure 9). The cast could be removed easily for knee mobilization physical therapy and then be replaced afterward. The patient was allowed out of bed one day after the operation. Static quadriceps exercises and gentle knee movements (passive range of motion not greater than 60˚ equal knee flexed at 60˚ and VMO was trans- ferred and sutured to patella) were permitted, but more vigorous or extensive movements were discouraged dur- ing the first week, in order to minim ize effusi on or bleeding. In the first two weeks, a passive range of motion up to 60˚ and under 90˚ was performed with the physiotherapist. After two weeks, the range of motion was in- creased up to 90˚ (note: the limitations on range of motion and weight-bearing counted only for the exercise pe- riods, and outside of the exercise times, the cast had to be worn). After three weeks, the range of motion was in- creased to normal. The cast was removed after about six weeks, but without weight-bearing. Afterwards, pa- tients were allowed to bear 25% of their body weight for the first two weeks, and 50% of their body weight the following two weeks. Full weight-bearing was allowed between the fourth and sixth week after cast removal. Follow-up All patients were examined and evaluated at follow -up times of 3 weeks, 6 weeks, 3 months, 6 months, 1 year, and afterwards every year. At latest follow-up, after an average period of 6 years, 7 months (range 2 years, 7 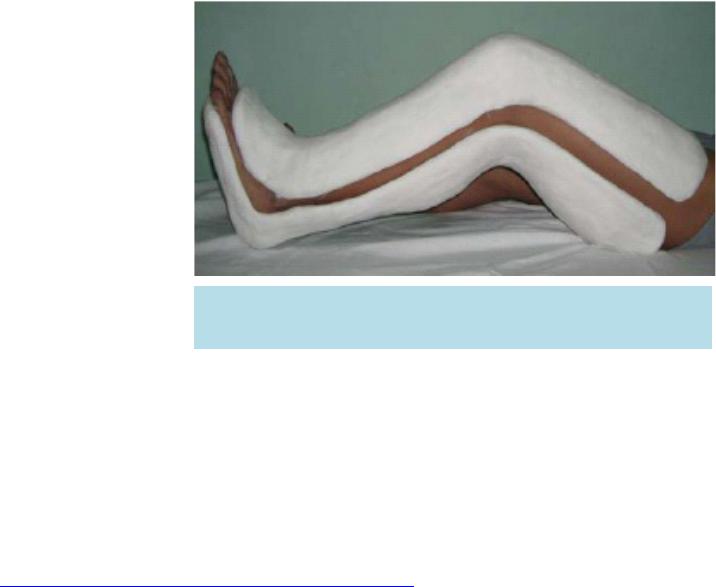 N. N. Hung et al. DOI:10.4236/oalib.1101003 8 October 2014 | Volume 1 | Figure 9. The double capsule cast—a long leg cast placed from above the knee down to the toes. The cast could easily remove at physiothe- rapy for knee mobilization and has to replace afterward. months to 9 years, 6 months), the average patient age was 12 years, 5 months (range, 9 years, 6 months to 18 years, 7 months). We classified the results of the operation according to Kumar et al. [17] with objective evaluation undertaken using Fulkerson et al. [10] and Kujala et al. [18] functional knee-scoring systems. The scores were graded as follows: excellent: 90 - 100 points; good: 80 - 89 points; fair: 70 - 79 points; poor: <70 points. Statistical analysis The data were analysed with Epi Info 6.04 sofware public domain statistical software for epidemiology, de- veloped by Centers for Disease Contro l and Prevention (CDC) in Atlanta, Georgia, USA, http://wwwn.cdc.gov /e piinfo/html/prevVersion.htm. We performed the χ2 test for percentage and the t-student test for mean comparison. P-values ≤ 0.05 were regarded as statistically significant. All reading s were provided as average values together with the appropriate standard deviation. Author is surgeon operated all patients i n this study 3. Result Classification of patellar dislocation Among our patient co hort, 94 knees (71. 2% ) we r e Type 1, a nd 38 k ne e s (2 8.8%) were Type 2. After the surgery we saw remarkable improvement in clinical and roentgenographic findings in our patient cohort. Clinical signs before and after the operation of these patients were operated ITT and VMO were not different with p > 0.05. The patients were operated ITT, average preoperative Q-angle was 15.5˚ (rang e, 12.0˚ to 22.0˚). There were 7 knees with a Q-angle greater than 20˚. Postoperatively, the average Q-angle was 8.8˚ (range, 5˚ to 14˚) which was sign ifica ntly ( p = 0.000695). The patients were operated VMO, average preoperative Q-angle w as 14 .8˚ (range, 13 .6˚ to 21.7˚). There were 5 knees with a Q-angle greater than 20˚. Postoperatively, the average Q-angle was 8.2˚ (range, 6˚ to 113.1˚) which was significantly (p = 0.000695). All patients had thigh atrophy preoperatively, which was related to the condition of fibrous muscle. There were 52 knees with corresponding atrophic thighs of 1.5 cm, and remaining 88 knees had a thigh atrophy of 1.5 cm to 2.5 cm. Preoperatively, limited medial translation of the patella had been the result of slackness or contracture of the lateral patellar retinacu la . After th e interv ention, the patella with medial glide test >5 mm at 30 ˚ of knee flexion. Imaging finding before and after the operation of these patients were operated ITT and these patient were op- erated VMO were not different with p > 0.05. The patients were operated ITT; preoperative, patella alta was apparent in 15 knees (19.7%), and postopera- tively it was only seen in 3 knees (3.9%); preoperatively, lateral patellar tilt was found in 54 knees (71.1%), and postoperatively in only 3 knees (3.9%); preoperatively, there were shallow patellar grooves in 20 (26.3) knees, of which 16 (21.1%) knees had flattening of the distal lateral femoral condyle, and postop eratively, only 2 knees N. N. Hung et al. DOI:10.4236/oalib.1101003 9 October 2014 | Volume 1 | (2.6%) showed shallow patellar groove and 4 (5.3%) knees showed flattening of the distal lateral femoral con- dyle. The patients were operated VMO; preoperatively, patella alta was apparent in 12 knees (21.2%), and post- operatively it was only seen in 3 knees (5.4%) ; preop eratively, la teral p atellar tilt was f ound in 34 knees (6 0.7%), and postoperatively in only 2 knees (3.6%); preoperatively, there were shallow patellar grooves in 18 (28.6%) knees, of which 11 (19.6%) knees had flattening of the distal lateral femoral condyle, and postoperatively, only 2 knees (3.6%) showed shallow patellar groove and 3 (5.4%) knees showed flattening of the distal lateral femor- al condyle. Pathological findings Intraoperatively, the vastus lateralis muscles were markedly fibrosed, contractured and shortened in all pa- tients. This generally comprised a dense, fibrous, band running along the muscle’s lower border. An abnormal attachment of the iliotibial tract to the patella was seen in all knees (100%), with the iliotibial tract attached to the distal vastus lateralis muscle and the superolateral patella. This tract had a rolled anterior border and swept forward to the patella rather than having its main attachment be to the tibia; the lateral patella retinaculum was thick and fibrous. The insertion of the vastus lateralis into the upper pole of the patella was seen clearly, and fibrous tissue developed around its lateral aspect, distinct from the rest of the fascia lata. The iliotibial tract was attached to the muscular vastus lateralis at a location about 2.5 cm to 5 cm above the superiolateral patella by fibrous tissues. Contractures were present in the rectus femoris in 80 knees (60.6%), and in the vastus interme- dius in 51 knees (38.6%). The VMO was degenerated and straightened in 102 knees (77.3%) and that affected its medial pulling function. We performed a muscular biopsy intraoperatively, which showed marked fibrosis of the muscular lateral vas- tus, intermedius vastus, and the lateral retinacular patella. The degeneration of the medial vastus and rectus fe- moris was also noted. All of these signs were also seen in the fibrosis of the quadriceps, triceps, gluteal, and deltoid muscles secondary to the antibiotic intramuscular injections. The quadriceps muscle was usually short- ened due to a severe degree of fibrosis. Postoperatively, all patients had the patella aligned with the patellar groove of the femur when flexing and extending. Knee function returned to normal in 115 knees (87.1%). There 11 knees (8.3%) with limitation of flexion to 60˚ - 90˚ in 8 knees (6.1%), and >90˚ in 3 knees (2.3%). There 6 knees (4.6%) with loss of extension, extension lag < 10˚ in 4 knees (3.0%), and 10˚ - 20˚ in 2 knees (1.5%), and no cases with extension lag more than 20˚. Extension lag happened only when both the vastus intermedius and the rectus femoris were severely damaged. Comparative complications limitation of flexion/extension were not different (p valuate: 0.937604, and 0.726761). Time for operation ITT: 65 minutes, and VMO: 55 minutes Mean of Kujala score: 97.4 points in ITT and 91.2 points in VMO (p valuate = 0.80444 4) Long-term follow-up of th ese patients were operated ITT and these patient were operated VMO were not dif- ferent. Latest follow-up, patien t’s age > 9 - ≤ 11 years old in 39 (29.6%), >11 - ≤14 years old in 86 (65.1%), and >14 years old in 7 (5.3%). All patients according to age of group and latest results were not di f fe rent. Latest follow-up, these patients were operated ITT and VMO according to age of group were not different (p valuate > 0.05). According to age under and over 14, excellent & good result in this study was better than Baker technique [2] with p valuate = 0.0085. At latest follow-up, after an average period of 6 years, 7 months (range 2 years, 7 months to 9 years, 6 months). T he avera ge pa t i e nt age was 1 2 ye ars, 5 mont hs (range , 9 ye a rs, 6 months to 18 years, 7 months). Overall, long-term follow -up showed excell ent: 95 (72. 0%), good: 30 (22.7%), fair: 7 (5.3%), and poor results in no knees. There was no redislocation or subluxation in any of the knees. The mean Kujala score was 58.3 points (range, 33 - 65) preoperatively, and 94.3 points (range, 76 - 100) at latest follow-up. An ugly scar was noted in thirteen knees (9.9%). Complications were as follows: Infections: none; Skin necrosis: none; Osteochondral patellar fracture: none; Redislocation or subluxation: none; Limitative knee movement: 17 knees.  N. N. Hung et al. DOI:10.4236/oalib.1101003 10 October 2014 | Volume 1 | 4. Discussion Williams reported 2 6 patients with stiffness of th e knee and 13 of them with dislocation of the patella [19], Al- varez [20], Dennis [21], Mukherjee [22], and Sharrard [23] reported stiffness of the knee with dislocation of the patella. Those patients developed dislocation of the pa tella after repeated antibio tic intramuscular injection s into the quadriceps muscle. Our study found a history of repeated antibiotic intramuscular injections into the quadri- ceps muscle in all patients, which caused thigh atrophy. The patella was held in the intercondylar groove so that the knee could not flex beyond 30˚. All parts of the quadriceps except the vastus medialis were involved, and there was also an abnormal attachment of the iliotibial tract. The quadriceps muscle was usually shortened and contractrue. Furthermore, this fibrosis also diffused into the lateral retinacular patella, which was shown by the patellar medial glide tes t to be 5 mm at 3 0˚ of knee flexion (see Table 1). Fibrous tissue of the lateral vastus in ultrasound. Fibrous tissue of the lateral vastus, intermedius vastus, and lateral retinaculum were shown even more clearly in muscular biopsy. Variations among patients with patellar instability suggest that one specific procedure may not be an appro- priate procedure for all patients with patellar dislocation [24]. The number of different techniques for patellar realignment and stabilization reported in the literature is astonishing. In 1959 Cotta [25] counted 137 surgical methods directed at solving the problems of an unstable patella. These procedures can be classified into soft- tissue balancing procedures and bony transfer procedures. In a skeletal immature patient with open growth plates, transfer of the tibial tubercle must be avoided if possible to prevent premature physeal closure and sub- sequent development of genu recurvatum. In children, soft-tissue balancing procedures are widely accepted me- thods of treatment, such as the surgical procedure which involves a lateral retinacular release w ith mobilization of the vastus medialis muscle to a more distal and lateral position on the extensor mechanism. The quadriceps muscle was weak and often shortened. As a result, realigning the vectors of action of the quadriceps muscle was the most important element in establishing normal patellofemoral joint function. However, when only the qua- driceps mechanism was corrected the recurrence rate was high. Many studies have published data relating to re- current dislocation rates of between 4% and 44% [26] [27]. Poor results have been reported, especially when lateral release is used as a solo procedure [10] [28]. Galeazzi [29], Baker [2] used semitendinosus tenodesis passed through the patella for repair of recurrent dislocation of the patella in children. However, this technique has some complications, such as fracture or degeneration and hypermobility of the patella, and patella alta is not fully corrected [30]. Surgical technique The iliotibial tract passed through patella The iliotibial tract is normally inserted into a facet on the lateral condyle of the tibia. Through this insertion the gluteus maximus and the tensor fasciae latae stabilize the slightly flexed knee during weight-bearing. How- ever, the iliotibial tract is merely a thickened strip of the fascia lata. T his fascia gives origin to the intermuscula r septa of the quadriceps group of muscles, and on either side of the patella is reinforced by fibers which blend with the aponeuroses of the vastus lateralis and the vastus medialis. These fibers are stronger on the lateral side, where they arise from the iliotibial tract. The iliotib ial tract lies in front of the axis of rotation of the knee joint, and passes behind that axis as the knee bends. It follows that if the patella is tethered to the tract in any way, it must be pulled laterally during flexion of the knee. The iliotibial tract is attached to the distal vastus lateralis muscle. If the vastus lateralis muscle is shortened the lateral dislocation of the patella is created when the knee flexes. The tendon of the vastus lateralis and the iliotibial tract have to be divided so that the patella can remain Table 1. Clinical signs before and after the operation. Pre-Operation Post-Operation ITT (%) VMO (%) p valuate ITT (%) VMO (%) p valuate Thigh atrophy 100 100 13.2 14.3 0.85196 The patellar medial glide test < 5 mm at 30 degrees of knee flexion 100 100 0 0 Q-Angle in degrees 15.5˚ (12˚ - 22˚) 14.8˚ (13.6˚ - 21.7˚) 0.8648 8.8˚ (5˚ - 14˚) 8.2˚ (6˚ - 13.1˚) 0.78966 Mean Kujala score 58.3 46.5 0.37977 97.4 91.2 0.80444 N. N. Hung et al. DOI:10.4236/oalib.1101003 11 October 2014 | Volume 1 | in the intercondylar groove when the knee is fully flexed. However, no one ever thought of using a divided ili- otibial tract to keep the patella in place. We used the iliotibial tract for dislo cation of the patella. We passed the iliotibial tract th rough a tunnel which was created between the front face of the patella and the patellar aponeurosis (see Figure 7 ), w ithout d rilling th e patella, so there was no fracture of the patella. The iliotibial tract created a force to stabilize the patella, medially aligning the quadriceps patellar tibial mechanism, and providing a balancing medial vector and distal realign- ment of the extensor mechanism. We modified Ober technique [31] did not create groove in medial proximal ti- bia, could be injury of physis in skeletally immature children. Our surgical technique meets all of the demands of Hinton [32] and Sta nitski [33]: 1) releasing an abnormal tethering vector, 2) balancing the medial vector, and 3) aligni ng the quadr i c e ps pa tella r-tibial mechanism. Transfering vastus medialis oblique muscle to superior border patella Vastus medialis oblique transplantation, distally and laterally to the front of the patella, was suggested by Madigan, Wissinger and Donaldson in 1975 [3]. All authors agreed that in children with immature bones, the intervention should be only done on the soft tissues. In 1975, Madigan et al. [3] (followed by other authors sub- sequently) transferre d the VMO laterally and distally and sutured it directly to the anterior side of the patella or to the medial rectus femoris tendon, as p er West [34], hoping to stabilize the patella and direct force on the pa- tella medially, thereby hoping to pr event lateral displacement. The vastus medialis muscle can be functionally divided into long and oblique components. Lieb and Perry [35] reported that in the larger and proximal long component, the fibers have a more vertical orientation, deviating medially 15 to 18 degrees from the longitudinal axis of the femur, while the fibers in the distal quarter of the muscle, the oblique component, deviate 50 to 55 degrees from the femoral axis. Furthermore, the vector of pull of the oblique component is similar to that of the long component. The only unique function of the vastus medialis oblique is to ex ert a medially directed force to the superior bord er of the patella and thereby prevent lateral displac ement. The impression is supported by the findings of Lieb and Perry [35]. Clinical realities showed an excellent and good rate of 94.7%, without poor results or redislocations, prov- ing the preeminence of this technique. In our study, the VM commonly was severely atrophic and more vertically oriented rather than oblique, as reported by Andrish [36]. To complete our first goal, which was to restore the original direction force of the VMO, we released it from the medial intermuscular septum and transferred it to the superior border of the patel- la. Unlike Madigan’s technique, in which they transferred the insertion of the vastus medialis laterally and dis- tally to overly the p atella, in our patients the VM was tight and shortened, so it could not be transfe rred distally and laterally to the front of the patella. Moreover, VMO had been transferred to the superior border of the patella so deviating angle from the femoral axis more than Madigan’s technique. In these cases, if the VMO were su- tured to the front of the patella, it would slip sutures if knee flexion or postoperative badly limit the knee flexion. Our second goal was to restore the normal alignment and function of the extensor mechanism. We released the insertion of the vastus lateralis and to the patella, so that the lateral forces on the patella were reduced. The vastus intermedius and rectus femoris also limited the movement of the knee. We lengthened the vastus inter- medius and rectus femoris with the goal of improving flexion and extension of the knees. Fibrous quadriceps muscle, special fibrous vastus lateralis and vastus intermedius could affect distal femoral nutrient artery and metabolism local distal femur. Further, mechanical damage due to the frequent patellar dis- location had created bone change around distal femur. Compare two techniq ues i n this stud y an d other techni ques If compare Madigan’s result [3] were fifty-eight percent had good or excellent and 42 percent had poor results after a mean follow-up of twenty-nine months; our result were ninety-four percent had good or excellent and without poor results or recurrent dislocation of the patella; our result were better than Madigan’s result with p valuate 0.000001. If comparision two surgical technique for dislocation of the patella in this study shown pre and post opera- tively had clinical and images signs were similar (p valuate > 0.05) (see Table 1, Table 2); and postoperative result were similar (p valuate > 0.05) (see Table 3); postoperative complication were similar too. However, we shown time for VM (mean 55 minute) shorter ITT (mean 65 minute). Compare ITT and VMO according to two age under and over 14 in this study, postoperative result were simi- lar (p valuate > 0.05) (see Table 4 ). If compare excellent and good result of Baker technique [2] and two t ech- niques in this study shown our technique were better than Baker technique (p valuate > 0.0085) (see Table 5).  N. N. Hung et al. DOI:10.4236/oalib.1101003 12 October 2014 | Volume 1 | Table 2. Imaging findings. Pre-Operation Post-Operation ITT (%) VMO (%) p valuate ITT (%) VMO (%) p valuate Patella alta 19.7 21.4 0.81176 3.9 5.4 0.96934 Lateral patellar tilt 71.1 60.7 0.21302 3.9 3.6 0.72676 Shallow patellar groove 26.3 28.6 0.80909 2.6 3.6 0.83963 Flattening of the distal lateral femoral condyles 21.1 19.6 0.81284 5.3 5.4 0.71203 Table 3. Long-term follow-up. ITT (%) VMO (%) p valuate Excellent 73.7 69.7 0.60940 Good 22.4 23.2 0.90875 Fair 3.9 7.1 0.67685 Poor 0 0 0 Table 4. Latest follow-up and age of group. Age Excellent Good Fair Total ITT VMO p ITT VMO p ITT VMO p >9 - ≤11 14 (25.0%) 17 (43.6%) 0.0572 2 (11.8%) 3 (23.1%) 0.7417 2 (66.7%) 3 (75.0%) 41 (31.1%) >11 - ≤14 39 (69.6%) 21 (53.8%) 0.1163 13 (76.4%) 9 (69.2%) 0.9778 1 (33.3%) 1 (25.0%) 84 (63.6%) >14 3 (5.4%) 1 (2.6%) 0.8826 2 (11.8%) 1 (7.7%) 0.8059 0 0 7 (5.3%) 56 (73.7%) 39 (69.7%) 0.6719 17 (22.4%) 13 (23.2%) 0.6843 3 (3.9%) 4 (7.1%) 132 p: p valuate. Table 5. Compare operative result according to age under and over 14 (Baker and Hung*). Under 14 Over 14 Baker [2] Hung* Pva. Baker [2] Hung* Pval. Excellent & Good 29 (79%) 118 (94.4%) 0.0085 14 (88%) 7 (100%) Fair 5 (13%) 7 (5.6%) 0.2086 0 0 Poor 1 (3%) 0 2 (12%) 0 Recurrence 2 (5%) 0 0 0 37 125 16 7 Pva: p valuate; Hung*: Hung in this study Bensahel et al. [16] performing operation for unstable patella in children with postoperative good result in 85%. Several studies have yielded favorable outcomes with the use of the semitendinosus tenodesis for disloca- tion of the patella [37]. Baker et al. [2] published a series of 53 knees and demonstrated that this technique yielded good to excellent results in the majority of both younger and older children and 79% and 89% good to excellent results in younger and older children, respectively. Recurrence rates were <5%. Hall et al. [38] de- scribed a series of 26 knees with >60% good to excellent results. However, Hall et al. [38] also performed a  N. N. Hung et al. DOI:10.4236/oalib.1101003 13 October 2014 | Volume 1 | Roux-Goldthwait procedure on 19 of the knees in his study that makes his data more difficult to interpret. More recently, Letts et al. [38] presented a series of 26 knees with 82% good to excellent results with a recurrence rate of 8%. This study is similar to the results previously reported by Baker et al. [2]. Limitations and complications Loss of extension 6 knees (4.6%) had extension lag 10˚ - 20˚. This result was due to the postoperative quadriceps weakness. Although that complication rate was low, and happened in severely damaged quadriceps, we still suggest that quadriceps lengthening should only be considered when the vastus intermedius release alone cannot attain the knee flexion of more than 90˚. Limitation of flexion There 11 knees (8.3%) had limitation of flexion. All knees had severely fibrous vastus intermedius, and de- generation of the rectus femoris in pathological examination. In our opinion, this may be due to 2 causes, either 1) incomplete liberation of the surrounding fibrosis, or 2) inadequate lengthening of the quadriceps. Therefore, we suggest that before finalizing the operation, performing knee flexion. If knee flexion of >90˚ was not achieved, the quadriceps should be further lengthened. However, we hope that during our children’s growth and development, their kne e functi on can recover. 5. Conclusions In children, an unstable patella with stiffness of the knee may occur after repeated antibiotic intramuscu lar injec- tions, which causes fibrosis in the quadriceps. The bone malnutrition and effective metabolism due to fibrosis and frequent patellar dislocation in turn cause the anatomical lesions such as patellar tilt, patellar alta, shallow patellar groove and flattening of the distal lateral femoral condyles. In surgery for dislo cation of the patella, it is difficult to ob tain a normal position of the patella in ch ildren us- ing soft-tissue balancing procedures alone. In our cases of pediatric dislocation of the patella caused by iatro- genic quadriceps fibrosis, by two surgical techniques with using iliotibial tract passing through patella and transfer of the vastus medialis to the superior border of the patella and combining capsulorraphy, quadri- cepsplasty showed high success in restoring the realignment mechanism of the patella. Long-term follow-up of these patients was operated ITT and these patients which were operated VMO were not different, but time for operation was: I TT: 65 minutes, and VMO: 55 minutes. Those techniques a re simple, safe and effective in ske- letally immature children. References [1] Hauser, E.D.W. (1938) Total Tendon Transplant for Slipping Patella: A New Operation for Recurrent Dislocation of the Patella. Surgery, Gynecology & Obstetrics, 66, 199-214. [2] Baker, R.H., et al. (1972) Semitendinosus Tenodesis for Recurrent Dislocation of the Patella. Journal of Bone and Joint Surgery, 54-B, 103-109. [3] Madigan, R., et al. (1975) Preliminary Experience with a Method of Quadricepsplasty in Recurrent Subluxation of the Patella. Journal of Bone and Joint Surgery, 57-A, 600-607. [4] Hughston, J.C. (1968) Subluxation of the Patella (Instructional Course Lectures of the American Academy of Ortho- paedic Surgeons). Journal of Bone and Joint Surgery, 50-A, 1003-1026. [5] Letts, R.M., et al. (1999) Semitendinosus Tenodesis for Repair of Recurrent Dislocation of the Patella in Children. Journal of Pediatric Orthopaedics, 19, 742-774. http://dx.doi.org/10.1097/01241398-199911000-00010 [6] Merchant, A.C. (1988) Classification of Patellofemoral D isorders. Arthroscopy, 4, 235-240. http://dx.doi.org/10.1016/S0749-8063(88)80037-9 [7] Hnëvkovský (1961) Progressive Fibrosis of the Vastus lntermedius Muscle in Children. Journal of Bone and Joint Surgery, 43-B, 318. [8] Gunn, D.R. (1964) Contracture of the Quadriceps Muscle. Journal of Bone and Joint Surgery, 46-B, 492-497. [9] Insall, J.N., et al. (1976) Chondromalacia Patellae: A Prospective Study. Journal of Bone and Joint Surgery, 58-A, 1-9. [10] Fulkerson, J.P., et al. (1990) Anteromedial Tibial Tuberele Transfer without Bone Graft. The American Journal of Sports Medicine, 5, 490-497. http://dx.doi.org/10.1177/036354659001800508 [11] Insall, J. and Salvati, E. (1971) Patella Position in the Normal Knee Joint. Radiology, 101, 101-104. http://dx.doi.org/10.1148/101.1.101  N. N. Hung et al. DOI:10.4236/oalib.1101003 14 October 2014 | Volume 1 | [12] Laurin, C.A., Lévesque, H.P., Dussault, R., Labelle, H. and Peides, J.P. (1978) The Abnormal Lateral Patellofemoral Angle. A Diagnostic Roentgenographic Sign of Recurrent Patellar Subluxation. Journal of Bone and Joint Surgery, 60, 55-60. [13] Grelsamer, R.P., Bazos, A.N. and Proctor, C.S. (1993) Radiographic Analysis of Patella Tilt. Journal of Bone and Joint Surgery, 73, 822-824. [14] Seil, R., Müller, B., Georg, T., Kohn, D. a nd Rupp, S. (2000) Reliability and Interobserver Variability in Radiological Patellar Height Ratios. Knee Surgery, Sports Traumatology, Arthroscopy, 8, 231-236. http://dx.doi.org/10.1007/s001670000121 [15] Dejour, H., Walch, G., Ney ret, P. and Adeleine, P. (1990) Dysplasia of the Femoral Trochlea. Revue de chirurgie or- thopedique et reparatrice de l’appareil moteur, 76, 45-54. [16] Bensahel, H., Souchet, P., Pennecot, G. F. and Mazda, K. (2000) The Unstable Patella in Children. Journal of Pediatric Orthopaedics, 9, 265-270. http://dx.doi.org/10.1097/01202412-200010000-00010 [17] Kumar, A., Jones, S., Bickerstaff, D.R. and Smith, T.W.D. (2001) Functional Evaluation of the Modified Elmslie- Trillat Procedure for Patello-Femoral Dysfunction. The Knee, 8, 287-292. http://dx.doi.org/10.1016/S0968-0160(01)00105-3 [18] Kujala, U.M., Jaakkola, L.H., Koskinen, S.K., Taimel a, S., Hurme, M. and Nelimarkka, O. (1993) Scoring of Patello- femoral Disorders. Arthroscopy, 9, 159-163. http://dx.doi.org/10.1016/S0749-8063(05)80366-4 [19] Williams, P.F. (1968) Quadriceps Contracture. Journal of Bone and Joint Surgery, 50, 278-284. [20] Alvarez, E.V., Munters, M., Lav ine, L.S., Manes, H. and Waxman, J. (1980) Quadriceps Myofibrosis. A Complication of Intramuscular Injections. Journal of Bone and Joint Surgery, American Volume , 62, 58-60. [21] Dennis, R.W. and Mercer, R. (1993) Knee Pain in Children and Adolescents. In: Dennis, R.W. and Mercer, R., Eds., The Art and Practice of Children’s Orthopaedics, Raven, New York, 220-255. [22] Mukherjee, P.K. and Das, A.K. (1980) Injection Fibrosis in the Quadriceps Femoris Muscle in Children. Journal of Bone and Joint Surgery, American Volume, 62, 453-456. [23] Sharrard, W.J.W. (1979) Developmental Contracture of the Quadripceps. In: Sharrard, W.J.W., Ed., Paediatric Ortho- paedics and Fracture, Blackwell, Oxford, 877-880. [24] Ghanem, I., Wattincourt, L. and Seringe, R. (2000) Congenital Dislocation of the Patella. Part I: Pathologic Anatomy. Journal of Pediatric Orthopaedics, 20, 812-816. http://dx.doi.org/10.1097/01241398-200011000-00023 [25] Cotta, H. (1959) Zur Therapie der habituellen Patellarluxation. Archiv für orthopädische und Unfall-Chirurgie, mit besonderer Berücksichtigung der Frakturenlehre und der orthopädisch-chirurgischen Technik, 51, 256-271. http://dx.doi.org/10.1007/BF00415542 [26] Drez, D., Edwards, T.B. and Williams, C.S. (2001) Results of Medial Patellofemoral Ligament Reconstruction in the Treatment of Patellar Dislocation. Arthroscopy, 17, 298-306. http://dx.doi.org/10.1053/jars.2001.21490 [27] Abraham, E., Washington, E. a nd Huang, T.L. (1989) Insall Proximal Realignment for Disorders of the Patella. Clini- cal Orthopaedics and Related Research, 248, 61-65. [28] Fulkerson, J.P. (1983) Anteromedialization of the Tibial Tuberosity for Patellofemoral Malalignment. Clinical Ortho- paedics and Related Research, 177, 176-181. [29] Galeazzi, R. (1922) Nuove applicazioni del trapianto muscolare e tendineo. Arch Di Ortop Milano, 38, 315-323. [30] Deie, M., Ochi, M., Sumen, Y., Yasumoto, M., Kobayashi, K. and Kimura, H. (2003) Reconstruction of the Medial Patellofemoral Ligament for the Treatment of Habitual or Recurrent Dislocation of the Patella in Children. Journal of Bone and Joint Surgery, British Volume, 85, 887-890. [31] Ober, F.R. (1935) Slipping Patella or Recurrent Dislocation of the Patella. Journal of Bone and Joint Surgery, 17, 774- 779. [32] Hinton, R.Y. and Sharma, K.M. (2003) Acute and Recurrent Patellar Instability in the Young Athlete. Orthopedic Clinics of North America, 34, 385-396. http://dx.doi.org/10.1016/S0030-5898(03)00033-6 [33] Stanitski, C.L. (1995) Management of Patellar Instability. Journal of Pediatric Orthopaedics, 15, 279-280. http://dx.doi.org/10.1097/01241398-199505000-00001 [34] West, F.E. and Soto-Hall, R. (1958) Recurrent Dislocation of the Patella in Adult, End Result of Patellectomy with Quadricepsplasty. Journal of Bone and Joint Surgery, 40-A, 386-394. [35] Lieb, F.J. and Perry, J. (1968) Quadriceps Function: An Anatomical and Mechanical Study Using Amputated Limbs. Journal of Bone and Joint Surgery, American Volume, 50, 1535-1548. [36] Andrish, J. (2008) The Management of Recurrent Patellar Dislocation. Orthopedic Clinics of North America, 39, 313- 327. N. N. Hung et al. DOI:10.4236/oalib.1101003 15 October 2014 | Volume 1 | [37] Moyad, T.F. and Blakemore, L. (2006) Modified Galeazzi Technique for Recurrent Patellar Dislocation in Children. Orthopedics, 29, 302-304. [38] Hall, J.E., Micheli, L.J. and McManama Jr., G.B. (1979) Semitendinosus Tenodesis for Recurrent Subluxation or Dis- location of the Patella. Clinical Orthopaedics and Related Research, 144, 31-35.
|