Health
Vol.5 No.3A(2013), Article ID:29559,19 pages DOI:10.4236/health.2013.53A073
Mental health in a Canadian Old Order Mennonite community
![]()
1School of Geography and Earth Sciences, McMaster University, Hamilton, Canada; *Corresponding Author: fisheka@mcmaster.ca
2School of Public Health and Health Systems, University of Waterloo, Waterloo, Canada
Received 14 December 2012; revised 14 January 2013; accepted 5 February 2013
Keywords: Social Determinants of Health; Rural Mental Health; Short-Form Health Survey (SF-12)
ABSTRACT
This paper presents the results of a 2010 survey exploring the determinants of rural mental health in two farming groups in Waterloo, Ontario, Canada: Old Order Mennonites (OOMs) and nonOOM farmers. Comparing these two groups reduces the likely impact of many contextual features impacting both groups, such as local economic conditions. We explore a comprehensive list of health determinants to assess their relative importance and thus enable policy action to focus on those having the greatest impact. The mental component summary (MCS) of the shortform health survey (SF-12) was used to measure mental health. We compare mental health in the two populations and use multiple regression to determine the relative importance of the determinants in explaining mental health. The results show that OOMs experience better mental health than non-OOMs, in part due to the strong mental health of OOM women. Coping, stress and social interaction shape mental health in both groups, reflecting the broader determinants literature and suggesting these are important across many populations with different life circumstances. Other determinants are important for one group but not the other, underscoring the diversity of rural populations. For example, different social capital measures shape mental health in the two groups, and sense-of-place is associated with mental health in only one group (OOMs). The results are discussed in terms of their implications for future health determinants research and policy action to address rural mental health.
1. INTRODUCTION
This paper is a study of the social determinants of health (SDOH) in rural populations. It tries to fill a gap in SDOH studies in a methodologically-rigorous way while engaging theoretical discussion and policy practice. Considerable research has been undertaken exploring the influence of the social and physical environments on health. These characteristics, or health determinants, have been prominent in Canadian policy discourse since the 1970’s. The Public Health Agency of Canada (PHAC) currently recognizes 12 such determinants: 1) Income and Social Status, 2) Social Support Networks, 3) Education and Literacy, 4) Employment/Working Conditions, 5) Social Environments, 6) Physical Environments, 7) Personal Health Practices and Coping Skills, 8) Healthy Child Development, 9) Biology and Genetic Endowment, 10) Health Services, 11) Gender, and 12) Culture [1]. Little attention has been paid to rural as opposed to general populations.
There are strong parallels with Canada’s list of heath determinants across developed nations. The WHO’s Commission on Social Determinants of Health (CSDH) recognizes a similar list, contextualized within a framework indicating interactions within and across determinants (Figure 1). As such, intermediary determinants directly influence health, but are in turn shaped by broader structural factors representing socio-economic and political contexts [2].
It remains unclear whether there are unique determinants underpinning rural health or whether a generic, more broadly-applicable set of determinants are distributed differently in rural settings [3]. This uncertainty reflects the lack of rural health research, but may also result from the standard approach of comparing rural and urban populations where the many social/physical environmental differences make it difficult to pinpoint the most influential health determinants. Significant sociodemographic diversity and health status variation exists even within rural settings, suggesting that it is important to restrict the geographical unit so that internal diversity is unmasked and results can be translated into action [3]. An action lens has been present in health determinants
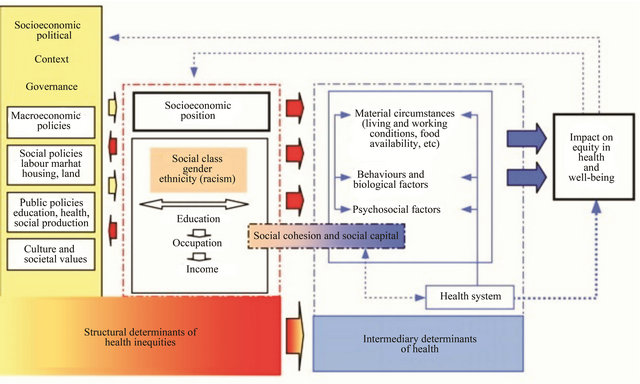
Figure 1. World Health Organization Commission on the Social Determinants of Health-Conceptual Framework for Social Determinants of Health (permission to reproduce received from WHO)
discussions, with research aimed at practical, economically-efficient solutions remaining a priority. As such, information on the relative importance of the determinants can be beneficial. However, most determinants research focuses on a subset of determinants, thus their relative importance is largely unknown [4].
This study addresses these research problems by comparing physical health status and its determinants in two farming populations that live in the same location. This approach reduces the number of factors responsible for health differences by eliminating many shared contextual determinants common to both groups. By focusing on two rural populations, this study may also offer unique insights into the health determinants of rural communities. A comprehensive list of determinants is included in the analysis, so that their relative importance can be assessed and policy actions can be designed that focus on those having the greatest health impact.
An additional feature of this study is its focus on a unique rural population—the Old Order Mennonites (OOMs) of Waterloo, Ontario (Canada). OOMs are farmers and key features of their lifestyle include no smoking, low/no alcohol consumption, high religiosity (Christian), strong family and community support, high levels of social interaction, and minimal reliance on technology [5]. Moreover, the OOMs lifestyle has remained relatively stable and culturally isolated for generations.
Studying isolated populations like OOMs is advantageous because distinct lifestyle practices may expose health benefits or risks (determinants) less easily identified in larger populations [6,7]. We hypothesize better mental health in OOMs compared to non-OOM farmers because of the health benefits of aspects of their lifestyle such as high levels of religiosity, social capital, social support and sense of community.
2. BACKGROUND
Poor mental health has been associated with a number of individual-level characteristics, including low socioeconomic status [8-10], low levels of job control [11], being female [12-14], being overweight [15], inferior coping skills and weaker social support [16], and higher stress levels [17]. There is no consistent evidence that contextual (area/population-level) characteristics significantly influence mental health once individual-level factors are accounted for. For example, area-level socioeconomic deprivation independent of individual factors has been linked to anxiety, depression and psychiatric hospital admissions [18-20]. But, other studies find that individual-level attributes such as age, gender and income represent the chief mental health determinants [21- 25].
Recent evidence links mental health to individuals’
perceptions about where they live, including sense of community belonging/cohesion and neighbourhood likes/ dislikes [4,22,23,26]. Sense of community belonging is a central measure used in sense-of-place research, with other core elements including rootedness, place identity, and the physical environment [27]. Researchers have further linked rootedness and place identity with the coherent integration of life experiences, enabling a smooth life-course transition and reinforcing individual/group continuity [28,29]. Most sense-of-place research focuses on physical health, with inconsistent evidence linking the two [27]. However, differences in methods, context and construct definitions have hampered study comparisons, as has the overall lack of theoretical development in placebased research [27,29]. Recent research suggests that sense-of-place may be more important in rural populations or in shaping mental health [23,30].
Social capital studies have also explored the health effects of the social environment. Social capital is broadly defined as social networks and norms of reciprocity, and its most common indicators are social participation, trust and reciprocity [31,32]. Distinguishing between different types of social capital, such as bonding ties with family/ friends versus bridging ties with more distant contacts [31], is important because the embedded social relations may have different meanings and health outcomes [33, 34]. Social capital studies generally focus on single social capital indicators and on physical or mental health [35]. Regarding mental health, there is evidence that individual-level social capital is associated with better mental health (after adjusting for socio-demographic factors), but area-level social capital effects appear weak [34,36,37]. Most studies showing a strong mental health association have explored bonding social capital, with trust being particularly influential [32,33,35,37,38].
Many studies have examined the religion-health linkage, which is particularly relevant to our study population. Regarding the SDOH, religiosity is closely aligned with the cultural determinant, although it overlaps with many others (e.g., social support, coping). Most studies focus on Jewish and Christian faiths [39], with mixed results regarding the mental health influence [40,41]. Literature reviews cite various limitations including difficulties in measuring religiosity, small “convenience” samples, treating correlation as causation and inappropriate control groups [42]. Spirituality, as opposed to religiosity, is also increasingly recognized as important in health research [43]. Evidence suggests that spirituality is more difficult to measure because it is comparatively abstract, internal and less associated with nonsacred elements such as social support [44]. This means research examining spirituality should employ measures other than church attendance and explore whether highly spiritual people (who may infrequently attend church) experience health benefits. A recent study examining the spirituality-health link found a positive association between psychological distress and feeling that spiritual values play an important role in life [45].
The OOMs are a closed community with little to no in-migration, increasing the likelihood of population bottlenecks combined with genetic drift, inbreeding, and thus genetic diseases [46]. Genetic studies of the OOM Waterloo lineage have identified a number of physical health disorders. These are relatively rare due to surpriseingly high genetic diversity [46]. Furthermore, [47] found a broad-based discouragement of close marriages and no evidence of higher rates of mental illness in Waterloo OOMs compared to the general population. The work by reference [47], while dated and lacking statisticcal validity, is nonetheless consistent with broader genetic research on OOM mental health. Studies examining the health-lifestyle linkage have found that Waterloo OOM and OOA (Old Order Amish) children demonstrate higher physical fitness levels compared to non-OOM/ OOA urban and rural children [48-50]. Most other (nongenetic) health information comes from U.S. studies of the OOA and indicate differences largely in favour of Old Orders for: death rate and life span [51], women’s mental and reproductive health [52], risk of cardiovascular disease [53], certain cancers [54-56] and Type 2 diabetes [57].
Rural health studies within developed countries offer additional insights on rural mental health. Most compare urban and rural populations, and reviews generally conclude that there is little evidence linking mental health differences with “rurality”, instead seeing it as a proxy for geographically dispersed determinants including job hazards, personal behaviour and socio-economic factors [3,58]. Reference [24] found no difference in urban-rural mental health using the SF-12 instrument employed in our study. References [30,59] found lower rates of depression among rural residents, with the former attributeing this to restricted service access and the latter to a stronger sense of community. Reference [23], in a recent study focused solely on rural populations, found sense of community to be important in shaping mental health. Other studies find more favourable health in rural populations, but most address physical health [60].
Caution is required in extending rural research results to our two populations. OOMs and non-OOMs live in the same region but occupy very different social environments. OOM scholars [47,61] suggest that a Gemeinschaft culture characterizes OOM social relations, with Gemeinschaft referring to a rural society rooted in the family farm and featuring shared values and norms, deeply-embedded ties, face-to-face relations, and mutual support [62]. Gesellschaft refers to the opposite society, one marked by self-interest, independence and the absence of shared values or norms. There is evidence of a more Gesellschaft culture in the non-OOMs, including the “factory farm” trends seen in adjacent farming communities [62-65] and survey differences such as the lower levels of social interaction, sense-of-place and perceived social support in non-OOMs (see Results below). Many Gemeinschaft characteristics are linked to mental health benefits, which we explore in the analysis below.
3. METHODS
3.1. Research Setting, Design
Both groups involved in the study reside in the Wellesley, Woolwich and Wilmot Townships of Waterloo, Ontario (Figure 2). Waterloo Region ranks second in Ontario in agricultural production [66], and the majority of the members in both groups are farmers. The two groups are compared with respect to mental health status, and the SDOH for each group are compared in an effort to explain health differences. Since both groups are mainly farmers living in the same location, determinants such as occupation and physical environment are unlikely to explain health difference.
A cross-sectional survey captured data for our study on mental health status and the SDOH. Early in the study design the challenges of accessing the closed OOM community had to be addressed. Consequently, the paper’s first author spent 1½ years regularly visiting the area, conducting participant observation, and meeting with OOMs or people knowledgeable about them. This started to build trust within the community and acceptance of the project’s utility.
OOM study participants were recruited through the churches. The senior OOM Bishop prepared a support letter to accompany the survey package, and arranged for the deacons to hand deliver the survey packages to all adults after the spring 2010 church services. Anonymity was assured by providing OOMs with a self-addressed, postage-paid envelope for mailing back the completed
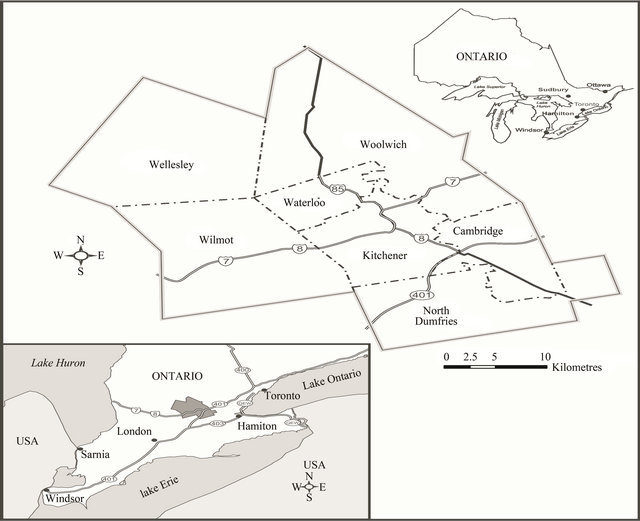
Figure 2. Study Location-Waterloo Region, Ontario, Canada.
survey. 1200 OOM surveys (60% response) were received, and 1171 were sufficiently completed for use in the analyses. The OOM sample was reduced to 850 in the following analyses, by eliminating those under the minimum age (28) of the non-OOMs. This was done in an effort to age-standardize the two groups.
Municipal tax rolls were used to identify non-OOM farmers. Directories of Mennonite and Amish groups were used to eliminate members of these groups from tax roll farmers, to avoid control group contamination. The survey package was mailed to all remaining tax roll farmers, with approximately 800 non-Mennonite (or non-Amish) households receiving the mailed survey. 344 completed surveys were received (43% response) from non-OOMs.
The survey distributed to both groups consisted of identical questions. It was piloted with a small number of OOM church leaders and community members, with feedback being incorporated into the final version. Study approval was received from the authors’ Ethics Review Board in February, 2010.
3.2. Mental Health Measure
We selected the mental component summary (MCS) score of the SF-12 health survey to measure mental health status because of its brevity, well-established psychometric properties [67] and demonstrated validity [68]. Generic measures like MCS are preferred to disease-specific measures, especially in exploring mental health in general populations [24]. The SF-12 consists of 12 questions measuring five mental health functional domains: general health perceptions (GH), energy and vitality (VT), social functioning (SF), role limitations due to emotional problems (RE) and mental health (MH) [67]. An algorithm scores the functional domains, standardizing them to a mean of 50 and standard deviation of 10. Higher MCS scores indicate better mental health status.
The SF-12 has been shown to be reliable in measuring health in the U.S., Australian, Israeli, Greek and Iranian populations, and many clinical groups [69,70]. Reliability and validity tests have been designed for the SF-36 [70] and adapted to the SF-12 [e.g., 72,73]. We conducted the SF-12 tests on both groups, with principal components analysis confirming the two-factor concepttual structure, and known group tests confirming expected relationships between demographic and healthrelated variables [74].
3.3. Determinants of Health Measures
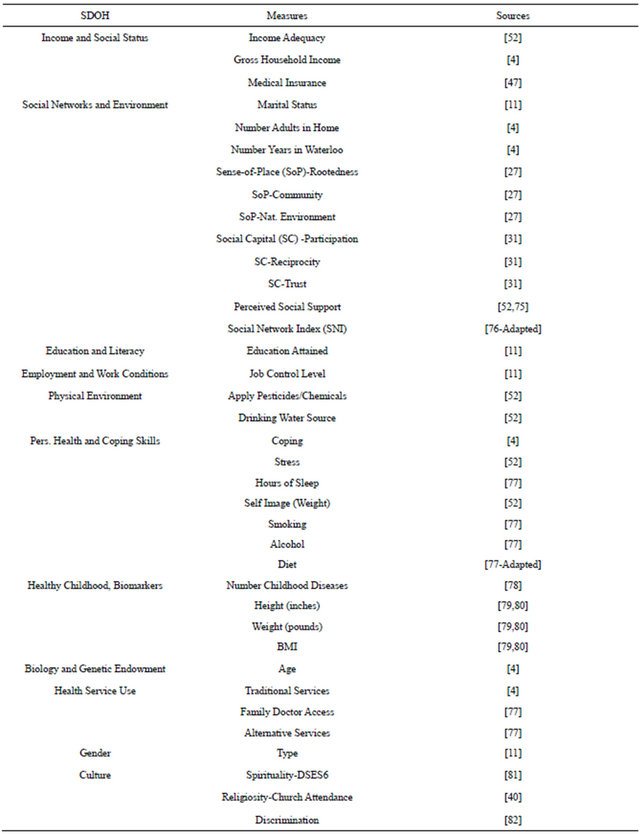
There are practical restrictions on how we can portray each determinant. Multiple measures were included in the survey for many SDOH because of their multidimensional nature and to provide alternative measures if significant non-responses were encountered. All SDOH were defined at the individual level. A variety of sources were consulted to guide the selection of measures, choice of wording, and response options (Table 1).
Some SDOH measures are scores created by adding up responses from one or more survey questions, with responses re-coded (if required) so higher scores represent higher levels of the underlying construct. For example, the three sense-of-place measures were re-coded so higher response codes represent higher sense-of-place levels (e.g., rootedness re-coded so 1 = not at all rooted… 5 = very rooted). For trust, the trust level selected for each of the 5 types of people were re-coded so higher scores represent higher trust (e.g., 4 = trust completely… 1 = do not trust at all) and a trust score was created by summing the re-coded responses for the 5 types of people. The perceived social support score was created by summing the tasks for which the respondent indicated that support existed most or all of the time. The participation score represents the sum of all organizations for which the respondent indicated “active” membership. The social network index (SNI) is the sum of the respondent’s number of close friends and relatives, with a number added for frequency of contact (1 if contact with friends/relatives was “rarely”, 2 for “once a week”, 3 for “daily”, 4 for “many times a day”). Reciprocity was split into help received and help given, with the score for each representing the sum of the tasks for which help was given or received. The 6-Item Daily Spirituality Experience Scale (DSES6) was created using the developer’s methodology [81], but no re-coding was employed to ensure comparability with the broader literature where higher DSES6 scores represent lower spirituality levels.
3.4. Statistical Analyses
SAS Version 9.2 was used for all statistical analyses. SF-12 MCS scores were calculated using the developer’s original (orthogonal) scoring algorithm [83], employing norms derived from U.S. population survey data [67,70]. References [84,85] confirm the validity of US-based norms in scoring Canadian applications of the SF-36 (hence SF-12). We compared the two groups with respect to the MCS and SDOH measures. Multivariate analyses (OLS) were conducted for both groups, with MCS as the dependent variable and the SDOH measures as independents. We restricted all regressions to working with the same set of SDOH measures to ensure comparability between the two groups (rather than maximizing explanatory power using a stepwise procedure to select the variables forming the optimal model). In this way, we could determine the degree to which SDOH measures
Table 1. SDOH measures and sources.
were significant in shaping mental health, given the presence of the same co-measures. All respondents in both groups answered at least 10 of the 12 SF-12 questions, and the proportion of missing data for the remaining survey questions was typically low (below 2%). Median values were substituted for missing values.
4. RESULTS
4.1. Distribution of Health Determinants
Compared to non-OOMs, the full OOM sample (n = 1171) is younger (mean age 43.4 versus 57.7) and has more females (58% versus 51%) and singles (33% versus 5%). Sample differences reflect differences in the recruitment efforts for the two groups. For example, church recruitment for the OOMs captured many singles living on their parent’s farm whereas municipal tax rolls for non-OOMs captured people owning their own farm. Sample differences also reflect natural population characteristics, since the OOM population is younger with more females compared to the Ontario population [86].
Table 2 provides the distribution of the SDOH measures used in the regression analyses, and shows that the two groups differ significantly on most SDOH. Some SDOH were excluded from the regressions, such as Education and Literacy because educational attainment did not vary in OOMs, Physical Environment because of high colinearity with other measures or absence of a significant health relationship, and Health Service Use since virtually all respondents (both groups) reported having family doctor access. Also excluded from the regressions were traditional health behaviours such as smoking and alcohol consumption, because no OOMs reported either. Employment type was excluded because the majority of members of both groups were farmers. Regarding employment status, more non-OOMs were unemployed than OOMs (28.5% of non-OOMs versus 10.8% of OOMs). Since the majority of the unemployed (over 90%) in both
Table 2. Distribution of Determinant Measures (p-values for χ2 or t test).
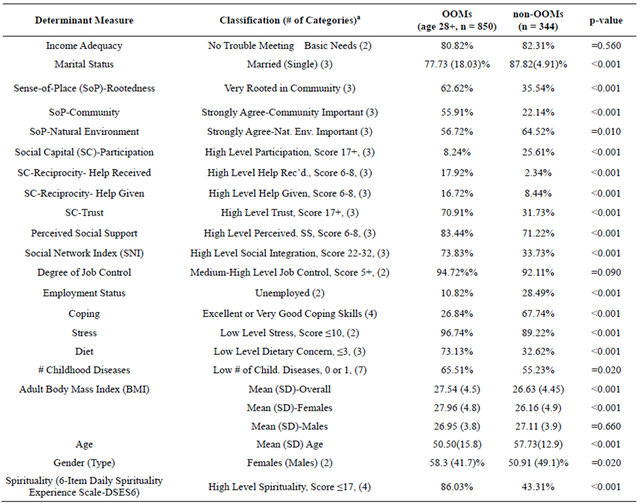
aCategories reduced as needed to meet minimum cell count for χ2 test or avoid exaggerating group differences.
groups indicated that retirement was the reason for unemployment, employment status was highly correlated with age and thus excluded from the regressions.
The groups did not differ on income adequacy or degree of job control, with most participants reporting no trouble meeting basic needs and high job control levels. Most members of both groups were married, with the OOMs having more singles. The OOMs assign more importance to the socially-oriented sense-of-place measures-rootedness and community-and less to the physical environment. For social capital, the OOMs report lower levels of participation and higher levels of trust and reciprocity. OOMs rarely join formal organizations, yet regularly participate within their community, suggesting that social interaction may better capture participation levels. More social interaction in OOMs is evident in the higher social network index (SNI) and perceived social support scores. OOMs report more difficulty coping but less stress, which seems counterintuitive although the stress question may not have captured the full response range or asked about stressors most common in OOMs. OOMs report fewer dietary concerns and childhood diseases. OOMs are shorter (p < 0.001 overall, each gender), with women’s weight being similar to non-OOM women and men’s being less than non-OOM men. Compared to non-OOMs, BMI is higher in OOM women (p < 0.001) and similar in OOM men. OOMs also report significantly higher spirituality levels.
4.2. Health Outcomes
Mean MCS scores are higher (p < 0.001) in OOMs than non-OOMs, indicating better mental health (Table 3). This appears to be largely due to differences in women, with mental health in OOM women being higher and showing less variation compared to non-OOM women. There is no gender difference within OOMs, yet within non-OOMs women have lower MCS scores (p = 0.03). These MCS score differences are statistically significant and of potential clinical significance since they exceed one-the minimum set for interpretation [83,87]. Potential clinical significance means the difference justifies further investigation as it may result from substantive differences in underlying socio-economic conditions. MCS scores in both groups are also negatively skewed, consistent with other SF-12 general population studies [72]. The functional domains used to calculate MCS scores show that group differences are mainly due to OOMs being more social and peaceful and having fewer blue/sad episodes.
Examining MCS scores by age and gender provides further insight into group differences and patterns. Since only 2.6% of non-OOMs (versus 18.6% of OOMs) are ≤34 (lowest age group), we cannot reach conclusions about mental health in this group. However, for the other five age groups, four show MCS differences exceeding one, all in favour of OOM women (marked “s” in Figure 3(a)). For men, only two of the five groups over age 34 have MCS differences exceeding one, both in favour of OOM men (marked “s” in Figure 3(b)). With the exception of non-OOM men, we also see that MCS scores increase with age as in most SF-12 studies [72], and peak in the 65-74 age group as seen in some [83,88].
4.3. Key Determinants Shaping Mental Health
Adjusted R-square values were 0.27 and 0.24 for the OOM and non-OOM regression models respectively, indicating that substantial variation in mental health in both groups remains unexplained (Table 4). In addition to the intercept, three SDOH measures were significant in the regression models of both groups-social interaction, coping and stress-with directionality consistent with the broader literature, pointing to apparently no significant differences between the groups in these areas.
Some SDOH were associated with only one group. Reciprocity (help received) was significant in nonOOMs but not OOMs, with declining mental health linked to an increase in help received. Six SDOH were associated with mental health in OOMs but not nonOOMs. Mental health in OOMs declined with increased
Table 3. SF-12 MCS Statisticsa.
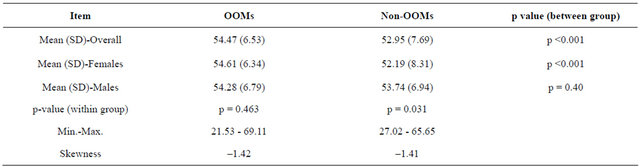
aall t-tests are two-tailed.
Table 4. Regression Model Coefficients, Dependent Variable MCS.
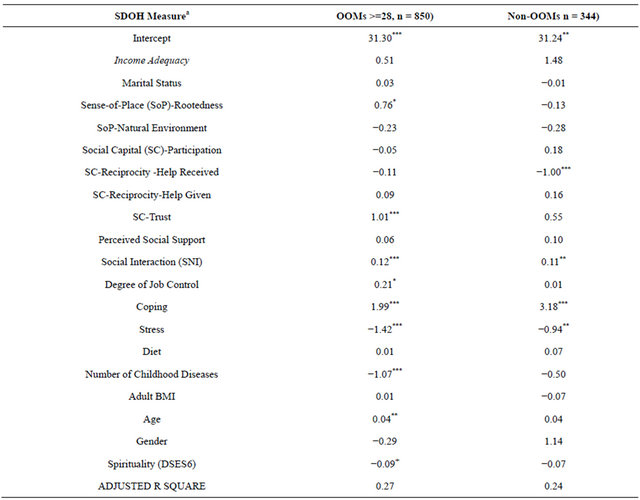
aSoP-Community dropped due to high colinearity with SoP-Rootedness, Employment Status dropped due to high colinearity with Age; ***p <= 0.001, **0.001 < p <= 0.01, *0.01 < p <= 0.05, +0.05< p <= 0.10.
childhood illness, and improved with increasing levels of rootedness, trust, job control, age and spirituality.
Age in the OOM model reflects earlier findings where MCS scores increased with age in men and women (Figures 3(a) and (b)). The absence of age in the nonOOM model likely reflects offsetting gender differences where women’s MCS scores increased with age but men’s did not (Figures 3(a) and (b)). The absence of gender in the OOM model is consistent with the absence of a gender difference in MCS scores (Table 3). However, gender is not significant in the non-OOMs regression even though a gender difference in MCS scores was seen (Table 3), perhaps because gender effects are captured in other significant SDOH (e.g., stress, reciprocity, coping).
We note that our regression models do not include physical functioning as a predictor, despite the evidence linking poor physical and mental health [35]. We exclude physical health because it, like mental health, is a dependent not a determinant in the SDOH literature. Moreover, the SF-12 scoring mechanism produces a measure of physical health (PCS) that is uncorrelated with the MCS score, thus the very low correlations seen in our study (Pearson coefficients of 0.03 and 0.02 for OOMs and non-OOMs). This means PCS would be an insignificant determinant in the MCS model, although our survey data provide alternate measures of physical functioning, e.g., number of chronic conditions. When this variable is included in the MCS model, it is significant (both groups, p = 0.01) without materially changing the significance of the other predictors. The explanatory power of the OOM model does not significantly improve, although the non-OOMs model does (adj. R-square increases to 0.27).
5. DISCUSSION
The purpose of this study was to determine whether mental health was better in OOMs than other rural popu-
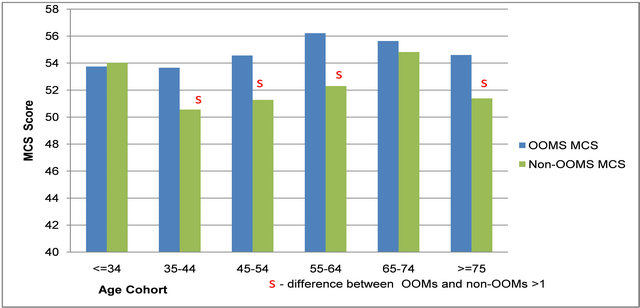 (a)
(a)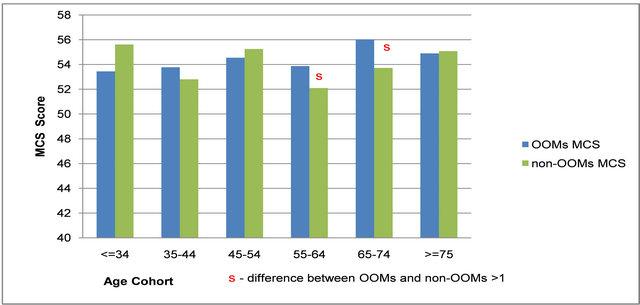 (b)
(b)
Figure 3. (a) FEMALE Mental Component Summary (MCS) Scores for Old Order Mennonites (OOMs) and non-OOMs. (b) MALE Mental Component Summary (MCS) Scores for Old Order Mennonites (OOMs) and non-OOMs.
lations, and identify the key SDOH shaping their mental health. OOM mental health was found to be better than non-OOMs. Since both groups live in the same locale, individual and social/cultural characteristics are more likely to cause health differences.
Better mental health in OOMs may relate to gender. OOM women have higher MCS scores than non-OOM women across most age groups. OOM women also have mental health comparable to OOM men, unlike within the non-OOMs and many other populations where women’s mental health is lower. Our results are consistent with those of a study on the culturally-similar OOA, where OOA women reported better mental health and less unfair gender treatment, stress and partner violence compared to women in the general population [52]. The strong mental health in OOM/OOA women is perhaps surprising given links between poor mental health and women’s subordinate position in patriarchal families [89]. However, patriarchy and traditional gendered roles characterize many farming populations [63,90], thus these are unlikely to explain differences between OOMs and nonOOMs. A closer comparison suggests the following forces may shape the mental health of both genders in our two groups:
1) Gemeinschaft culture: The OOM family farm is viewed as the product of valued, material contributions from both genders-men for their role in farming, and women for childcare, household duties and food production and preservation [47]. Social separation, consistent mutual support, and parochial school/church doctrine reinforce gender roles and traditional values. A secure parental base, a byproduct of the family farm, is also linked to better women’s mental health [14]. Many of these features exist to a lesser degree (if at all) in the non-OOMs. Our survey results indicate higher divorce/ separation rates among non-OOMs (none in OOMs), less perceived social support, and more diverse organizational memberships increasing exposure to alternative roles, views on gender inequality, and devaluation of farming by urban dwellers [63].
2) Technological Change: There are no “factory farms” among the OOMs, who have also been slow to adopt technology. Their more labour-intensive farming practices empower both women and men, providing them with satisfying, valued opportunities to engage in collaborative farm work. Non-OOM farmers in nearby communities cite trends towards “factory farms” requireing increased capitalization [64,65]. Technological change has created steep learning curves and high debt loads, increasing stress and often forcing women to take offfarm jobs to sustain the farm [63,64]. Such “paid” employment is uncommon in OOMs [47,91], causes overload in non-OOM women as it exists in addition to household duties, and is often invisible because it allows the continuation of the farm which is seen as the primary occupation [90].
3) Life-course Involvement: OOMs provide elderly family members with a dwelling (“doddy house”) attached to or located near the farmhouse [91]. This facilitates caring for the elderly, but also allows continued involvement on the family farm. Reference [47, p. 181] notes: “The family farm is for young and old, male and female, grandparents and grandchildren. All contribute and all benefit.” This may explain the differences in OOM MCS scores across the life-cycle, with the happiest of all being OOM women in the 55 - 64 age cohort, followed by OOM males in the 65 - 74 age group (Figures 3(a) and (b)). Does this reflect satisfaction in early grandmothering and later grandfathering experienced by OOMs, or the ongoing involvement of both genders on the family farm? On-farm accommodation of the elderly is uncommon even among other Mennonite groups, with the provision of living centres for seniors being the usual practice in most communities [47].
These differences point to the importance of the social context in which traditional farming gender roles play out. The tight script linking the farm, church and school sends a consistent message to OOMs that is protected by separation. High levels of control are common in Gemeinschaft societies, although the positive health effects seen in this study are not always observed [92].
Social interaction, coping and stress shaped mental health in both groups. The priority that OOMs assign to social interaction is evident from their response to the related SF-12 question. However, the appearance of this determinant in both groups highlights its significance beyond OOMs, which is supported by a broader literature linking low levels of social interaction with higher mortality rates and a range of physical and mental disorders [93]. The significant negative impact of social isolation on health in seven of eight former Soviet countries is a striking, recent reminder of the importance of this determinant [94]. Coping and stress were highly significant for both groups even though they differ on these, indicating their central role in shaping mental health across many populations. This interpretation is supported by [45], who found stress and coping to be among the strongest correlates with psychological distress. Reference [95] also found coping and stress to be important to many health outcomes, and coping to be an important mediator between health and income. We explored this mediation effect in OOMs, where the sample size was sufficient (≥500) for mediation testing. Using the methodology recommended by [96], we confirmed that all mediation conditions were met, that is: significant relationships existed between the predictor and outcome, predictor and mediator, and mediator and outcome; and the relationship between the predictor and outcome was significantly reduced once the mediator entered the model. Reference [96] also provide methods to test the significance of the mediator effect, and applying these we find that coping is a significant mediator (p = 0.05) that mediates 39% of the total effect of income on mental health. The interaction term (income adequacy x coping) was also significant (p = 0.05) in the OOM regression model.
Reciprocity (help received) significantly and negatively shaped mental health in the non-OOMs. Since we do not see this relation in OOMs, it is unlikely to reflect the material reality that people with poorer mental health require more help. More likely, the association reflects the psychosocial effects of receiving help, including stress arising from feelings of indebtedness, being a burden or losing independence [97]. The absence of reciprocity in the OOM model is unexpected given their high levels of both forms of reciprocity (Table 2). However, two other studies found a strong association between individual-level trust and mental health but no association for reciprocity [33,38]. This may reflect theoretical differences between the two constructs, with reciprocity being seen as restricted to personal relations and trust as generalizable to strangers [34]. Unfortunately, many studies combine trust and reciprocity into one measure [35], making it difficult to separate the effects of each construct. Another reason why reciprocity may not shape OOM mental health is that it is common place such that the (high reciprocity) norm may lack psychological impact. The OOM mutual support system is deeplyembedded within their culture and is backed by a long history of meeting the community’s needs [47,91]. Tӧnnies also stressed that social relationships in Gemeinschaft communities are governed by custom, tradition and habit [98]. Reference [34, pp. 189-190] confirms that reciprocity is a particular ethic of “closure networks”, acquiring a familiarity beyond any conscious, deliberate act. Therefore, reciprocity within OOMs may represent a customary norm that is unlikely to trigger feelings of dependence or obligation (as it appears to do in non-OOMs).
Sense-of-place (as rootedness), social capital (as trust), job control, age, spirituality and number of childhood disorders shaped mental health in OOMs only. Most of the predictors of a strong sense-of-place are characteristic of OOMs and non-OOMs alike (e.g., lengthy residence, home ownership, low density housing). Lack of ethnic diversity in the closed OOM community may account for their stronger sense-of-place [29]. Generational experiences, dating back to the early 1800’s for Waterloo OOMs, may result in their stronger sense-of-place by reinforcing individual and group continuity [28,29]. Tӧnnies considered place (land) as one of the three pillars (bonds) of Gemeinschaft [98,99], thus sense-of-place may be an organic element of OOM culture. Sense-ofplace may also arise from the sense of security deeply characteristic of communal societies [92]. However, a strong sense-of-place does not necessarily produce better health [27,100]. Recent studies suggest that it may be important to focus on rural populations and/or mental health [23,30], although rurality alone has been linked to a strong sense-of-place in many but not all studies [29, 101]. While little is known about the mechanisms linking sense-of-place with health, the psychosocial pathway seems to be a plausible mechanism. Chronic exposure to stressors can lead to elevated blood cortisol levels which have been linked to major chronic conditions such as depression, cardiovascular disease, and diabetes [11]. Strong sense-of-place in OOMs could reflect their low stress levels, which could translate into positive physiological changes affecting health. Also, since sense-of-place in OOMs is more socially than physically oriented, it may reflect high levels of social interaction/support or other elements of social capital, which in turn may be linked to positive health outcomes. Reduced stress and increased social interaction were viewed as the most probable pathways linking trust with health in a recent study [102].
The positive association between trust and mental health observed in OOMs has been found in other populations, with trust often rivalling other social capital and traditional health determinants [32,33,94,103,104]. Of the two main types of social capital (bonding and bridging), OOM trust would arise from bonding relations given their closed nature and emphasis on family values [29,103]. However, their mutual aid program, care for the elderly/disabled, legendary “barn raisings” etc. have an international reach that provide OOMs with bridging-like benefits normally acquired by members of mainstream populations through participation in volunteer organizations (e.g., information, advice, work opportunities). Other evidence suggests that OOM trust may be more generalized and include bridging relations. For example, the research team received an extremely positive response from the OOMs, including endorsement of the research agenda and unsolicited offers of help that facilitated community engagement and enabled analyses not otherwise possible. Also, OOMs reported higher levels of trust in our survey for both 1) family/friends, and 2) strangers and first time acquaintances (who would be mainly non-OOMs). These results are consistent with studies finding that informal network trust is a prototype for generalized trust [105]. High levels of generalized trust among OOMs may seem surprising, given their cultural separation and resistance to change because of a fear it will disrupt group unity [47]. However, the local context is also recognized as uniquely supportive, with the OOMs held in high regard by Waterloo’s secular community and its many Mennonite groups [47,61]. This supportive environment is thought to contribute to the high degree of tolerance of outsiders demonstrated by Waterloo OOMs, a feature rarely seen in Gemeinschaft cultures [61]. High trust levels among OOMs may also originate from religious doctrine. Reference [91, p. 145] notes that OOMs “believe in loving others as ourselves, even our enemies. It is our conviction that by living in this manner, we are only doing what is expected of Christians”. Such unconditional love would be difficult to sustain without generalized trust. Regarding the mechanisms underlying the protective effect of high trust on mental health, it has been postulated that social influence and social support impact health through behavioural and psychological pathways such as stress reduction and promotion of a strong sense-of-place [33,103, 106]. Reference [32] theorizes that the psychological pathway is particularly relevant to trust. The low stress levels, high trust and sense-of-place levels, and health linkages of these in OOMs do not contradict the theory of a psychological pathway linking trust with health.
The positive association between job control and mental health in OOMs is supported by a number of studies finding poorer mental health in those with lower levels of control [107]. Although both OOMs and non-OOMs report equally high levels of job control, there are reasons, grounded in materialist and psychosocial theory, regarding its importance in shaping OOM health. OOMs choose to not participate in government programs including social assistance, public health insurance, unemployment insurance, pension and old age security programs. In addition, self-reliance remains a basic virtue taught to all OOMs from childhood, despite the existence of a strong mutual aid system [47]. Reluctance among OOMs to utilize broader safety nets may elevate the importance of job control to ensure adequate material resources and economic stability in meeting ongoing family needs. Also, farming is the sacred vocation valued above all others by OOMs, thus job control may be seen as the way to preserve their culture identity and family ideals [47]. Therefore, the psychosocial pathway represents another potential mechanism through which job control impacts mental health. With more control comes the ability to vary the pace and focus of the work or to support others, all of which have been linked to better mental health in the workplace [107]. Moreover, control allows OOMs to focus on farming, which they view as “physically exhausting, yet mentally and spiritually exhilarating” [47, p. 219]. Links between land, work and pleasure are instrumental in Gemeinschaft cultures according to Tönnies: the first bond (pillar) is with the land, with those working it receiving a sense of enjoyment that “intensifies the reciprocal relationship between work and pleasure” [99].
Improved mental health with age is a common finding in studies employing the SF-12 and GHQ12 (12-item General Household Questionnarie), and the relation often peaks before the oldest age cohorts as seen in our study and others [35,72]. Broader evidence of mental health improving with age also exists in other studies [108]. The psychosocial pathway is the likely mechanism linking age with mental health. In OOMs, comfort and reduced stress likely accompany aging, due to their strong family and community support system and the resulting high levels of social interaction maintained throughout life. Moreover, OOMs rarely fully retire, with women continuing to assist in the home with childcare and household duties and men working in shops building cabinets and other furniture, repairing machinery and manufacturing stabling [91]. Reference [91, p. 234], a scholar and OOM, refers to the positive work-health relation: “the psychological effect of gainful employment among seniors is positive. Life continues to be meaningful. Greater longevity seems to result.”
Linkages of spirituality with better mental health find support in the broader literature [40]. Given the central role of religion in OOM life, it is perhaps not surprising that this determinant shapes their mental health. There is some evidence that religion has more significant effects for those more closely tied to it (e.g., clergy, elders and ministers), however, the effects can be positive or negative depending on the individual [109]. As for why spirituality improves mental health, the following specific mechanisms, grounded in psychosocial (and psychologycal and psychobehavioural) theories, have been suggested, though none are validated by a large body of empirical work at this point: 1) behavioural/motivational, such as attitudes towards smoking, drinking and exercise; 2) interpersonal, such as tangible and emotional support; 3) cognitive, in terms of establishing a mental framework for interpreting life experiences; 4) affective, such as soothing emotions that buffer stress and anxiety; and 5) psychophysiological, such as employing hope and optimism to tackle burdens and restore functionality [110]. These mechanisms are all plausible within OOMs, since religion is the tie binding all cultural elements together. Religion is also a key concept in Tönnies depiction of Gemeinschaft cultures, often reinforcing a variety of community-enhancing behaviours such as the separation and rituals seen in OOMs [92,98].
Finally, our observation of a negative association between childhood illness and mental health in OOMs is consistent with the broader life-course literature [111]. Childhood illness may continue into adulthood or lead to the early onset of disease, which can negatively impact the ability to work, marry, have children, take care of a family and contribute to society. Given the aforementioned absence of a safety net and emphasis on self-reliance among OOMs, it is perhaps not surprising that this determinant significantly shapes their mental health. Many pathways may be involved in linking this determinant with health, including increased illness throughout the life-course, reduced material resources due to employment restrictions, and the psychosocial effects of stress arising from limited participation in social and economic activities In discussing the relative importance of the determinants for mental health, we acknowledge several study limitations. First, responses rely on self-report and interpretation, and are cross-sectional only, although these same limitations are consistently found in most large population studies. Second, results may be limited by the ways in which various determinants were measured. Since we were trying to measure all of the determinants, we were restricted in the number of measures that could be feasibly included in the survey. Third, the non-OOM sample size (344) is below the 500 recommended by the SF-12 developers (for consistency with SF-36 results), with the small sample size also potentially contributing to the lack of significance amongst variables in the nonOOM regression. However, tests conducted for the nonOOMs indicate that the instrument shows acceptable reliability and distinguishes between socio-demographic classes of respondents in the expected manner, and exceeds the small convenience samples often used in SF-12 validity studies [73]. Finally, OLS multiple regressions assume normality, yet a few variables show evidence of non-normality. However, since these variables are negatively skewed, commonly employed data transformations will be ineffective in normalizing them [112].
6. CONCLUSIONS
Despite the above limitations, this research with its focus on the rural, deeply-rooted, community-oriented OOMs highlights a number of important avenues for future research and policy action on the social determinants.
Regarding future research, the sense-of-place relation with health warrants the further study. Is sense-of-place more critical to mental health? How does it relate to other determinants, particularly social indicators such as trust, social interaction and social support? Future research requires clear specification and testing of the pathway linking specific measures of sense-of-place and other social measures to one another and to distinct health outcomes. Our study also points to the need for a detailed, gender-focused analysis of farming cultures. There is variation in contemporary farming, yet little research on the related sociological conditions [113]. Family farms are unlikely to display the same set of social conditions seen among OOMs. Patriarchy, technological change, tradition, local norms and values, social separation, and broader societal support for farming are among the factors that determine gender roles and acceptance of them. However, how these factors vary across farm communities and how they impact mental health remains poorly understood. Our results also show the importance of breaking down determinant constructs and distinguishing between them theoretically and empirically. For example, distinguishing between different types of social capital is important, given that our study and others show: 1) a weaker than expected correlation between social capital measures, and 2) the highly influential role of specific measures such as trust. Our distinction between reciprocity received and given further highlights the importance of breaking down constructs, as doing so may expose directional differences in functional elements.
Studying OOMs highlights the importance of trust, which appears to be generalized and result from deeply embedded cultural values, consistent mutual support, strong support from surrounding populations, and seclusion limiting exposure to growing levels of broad-based societal mistrust [114]. However, this does not mean we have to be an OOM to be trusting, even though they are more likely to reciprocate. Top-down and bottom-up programs can be developed to cultivate trust in general populations. Reference [32] found that social capital (trust, participation) and health can change in as little as six years. This short timeline is highlighted in the empirical regularity cited by [115, pp. 104-105]: “Persons are slow to trust a friend but quick to trust a ‘confidence man’, someone they have never seen before.” This is because there is less to lose confiding in a stranger; it does not threaten the close bond that develops (over long periods of time) with personal relations. It is reassuring that trust in strangers takes less time, since these relations encompass a broader range of people and thus represent an efficient target for population health intervenetion. Ultimately, these aspects of trust (a learned capacity, a short timeline for developing generalized trust) should increase the appeal of social capital interventions for term-oriented policy makers.
Our results also support action on determinants such as coping, stress and social interaction, which were found to be significant for both our groups. Support can be found in the broader literature as well, suggesting that these determinants transcend the boundaries of OOMs, farmers, rural residents and Canadians. They likely warrant multiple interventions-enhancing services to help individuals cope, manage stress and increase interaction; adding community programs that alleviate the broader economic/social conditions that challenge peoples’ ability to cope, manage stress or interact; and ensuring that these programs include children and are sustainable over the life-course. Since the determinants involve public health and other sectors, interagency cooperation is important for developing effective community programs (e.g., childcare programs coordinated with local employers and educational institutions).
Studying OOMs has highlighted the important role that many social determinants play in shaping mental health, including trust, spirituality, job control and senseof-place. These determinants, while measured at the individual level, are contextual phenomena that reflect underlying social conditions within the OOM community. They owe their strength to a communal (Gemeinschaft) culture and “sense of community matched by none” [47, p. 186]. OOMs continue to flourish in Waterloo, remaining united and strong despite the trend towards independence (Gesellschaft) that few societies have escaped.
7. ACKNOWLEDGEMENTS
We are indebted to the members of the Old Order Mennonite community of Waterloo (Ontario, Canada) for their trust, support and participation in this study. We also acknowledge the support and assistance of the Senior Bishop and deacons, who distributed the survey to the 13 Meeting Houses in the Waterloo community.
REFERENCES
- Public Health Agency of Canada PHAC (2011) What determines health? Retrieved 10 September 2011. http://www.phac-aspc.gc.ca/ph-sp/determinants/index-eng.php#determinants
- WHO (2007) Discussion paper for the commission on social determinants of health. Draft Document Dated April 2007. Retrieved 13 October 2011. http://www.who.int/social_determinants/resources/csdh_framework_action_05_07.pdf
- Smith, B.K., Humphreys, J.S. and Wilson. M.G.A. (2008) Review article: Addressing the health disadvantage or rural populations: How does epidemiological evidence inform rural health policies and research? Australian Journal Rural Health, 16, 56-66. doi:10.1111/j.1440-1584.2008.00953.x
- Wilson, K., Eyles, J., Elliott, S. and Keller-Olaman, S. (2009) Health in Hamilton neighbourhoods: Exploring the determinants of health at the local level. Health and Place, 15, 374-382. doi:10.1016/j.healthplace.2008.07.002
- Reimer, L.M. (2008) One quilt many pieces: A guide to Mennonite groups in Canada. Herald Press, Waterloo.
- Maziak, W. (2009) Point-counterpoint: The triumph of the null hypothesis-epidemiology in an age of change. International Journal of Epidemiology, 38, 393-402. doi:10.1093/ije/dyn268.
- Rudan, I. (2006) Health effects of human population isolation and admixture. Croation Medical Journal, 47, 526- 531.
- Fryers, T., Melzer, D. and Jenkins, R. (2003) Social inequalities and the common mental disorders: A systematic review of the evidence. Social Psychiatry and Psychiatric Epidemiology, 38, 229-237. doi:10.1007/s00127-003-0627-2
- Hong, J., Martin, K. and Alistair, M. (2011) Income-related inequalities in the prevalence of depression and suicidal behaviour: A 10-year trend following economic crisis. World Psychiatry, 10, 40-44.
- Zhang, W., Chen, Q., McCubbin, H., McCubbin, L. and Foley, S. (2011) Predictors of mental and physical health: Individual and neighbourhood levels of education, social well-being, and ethnicity. Health and Place, 17, 238-247. doi:10.1016/j.healthplace.2010.10.008
- Marmot, M. and Wilkinson, R.G. (2008) Social determinants of health. 2nd Edition, Oxford University Press, Oxford.
- Madden, D. (2010) Gender difference in mental wellbeing: A decomposition analysis. Social Indicators Research, 99, 101-114. doi:10.1007/s11205-009-9569-8
- Oksuzyan, A., Crimmins, E., Saito, Y., O’Rand, A., Vaupel, J.W. and Christensen, K. (2010) Cross-national comparison of sex differences in health and mortality in Denmark, Japan and the US. European Journal of Epidemiology, 25, 471-480. doi:10.1007/s10654-010-9460-6
- Ussher, J.M. (2010) Are we medicalizing women’s misery? A critical review of women’s higher rates of reported depression. Feminism and Psychology, 20, 9-35. doi:10.1177/0959353509350213
- Kivimaki, M., Jokela, M., Hamer, M., Geddes, J., Ebmeier, K., Kumari, M., Singh-Manoux, A., Hingorani, A. and Batty, G.D. (2011) Examining overweight and obesity as risk factors for common mental disorders using fat mass and obesity associated FTO genotype instrumented analysis. American Journal of Epidemiology, 173, 421- 429. doi:10.1093/aje/kwq444
- Turner, R.J. and Lloyd, D.A. (1999) The stress process and the social distribution of depression. Journal of Health and Social Behavior, 40, 374-404. doi:10.2307/2676332
- Thoits, P.A. (2010) Stress and health: Major findings and policy implications. Journal of Health and Social Behaviour, 51S, S41-S53. doi:10.1177/0022146510383499
- Fone, D., Dunstan, F., Lloyd, K., Williams, G., Watkins, J. and Palmer, S. (2007) Does social cohesion modify the association between area income deprivation and mental health? A multilevel analysis. International Journal of Epidemiology, 36, 338-345. doi:10.1093/ije/dym004
- Galea, S., Ahern, J., Nandi, A., et al. (2007) Urban neighbor-hood poverty and the incidence of depression in a population-based cohort study. Annals of Epidemiology, 17, 171-179. doi:10.1016/j.annepidem.2006.07.008
- Sundquist, K. and Ahlen, H. (2006) Neighbourhood income and mental health: A multilevel follow-up study of psychiatric hospital admissions among 4.5 million women and men. Health and Place, 12, 594-602. doi:10.1016/j.healthplace.2005.08.011
- Butterworth, P., Rogers, B. and Jorm, A.F. (2006) Examining geographical and household variation in mental health in Australia. Australian and New Zealand Journal of Psychiatry, 40, 491-497. doi:10.1080/j.1440-1614.2006.01827.x
- Gale, C.R., Dennison, E.M., Cooper, C. and Sayer. A.A. (2011) Neighbourhood environment and positive mental health in older people: The Hertfordshire Cohort Study. Health and Place, 17, 867-874. doi:10.1016/j.healthplace.2011.05.003
- Kelly, B., Lewin, T.J., Stain, H.J., Coleman, C., Fitzgerald, M., Perkins, D., Carr, V.J., Fragar, L., Fuller, J., Lyle, D. and Beard, J.R. (2011) Determinants of mental health and well-being within rural and remote communities. Social Psychiatry Psychiatric Epidemiology, 46, 1331-1342. doi:10.1007/s00127-010-0305-0
- Peterson, L.E., Tsai, A.C., Petterson, S. and Litaker, D.G. (2009) Rural-urban comparison of contextual associations with self-reported mental health status. Health and Place, 15, 125-132. doi:10.1016/j.healthplace.2008.03.001
- Propper, C., Jones, K., Bolster, A., Burgess, S., Johnston, R. and Sarker, R. (2005) Local neighbourhood and mental health: Evidence from the UK. Social Science and Medicine, 61, 2065-2083. doi:10.1016/j.socscimed.2005.04.013
- Young, A.F., Russell, A. and Powers, J.R. (2004) The sense of belonging to a neighbourhood: Can it be measured and is it related to health and well being in older women? Social Science and Medicine, 59, 2627-2637. doi:10.1016/j.socscimed.2004.05.001
- Eyles, J.D. and Williams, A. (2008) Sense of place, health and quality of life. MPG Books Limited, Great Britain.
- Hay, R. (1998) Sense of place in developmental context. Journal of Environmental Psychology, 18, 5-29. doi:10.1006/jevp.1997.0060
- Lewicka, M. (2011) Place attachment: How far have we come in the last 40 years. Journal of Environmental Psychology, 31, 207-230. doi:10.1016/j.jenvp.2010.10.001
- Romans, S., Cohen, M. and Forte, T. (2011) Rates of depression and anxiety in urban and rural Canada. Social Psychiatry Psychiatric Epidemiology, 46, 567-575. doi:10.1007/s00127-010-0222-2
- Bhandari, H. and Yasunobu, K. (2009) What is social capital: A comprehensive review of the concept. Asian Journal of Social Science, 37, 480-510. doi:10.1163/156853109X436847
- Giordano, G.N. and Lindstrom, M. (2010) The impact of changes in different aspects of social capital and material conditions on self-rated health over time: A longitudinal cohort study. Social Science and Medicine. 70: 700-710. doi:10.1016/j.socscimed.2009.10.044
- Kim, S. C. Yeonseung, M. Perry, I. Kawachi. S. Subramanian. 2012. Association between Interpersonal Trust, Reciprocity, and Depression in South Korea: A Prospective Analysis. PLoS ONE, 7, 1-8, e30602.
- Torche, F. and Valenzuela, E. (2011) Trust and reciprocity: A theoretical distinction of the sources of social capital. European Journal of Social Theory, 14, 181-198. doi:10.1177/1368431011403461
- Nieminen, T., Martelin, T., Koskinen, S., Aro, H., Alanen, E. and Hyyppa, M.T. (2010) Social capital as a determinant of self-rated health and psychological well-being. International Journal of Public Health, 55, 531-542. doi:10.1007/s00038-010-0138-3
- De Silva, M.J., McKenzie, K., Harpham, T. and Huttly, S.R. (2005) Social capital and mental illness: A systematic review. Journal of Epidemiology and Community Health, 59, 619-627. doi:10.1136/jech.2004.029678
- Phongsavan, P., Chey, T., Bauman, A., Brooks, R. and D. Silove (2006) Social capital, socio-economic status and psychological distress among Australian adults. Social Science and Medicine, 63, 2546-2561. doi:10.1016/j.socscimed.2006.06.021
- Fujiwara, T. and Kawachi, I. (2008) A prospective study of individual-level social capital and major depression in the United States. Journal of Epidemiology and Community Health, 62, 627-633. doi:10.1136/jech.2007.064261
- Kier, F.J. and Davenport, D.S. (2004) Unaddressed problems in the study of spirituality and health. American Psychologist, 59, 53-54. doi:10.1037/0003.066X.59.1.53
- Koenig, H.G., McCullough, M.E. and Larson, D.B. (2001) Handbook of religion and health. Oxford University Press, New York. doi:10.1093/acprof:oso/9780195118667.001.0001
- Salsman, J.M., Brown, T.L., Brechting, E.H. and Carlson, C.R. (2005) The link between religion and spirituality and psychological adjustment: The mediating role of optimism and social support. Personality and Social Psychology Bulletin, 31, 522-535. doi:10.1177/0146167204271563
- Hwang, K., Hammer, J.H. and Cragun, R.T. (2011) Extending religion-health research to secular minorities: Issues and concerns. Journal of Religion Health, 50, 608- 622.
- King, M.B. and Koenig, H.G. (2009) Conceptualising spirituality for medical research and health service provision. BMC Health Services Research, 9, 1-7. doi:10.1186/1472-6963-9-116
- Schlehofer, M., Omoto, A.M. and Adelman, J.R. (2008) How do religion and spirituality differ? Lay definitions among older adults. Journal for the Scientific Study of Religion, 47, 411-425. doi:10.1111/j.1468-5906.2008.00418.x
- Caron, J. and Liu, A. (2011) Factors associated with psychological distress in the Canadian population: A comparison of low-income and non low-income sub-groups. Community Mental Health Journal, 47, 318-330.
- Puffenberger, E.G. (2003) Genetic heritage of the old order mennonites of southeastern Pennsylvania. American Journal of Medical Genetics. Part C. Semin. Med. Genet. 121C, 18-31. doi:10.1002/ajmg.c.20003
- Fretz, J.W. (1989) The Waterloo mennonites: A community in paradox. Wilfred Laurier University Press, Waterloo.
- Bassett Jr., D.R., Tremblay, M.S., Esliger, D.W.. et al. (2007) Physical activity and body mass index of children in an old order Amish community. Medicine and Science in Sports and Exercise, 39, 410-415.
- Esliger, D.W., Bassett Jr., D.R., Tremblay, M.S. and Copeland, J.L. (2010) Physical activity profile of old order Amish, Mennonite and contemporary children. Medicine and Science in Sports and Exercise, 42, 296-308. doi:10.1249/MSS.0b013e3181b3afd2
- Tremblay, M.S., Barnes, J.D., Copeland, J.L. and Esliger, D.W. (2005) Conquering childhood inactivity: Is the answer in the past? Medicine and Science in Sports and Exercise, 37, 1187-1194. doi:10.1249/01.mss.0000170079.71522.a6
- Hewner, S. (1998) Fertility, migration and mortality in an old order Amish community. American Journal of Human Biology, 10, 619-628. doi:10.1002/(SICI)1520-6300(1998)10:5<619::AID-AJHB8>3.0.CO;2-8
- Miller, K., Yost, B., Flaherty, S., Hillemeier, M.M., Chase, G.A., Weisman, C.S. and Dyer, A.-M. (2007) Health status, health conditions, and health behaviours among Amish women: Results from the central Pennsylvania women’s health study CePAWHS. Women’s Health Issues, 17, 162-171. doi:10.1016/j.whi.2007.02.011
- Glick, M., Michel, A.C., Dorn, J., Horwitz, M., Rosenthal, T. and Trevisan, M. (1998) Dietary cardiovascular risk factors and serum cholesterol in an old order mennonite community. American Journal of Public Health, 88, 1202-1205.
- Hamman, R.F., Barancik, J.I. and Lilienfeld, A.M. (1981) Patterns of mortality in the old order Amish. American Journal of Epidemiology, 114, 845-861.
- Troyer, H. (1988) Review of cancer among 4 religious sects: Evidence that lifestyles are distinctive sets of risk factors. Social Science and Medicine, 26, 1007-1017. doi:10.1016/0277-9536(88)90218-3
- Westman, J.A., Ferketich, A.K., Kauffman, R.M., MacEachern, S.N., Wilkins, J.R., Wilcox, P.P., Pilarski, R.T., Nagy, R., Lemeshow, S., de la Chapelle, A. and Bloomfield, C.D. (2010) Low cancer incidence rates in Ohio Amish. Cancer Causes Control, 21, 69-75. doi:10.1007/s10552-009-9435-7
- Hsueh, W.-C., Mitchell, B.D., Schneider, J.L., St. Jean, P.L., Pollin, T.I., Ehm, M.G., Wagner, M.J., D.K., Burns, H.S., Bell, C.J. andShuldiner, A.R. (2001) Genome-Wide scan of obesity in the old order Amish. The Journal of Clinical Endrocrinology and Metabolism, 86, 1199-1205. doi:10.1210/jc.86.3.1199
- CIHI (Canadian Institute of Health Information) (2006) How healthy are rural Canadians? An assessment of their health status and health determinants. Prepared by Canadian Population Health Initiative part of CIHI, Public Health Agency of Canada PHAC and the Centre for Rural and Northern Health Research Laurentian University.
- Wang, J.L. (2004) Rural-urban differences in the prevalence of major depression and associated impairment. Social Psychiatry and Psychiatric Epidemiology, 39, 19-25. doi:10.1007/s00127-004-0698-8
- [61] van Hoojidonk, C., Droomers, M., van Loon, J.A.M., van der Lucht, F. and Kunst, A.E. (2007) Exceptions to the rule: Healthy deprived areas and unhealthy wealthy areas. Social Science and Medicine, 64, 1326-1342. doi:10.1016/j.socscimed.2006.10.041
- [62] Gingrich, L.G. and Lightman, E. (2006) Striving toward self-sufficiency: A qualitative study of mutual aid in an old order Mennonite community. Family Relations, 55, 175-189. doi:10.1111/j.1741-3729.2006.00368.x
- [63] Tönnies, F. (1887/1991) Gemeinschaft and gesellschaft: Frundbegriffe der reinen sociologie. Wissenschaftliche Buchgesellschaft, Darmstadt.
- [64] Leipert, B. and George, J. (2008) Determinants of rural women’s health: A qualitative study in southwest Ontario. The Journal of Rural Health, 24, 210-218. doi:10.1111/j.1748-0361.2008.00160.x
- [65] Smithers, J. and Johnson, P. (2004) The dynamics of family farming in North Huron County, Ontario. Part I: Development trajectories. The Canadian Geographer, 48, 191-208. doi:10.1111/j.0008-3658.2004.00055.x
- [66] Smithers, J., Johnson, P. and Joseph, A. (2004) The dynamics of family farming in North Huron County, Ontario. Part II: Farm-community interactions. The Canadian Geographer, 48, 209-224.
- [67] Foodlink Waterloo Region (2011) Agriculture in our region: Find healthy local food in Waterloo region. http://www.kwnow.ca/cdps/cditem.cfm?nid=16257
- [68] Ware, Jr., J.E., Kosinski, M. and Keller, S.D. (1996) A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220-226. doi:10.1097/00005650-199603000-00003
- [69] Gill, S.C., Butterworth, P., Rodgers, B. and Mackinnon, A. (2007) Validity of the mental health component scale of the 12-item Short-Form Health Survey MCS-12 as measure of common mental disorders in the general population. Psychiatry Research, 152, 63-71.
- [70] Fleishman, J.A., Selim, A.J. and Kazis, L.E. (2010) Deriving SF-12v2 physical and mental health summary scores: A comparison of different scoring algorithms. Quality of Life Research, 19, 231-241. doi:10.1007/s11136-009-9582-z
- [71] Gandek, B., Ware, J.E., Aaronson, N.K., Apolone, G., Bjorner, J.B., Brazier, J.E., Bullinger, M., Kaasa, S., Leplege, A., Prieto, L. and Sullivan, M. (1998) Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. Journal of Clinical Epidemiology, 51, 1171-1178. doi:10.1016/S0895-4356(98)00109-7
- [72] Gandek, B.G., Ware Jr., J.E., Aaronson, N.K., Alonso, J., Apolone, G., Bjorner, J., Brazier, J., Bullinger, M., Fukuhara, S., Kaasa, S., Leplège, A. and Sullivan, M. (1998) Tests of data quality, scaling assumptions, and reliability of the SF-36 In eleven countries: Results from the IQOLA Project. Journal of Clinical Epidemiology, 51, 1149-1158. doi:10.1016/S0895-4356(98)00106-1
- [73] Kontodimopoulos, N., Pappa, E., Niakas, D. and Tountas, Y. (2007) Validity of SF-12 summary scores in a Greek general population. Health and Quality of Life Outcomes, 5, 1-9.
- [74] Okonkwo, O.C., Roth, D.L., Pulley, L.V. and Howard, G. (2010) Confirmatory factor analysis of the validity of the SF-12 for persons with and without a history of stroke. Quality of Life Research, 19, 1323-1331. doi:10.1007/s11136-010-9691-8
- [75] Fisher, K. and Newbold, K.B. (2013) Validity of the SF-12 in a Canadian Old Order Mennonite Community. Applied Research in Quality of Life, in Press.
- [76] Cohen, S. and Wills, T.A. (1985) Stress, social support and the buffering hypothesis. Psychological Bulletin, 98, 310-357.
- [77] Berkman, L. (1977) Social networks and health. University of Berkeley, Berkeley.
- [78] Statistics Canada (2011) Retrieved August 31, 2011. http://www.statcan.gc.ca/concepts/health-sante/index-eng.htm
- [79] Smith, J.P. (2009) Reconstructing childhood health histories. Demography, 46, 387-403. doi:10.1353/dem.0.0058
- [80] Krieger, N. and Smith, G.D. (2004) Bodies count and body counts: Social epidemiology and embodying inequality. Epidemiological Reviews, 26, 92-103. doi:10.1093/epirev/mxh009
- [81] Krieger, N. (2001) Theories for social epidemiology in the 21st century: An ecosocial perspective. International Journal of Epidemiology, 30, 668-677. doi:10.1093/ije/30.4.668
- [82] Underwood, B. (2011) Daily spiritual experience scale. http://dsescale.org/
- [83] Krieger, N. (1999) Embodying inequality: A review of concepts, measures and methods for studying health consequences of discrimination. International Journal of Health Services, 29, 295-352. doi:10.2190/M11W-VWXE-KQM9-G97Q
- [84] Ware Jr., E., Kosinski, M. and Keller, S.D. (1995) How to score the SF-12 physical and mental health summary scales. 2nd Edition, The Health Institute, Boston.
- [85] Hopman, W.M., Berger, C., Joseph, L., Towheed, T., Anastassiades, T., Tenenhouse, A., Poliquin, S., Berger, C., Brown, J.P., Murray, T.M., Adachi, J.D., Hanley, D.A., Papadimitropoulos, E. and CaMos Research Group (2002) Is there regional variation in the SF-36 scores of Canadian adults. Canadian Journal of Public Health, 93, 233- 237.
- [86] Hopman, W.M., Towheed, T., Anastassiades, T., Tenenhouse, A., Poliquin, S., Berger, C., Joseph, L., Brown, J.P., Murray, T.M., Adachi, J.D., Hanley, D.A., Papadimitropoulos, E. and the Canadian Multicentre Osteoporosis Study Research Group (2000) Canadian normative data for the SF-36 health survey. Canadian Medical Association Journal, 163, 265-271.
- [87] Statistics Canada (2011) 2006 census tables. http://www12.statcan.ca/census-recensement/2006/dp-pd/hlt/97-551/pages/page.cfm?Lang=EandGeo=PRandCode=01andTable=1andData=CountandSex=2andStartRec=1andSort=2andDisplay=Page
- [88] Taft, C., Karlsson, J. and Sullivan, M. (2001) Reply to Drs War and Kosinski. Quality of Life Research, 10, 415-420. doi:10.1023/A:1012552211996
- [89] Hanmer, J., Lawrence, W.F., Anderson, J.P., Kaplan, R.M. and Fryback, D.G. (2006) Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Medical Decision Making, 26, 391-400. doi:10.1177/0272989X06290497
- [90] WHO (2009) Women and health: Today’s evidence, tomorrow’s agenda. World Health Organization, Geneva.
- [91] Heather, B., Skillen, L., Young, J. and Vladicka, T. (2005) Women’s gendered identities and the restructuring of rural Alberta. Sociologia Ruralis, 45, 88-97.
- [92] Horst, I. (2000) A separate people: An insider’s view of old order Mennonite customs and traditions. Herald Press, Waterloo.
- [93] Brint, S. (2001) Gemeinschaft revisited: A critique and reconstruction of the community concept. Sociological Theory, 19, 1-23. doi:10.1111/0735-2751.00125
- [94] Stansfeld, S. (2008) Social cohesion and social support. In: Marmot, M. and Wilkinson, R.G., Eds., Social Determinants of Health, 2nd Edition, Oxford University Press, Oxford, 148-171.
- [95] d’Hombres, B., Lorenzo, R., Suhrcke, M., et al. (2011) The influence of social capital on health in eight former Soviet countries: why does it differ? Journal of Epidemiology of Community Health, 65, 44-50. doi:10.1136/jech.2009.097592
- [96] Poetz, A., Eyles, J.D., Elliott, S., Wilson, K. and KellerOlaman, S. (2007) Path analysis of income, coping and health at the local level in a Canadian context. Health and Social Care in the Community, 15, 542-552. doi:10.1111/j.1365-2524.2007.00715.x
- [97] Frazier, P.A., Tix, A.P. and Barron, K.E. (2004) Testing moderator and mediator effects in counseling psychology research. Journal of Counseling Psychology, 51,115-134. doi:10.1037/0022-0167.51.1.115
- [98] Abbott, S. and Freeth, D. (2008) Social capital and health: Starting to make sense of the role of generalized trust and reciprocity. Journal of Health Psychology, 13, 874-883. doi:10.1177/1359105308095060
- [99] Tilman, R. (2004) Ferdinand Tönnies, Thorstein Veblen and Karl Marx: From community to society and back? European Journal of the History of Economic Thought, 11, 579-606. doi:10.1080/0967256042000292114
- [100] Adair-Toteff, C. (1995) Ferdinand Tönnies: Utopian visionary. Sociological Theory, 13, 58-65. doi:10.2307/202006
- [101] Carpiano, R.M. and Hystad, P.W. (2011) Sense of belonging in health surveys: What social capital is it measuring? Health and Place, 17, 606-617. doi:10.1016/j.healthplace.2010.12.018
- [102] Stain, H.J., Kelly, B., Lewin, T.J., Higginbotham, N., Beard, J.R. and Hourihan, F. (2008) Social networks and mental health among a farming population. Social Psychiatry and Psychiatric Epidemiology, 43, 843-849. doi:10.1007/s00127-008-0374-5
- [103] Jen, M.H., Sund, E.R., Johnston, R. and Jones, K. (2010) Trustful societies, trustful individuals and health: An analysis of self-rated health and social trust using the World Values Survey. Health and Place, 16, 1022-1029. doi:10.1016/j.healthplace.2010.06.008
- [104] Ferlander, S. and Makinen, I.H. (2009) Social capital, gender and self-rated health. Evidence from the Moscow Health Survey 2004. Social Science and Medicine, 69, 1323-1332.
- [105] Mansyur, C., Amick, B.C., Harrist, R.B. and Franzini, L. (2008) Social capital, income inequality, and self-rated health in 45 countries. Social Science and Medicine, 66, 43-56. doi:10.1016/j.socscimed.2007.08.015
- [106] Glanville, J.L. and Paxton, P. (2007) How do we learn to trust? A confirmatory tetrad analysis of the sources of generalized trust. Social Psychology Quarterly, 70, 230- 242. doi:10.1177/019027250707000303
- [107] Kawachi, I. and Berkman, L. (2001) Social ties and mental health. Journal of Urban Health, 78, 458-467. doi:10.1093/jurban/78.3.458
- [108] Marmot, M., Siegrist, J. and Theorelle, T. (2008) Health and the psychosocial environment at work. Social Determinants of Health, 2nd Edition, Oxford University Press, Oxford, 97-130.
- [109] Delaney, K. (2012) Insights of the elderly. New York Times, Saturday, 11 February 2012.
- [110] Pargament, K., Tarakeshwar, N., Ellison, C.G. and Wulff, K.W. (2001) Religious coping among the religious: The relationship between religious coping and well-being in a national sample of presbyterian clergy, elders and members. Journal for the Scientific Study of Religion, 40, 497- 513. doi:10.1111/0021-8294.00073
- [111] Levin, J. (2009) How faith heals: A theoretical model. Explore, 5, 77-96. doi:10.1016/j.explore.2008.12.003
- [112] Blane, D. (2008) The life course, the social gradient and health. In: Marmot, M. and Wilkinson, R.G., Eds., Social Determinants of Health, 2nd Edition, Oxford University Press, Oxford, 54-77.
- [113] Sheskin, D.J. (2007) Handbook of parametric and nonparametric statistical procedures. 4th Edition, Chapman and Hall/CRC, Taylor and Francis Group, Boca Raton.
- [114] Roche, M. (2002) Rural geography: Searching rural geographies. Progress in Human Geography, 26, 823-829. doi:10.1191/0309132502ph406oa
- [115] Dowbiggin, I.R. (2009) High anxieties: The social construction of anxiety disorders. Canadian Journal of Psychiatry, 54, 429-435.
- [116] Coleman, J.S. (1990) The foundations of social theory. Harvard University Press, Cambridge.

