Clinical Feature of Japanese Patients with Fulminant Myocarditis
262
the mechanical support in order to resume a normal life.
Thus, several specialists, such as cardiologists, anesthe-
siologists, respiratory doctors, infection control teams,
mechanical support technicians, and skilful nurses, were
essential to care patients with fulminant myocarditis in
intensive care unit.
The treatment of myocarditis is controversial, and no
specific therapeutic regimen has been established [11].
All patients with myocarditis should receive standard
heart failure therapy. Immunosuppressive therapy has
been proposed to treat myocarditis in both children and
adults. The results of an international trail, the Myocardi-
tis Treatment Trial in 1995, showed that there was no
difference in heart function in the treated with immuno-
suppressive agents or placebo [12]. Despite the negative
results of this trail, the authors indicated that patients
who responded to immunosuppressive therapy appeared
to have higher initial ejection fraction and shorter dura-
tion of illness. High-dose intravenous immune globulin
(IVIG) has both immune modulatory and antiviral effects
[13-15]. However, there was no difference between pla-
cebo and IVIG. Thus, there was no benefit of immuno-
modulation. In the present study, some patients had im-
munosuppressive therapy, some had IVIG and some had
both. The present small study cannot conclude the effects
of the immunosuppressive and the immunomodulation
therapy for fulminant myocarditis. Taken as a whole, the
present small study together with previous trials, do not
support the routine use of immunosuppressive and im-
munomodulation therapy for fulminant myocarditis [16].
These data suggest that subgroup with ongoing fulminant
myocarditis, especially in the patients who need me-
chanical cardiac support, can be more likely to benefit
from immunosuppressive and immunomodulation ther-
apy, although no uniform methodology yet exists to
identify them.
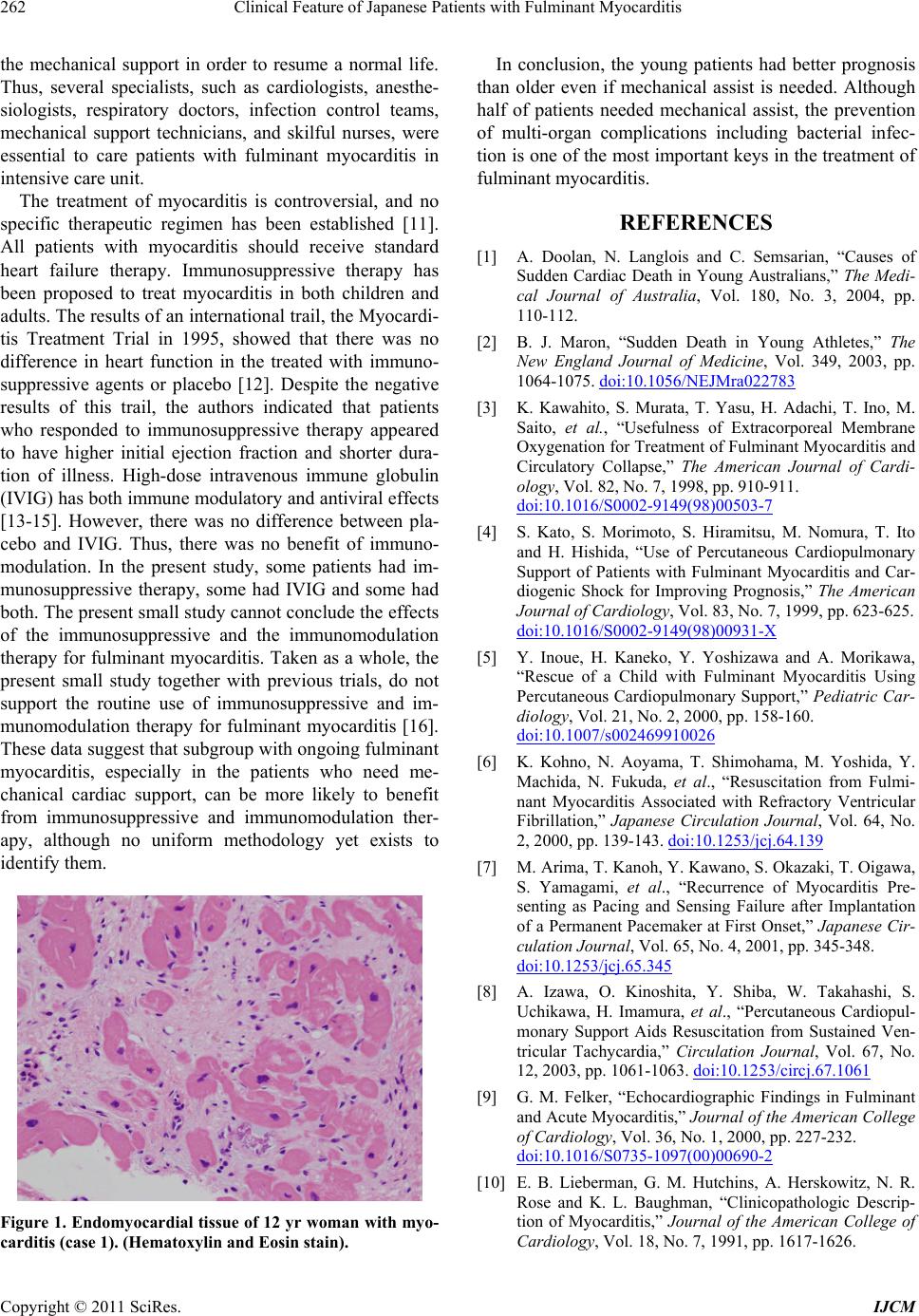
Figure 1. Endomyocardial tissue of 12 yr woman with myo-
carditis (case 1). (Hematoxylin and Eosin stain).
In conclusion, the young patients had better prognosis
than older even if mechanical assist is needed. Although
half of patients needed mechanical assist, the prevention
of multi-organ complications including bacterial infec-
tion is one of the most important keys in the treatment of
fulminant myocarditis.
REFERENCES
[1] A. Doolan, N. Langlois and C. Semsarian, “Causes of
Sudden Cardiac Death in Young Australians,” The Medi-
cal Journal of Australia, Vol. 180, No. 3, 2004, pp.
110-112.
[2] B. J. Maron, “Sudden Death in Young Athletes,” The
New England Journal of Medicine, Vol. 349, 2003, pp.
1064-1075. doi:10.1056/NEJMra022783
[3] K. Kawahito, S. Murata, T. Yasu, H. Adachi, T. Ino, M.
Saito, et al., “Usefulness of Extracorporeal Membrane
Oxygenation for Treatment of Fulminant Myocarditis and
Circulatory Collapse,” The American Journal of Cardi-
ology, Vol. 82, No. 7, 1998, pp. 910-911.
doi:10.1016/S0002-9149(98)00503-7
[4] S. Kato, S. Morimoto, S. Hiramitsu, M. Nomura, T. Ito
and H. Hishida, “Use of Percutaneous Cardiopulmonary
Support of Patients with Fulminant Myocarditis and Car-
diogenic Shock for Improving Prognosis,” The American
Journal of Cardiology, Vol. 83, No. 7, 1999, pp. 623-625.
doi:10.1016/S0002-9149(98)00931-X
[5] Y. Inoue, H. Kaneko, Y. Yoshizawa and A. Morikawa,
“Rescue of a Child with Fulminant Myocarditis Using
Percutaneous Cardiopulmonary Support,” Pediatric Car-
diology, Vol. 21, No. 2, 2000, pp. 158-160.
doi:10.1007/s002469910026
[6] K. Kohno, N. Aoyama, T. Shimohama, M. Yoshida, Y.
Machida, N. Fukuda, et al., “Resuscitation from Fulmi-
nant Myocarditis Associated with Refractory Ventricular
Fibrillation,” Japanese Circulation Journal, Vol. 64, No.
2, 2000, pp. 139-143. doi:10.1253/jcj.64.139
[7] M. Arima, T. Kanoh, Y. Kawano, S. Okazaki, T. Oigawa,
S. Yamagami, et al., “Recurrence of Myocarditis Pre-
senting as Pacing and Sensing Failure after Implantation
of a Permanent Pacemaker at First Onset,” Japanese Cir-
culation Journal, Vol. 65, No. 4, 2001, pp. 345-348.
doi:10.1253/jcj.65.345
[8] A. Izawa, O. Kinoshita, Y. Shiba, W. Takahashi, S.
Uchikawa, H. Imamura, et al., “Percutaneous Cardiopul-
monary Support Aids Resuscitation from Sustained Ven-
tricular Tachycardia,” Circulation Journal, Vol. 67, No.
12, 2003, pp. 1061-1063. doi:10.1253/circj.67.1061
[9] G. M. Felker, “Echocardiographic Findings in Fulminant
and Acute Myocarditis,” Journal of the American College
of Cardiology, Vol. 36, No. 1, 2000, pp. 227-232.
doi:10.1016/S0735-1097(00)00690-2
[10] E. B. Lieberman, G. M. Hutchins, A. Herskowitz, N. R.
Rose and K. L. Baughman, “Clinicopathologic Descrip-
tion of Myocarditis,” Journal of the American College of
Cardiology, Vol. 18, No. 7, 1991, pp. 1617-1626.
Copyright © 2011 SciRes. IJCM