Safety and Efficacy of Pediatric General Anesthesia by Laryngeal Mask Airway Without Intravenous Access 329
0.001) for ENT procedures and when using the size 1
LMA.
There has been only one report in the literature (Hau-
pert et al. 2004) that addresses the issue of whether an
IV is even required for pediatric general anesthesia
where access is technically challenging due to anatomi-
cal considerations and a lack of patient cooperation. This
randomized controlled study had 100 ASA statuses I or
II children aged 2-12 who underwent bilateral myringo-
tomies with pressure equalizing tube placement [4]. One
group received IV access and the other did not. Both
groups had mask induction and maintenance with oxy-
gen, nitrous oxide, and Sevoflurane. All children re-
ceived Fentanyl intramuscularly and spontaneous venti-
lation was maintained. Patients with IV access received
Lactated Ringer’s solution. Their study concluded that
intravenous access in otherwise healthy children in my-
ringotomy procedures provided no added benefit [4].
Significant differences included more pain medication
required (p < 0.001), lower parental satisfaction (p <
0.001) and more time spent in both the operating room
(p = 0.02) and recovery (p = 0.02) for the group of chil-
dren with IV access [4].
The purpose of this study was to determine if general
anesthesia by laryngeal mask airway without intrave-
nous access is safe and efficacious, resulting in highly
successful placement rates, shorter procedure times and
a low rate of anesthetic complications in a pediatric
population. Our study would be the first to highlight the
benefits of using general anesthesia by LMA without IV
access for short pediatric procedures in the head and
neck region such as bilateral myringotomies and tube
placement (BMT), ophthalmologic exams under anes-
thesia (EUA), nasolacrimal duct probing and chalazion
excision.
2. Methods
After receiving institutional review board approval, the
surgery schedule at the University of Illinois Medical
Center Surgicenter was used to select patients aged 0-17
who underwent GA by LMA between the dates of Sep-
tember 1, 2003 to August 30, 2005. A retrospective chart
review was performed and the following documents
were gathered for each potential subject: anesthesia re-
cords, operative reports, and if applicable, Surgicenter
reports, hospital admission notes and recovery room
notes. Subjects having complete records were then cho-
sen for inclusion. Subjects lacking the appropriate docu-
mentation were excluded from the study. Eligible pa-
tients were then assigned into 2 groups, based on
whether they had an IV placed after mask induction with
Sevoflurane. Group 1 had no IV access, and group 2 had
IV access. The following data was then collected and
compared between the two groups:
Age, gender, weight, medical conditions and ASA
class
Procedure done and operating room (OR) time to
incision
LMA type used and whether successfully placed
Type of anesthetic used, method of ventilation
Type and location of intravenous placed if any
Medications given pre-, peri- and post-operatively
and route of administration
Anesthesia complications and management
Statistical analysis was performed using the software
program SigmaStat for Windows. Z-tests were utilized
for analysis of both LMA placement success rates and
complication rates between the groups 1 and 2. T-tests
were utilized for analysis of time to incision between the
groups. Statistically significant differences were consid-
ered achieved at p < 0.05.
3. Results
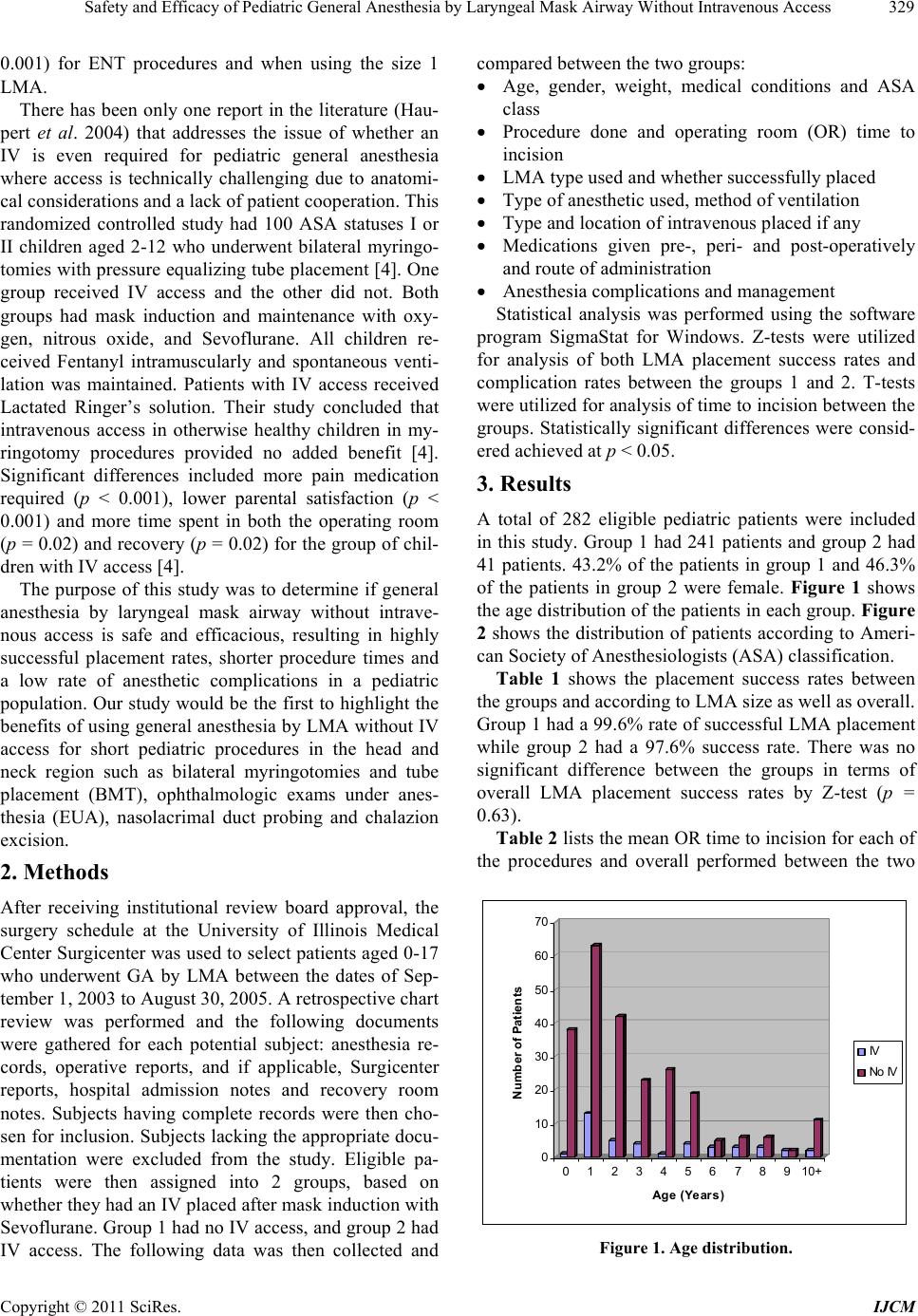
A total of 282 eligible pediatric patients were included
in this study. Group 1 had 241 patients and group 2 had
41 patients. 43.2% of the patients in group 1 and 46.3%
of the patients in group 2 were female. Figure 1 shows
the age distribution of the patients in each group. Figure
2 shows the distribution of patients according to Ameri-
can Society of Anesthesiologists (ASA) classification.
Table 1 shows the placement success rates between
the groups and according to LMA size as well as overall.
Group 1 had a 99.6% rate of successful LMA placement
while group 2 had a 97.6% success rate. There was no
significant difference between the groups in terms of
overall LMA placement success rates by Z-test (p =
0.63).
Table 2 lists the mean OR time to incision for each of
the procedures and overall performed between the two
0
10
20
30
40
50
60
70
Number of Patients
012345678910+
Age (Years)
IV
No IV
Figure 1. Age distribution.
Copyright © 2011 SciRes. IJCM