Open Journal of Anesthesiology
Vol.3 No.3(2013), Article ID:31255,4 pages DOI:10.4236/ojanes.2013.33034
Comparison of Clinical Problems in Thoracoscopic Esophagectomy between Prone Position with Pneumothorax Procedure and Lateral Position*
![]()
1Department of Anesthesiology, Osaka City General Hospital and Children’s Hospital 2-13-22 Miyakojima-Hondori, MiyakojimaKu, Osaka, Japan; 2Department of Digestive Surgery, Osaka City General Hospital and Children’s Hospital 2-13-22 MiyakojimaHondori, Miyakojima-Ku, Osaka, Japan.
Email: #yoshihirokasagi@hotmail.com
Copyright © 2013 Yoshihiro Kasagi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 18th, 2013; revised April 19th, 2013; accepted May 6th, 2013
Keywords: Thoracoscopic Esophagectomy; Prone Position; Lateral Position; CO2 Pneumothorax; Oxygenation
ABSTRACT
Study Objective: We compared the effects of intraoperative body position on blood gas and fluid balance in patients undergoing a thoracoscopic esophagectomy as well as during operation and postoperative laboratory data. Design: Prospective study. Setting: Operating room and intensive care unit. Patients: ASA physical status 1 and 2 patients (n = 26), scheduled for elective thoracoscopic esophagectomy and immediate reconstruction under general anesthesia with one-lung ventilation were enrolled. Interventions: Patients were assigned to either the lateral (n = 16) or prone (n = 10) position groups based on the planned intraoperative body position. A pneumothorax procedure was concomitantly performed only in the prone position group. Measurements: Fluid balance, PaO2/FIO2 ratio (P/F ratio), and maximum PaCO2 during the operation and postoperative laboratory data were analyzed. Main Results: There were no significant differences between the groups for amount of blood loss, blood transfusion, fluid infusion, or urine output. The P/F ratio during one-lung ventilation was significantly higher in the prone than the lateral position group (379 ± 122 vs. 297 ± 67 mmHg, p = 0.017), as was maximum intraoperative PaCO2 (72.2 ± 15.6 vs. 48.3 ± 6.3 mmHg, p < 0.001). Conclusions: A thoracoscopic esophagectomy in the prone position performed concomitantly with a CO2 pneumothorax procedure resulted in a significantly better P/F ratio during one-lung ventilation as compared to the lateral position, indicating that the prone position is more advantageous for oxygenation.
1. Introduction
The less invasive characteristics of a thoracoscopic esophagectomy procedure in the lateral position in comparison with an open esophagectomy have been shown [1]. However, the lateral position presents technical disadvantages, such as visualization obstructed by the lung and accumulated bleeding, resulting in frequent changes of instruments and prolonged operative time [2].
In 1994, Cuschieri proposed positioning patients undergoing this procedure into a prone position [3], while Palanivelu et al. reported outcomes of a prone thoracoscopic esophagectomy performed with a CO2 pneumothorax procedure in 2006 [4]. In the prone position, the lung becomes located in a lower position by gravity and CO2 pressure in cases that undergo a concomitant pneumothorax procedure, allowing for blood to pool outside of the operative field. These conditions provide a better operative view for the surgeon, and decrease the amount of retraction of the lung and frequency of instrument changes [2]. Fabian et al. also reported significantly shorter times for thoracoscopic procedures in the prone position in comparison to the lateral position due to decreased retraction and fewer instrument changes [5].
However, prone positioning during an esophagectomy leads to inevitable hypercapnia in cases that utilize a CO2 pneumothorax procedure and the risk of tracheal tube complications is increased. Few studies have compared between the prone and lateral positions in patients undergoing a thoracoscopic esophagectomy procedure, thus we sought to identify clinical differences between these intraoperative positions in the present study.
2. Patients and Methods
Twenty-six patients underwent a thoracoscopic esophagectomy procedure and immediate reconstruction performed by a single surgeon from March 2008 to March 2010 at Osaka City General Hospital.
An epidural catheter was inserted 5 cm cranial from Th6-Th9 and 3 ml of 1.5% lidocaine (45 mg) was injected on a trial basis. Approximately 3 minutes later, absence of signs of subarachnoid anesthesia was confirmed and general anesthesia was induced. After setting the target control infusion of propofol concentration in blood to 2.8 - 3.5 μg/ml, general anesthesia was maintained by intermittent administrations of fentanyl and vecuronium, while 1.5% lidocaine was administered at 4 - 8 ml/hour through the epidural catheter. A BIS sensor (BIS XP version 4.0; Aspect Medical Systems, Natick, MA, USA) was attached to the frontal region for monitoring. For respiratory management, a left-sided double lumen tube (Broncho-cath: Tyco Healthcare, Argyle, Mansfield, MA, USA) was utilized. After securing the airway, the patient was changed to a lateral decubitus or prone position, with the following ventilation conditions: inspired oxygen concentration, 1.0 - 0.7; pressure-limited method; maximal inspiratory pressure, 15 - 25 cm H2O; positive end-expiratory pressure, 5 cm of H2O; respiratory rate, 15 - 20 breaths/minute; and tidal volume, 220 - 300 ml.
Patients were divided into the prone (n = 10) and lateral (n = 16) position groups, according to the planned intraoperative positioning by chief surgen. A CO2 pneumothorax procedure with 8 mmHg of CO2 pressure was also utilized in all patients in the prone position group except for 1 case with a CO2 pressure of 5 mmHg, while none in the lateral position group, underwent that procedure. Patients who underwent a second reconstruction or limited operation were excluded from analysis.
For patient background characteristics, we examined age, American Society of Anesthesiologists physical status, Brinkman index, and preoperative respiratory function between the groups. To clarify clinical differences, we examined operative time, one-lung ventilation time, anesthesia time, amount of bleeding, amount of blood transfusion, arterial blood gas data, and clinical laboratory data (white blood cell count, C-reactive protein, total protein, albumin).
3. Statistical Analysis
The statistical significance of differences observed between the groups was assessed with a two-tailed MannWhitney U-test using yStat 2008 software (statistical program file developed with Microsoft Excel, Igakutoshoshuppan, Tokyo, Japan). Differences were considered significant when the P value was < 0.05.
4. Results
There were no significant differences between the groups for age, American Society of Anesthesiologists physical status, Brinkman index, or preoperative respiratory function between the groups (Table 1). As for intraoperative data, no significant differences were seen in regard to operative time, one-lung ventilation time, anesthesia time, amount of blood loss, or amount of blood transfusion (Table 2). In contrast, the P/F ratio during one-lung ventilation was significantly higher in the prone position in comparison with the lateral position (379 vs. 297, p = 0.017), while maximum intraoperative PaCO2 was higher in the prone position group (72.2 vs. 48.3 mmHg, p < 0.001). There were no significant differences in regard to clinical laboratory data obtained on postoperative days 0, 1, 2, and 3 (Table 3).
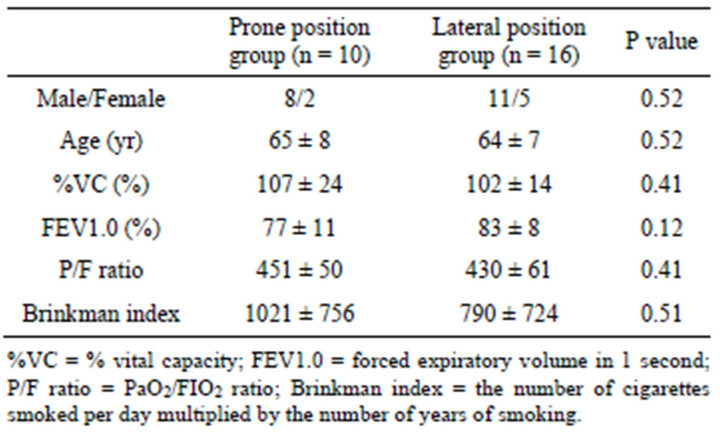
Table 1. Preoperative data.
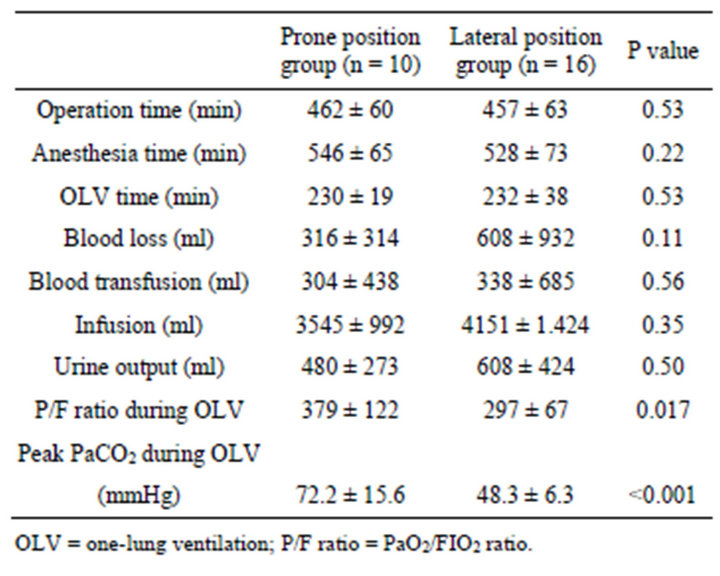
Table 2. Intraoperative data.
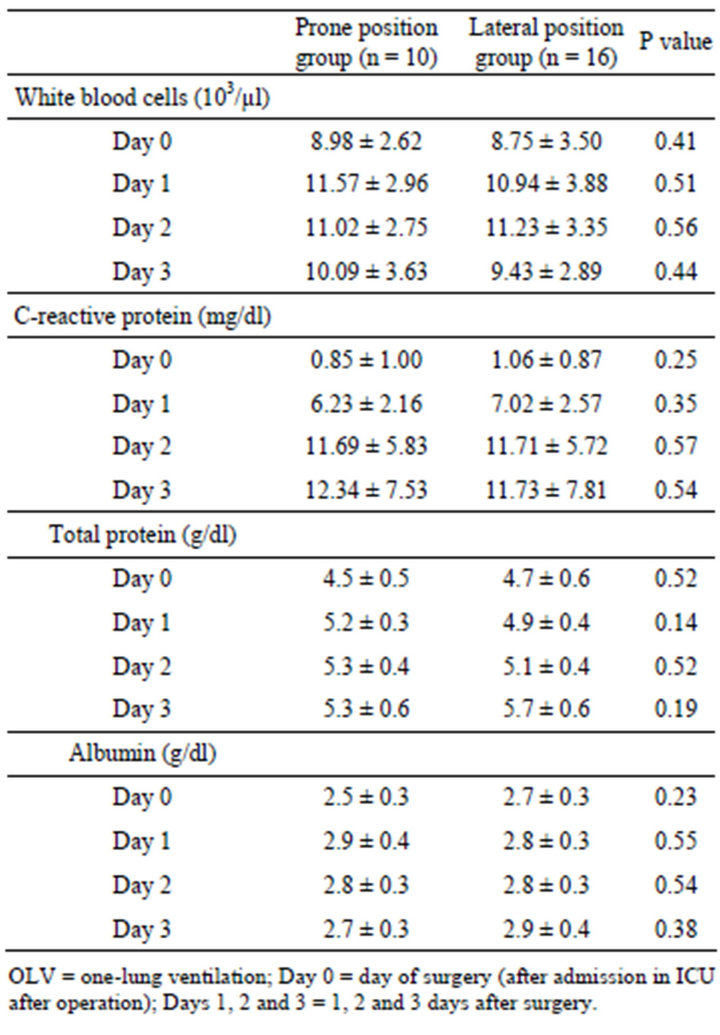
Table 3. Postoperative data.
5. Discussion
A thoracoscopic esophagectomy procedure has been shown to be less invasive as compared with a thoracotomy due to a smaller reduction in postoperative respiratory function [6] and lower levels of cytokines (IL-6 and IL-8) in blood [7], while it has also been shown to be not inferior to that procedure in regard to radical lymph node dissection [8]. However, when a lateral approach is employed, the thoracoscopic view is often obscured by both the overlying lung and a small amount of pooled blood, resulting in frequent changes of operative instruments. On the other hand, the prone position is considered to provide a better view due to both downward movement of the lung by gravity and exclusion of the lung by use of a concomitant CO2 pneumothorax procedure, thus enabling a lower frequency of instrument changes [2].
As shown in the present study, hypercapnia is inevitable in the prone position when a CO2 pneumothorax procedure is concomitantly performed. However, since pulmonary oxygenation capacity during one-lung ventilation was significantly higher in the prone position group, that position is considered to be advantageous for oxygenation. We consider that surgery done in the prone position has a potentially reduced risk of postoperative respiratory complications and is a promising method, as long as hypercapnia is controllable within a tolerable range (pH > 7.25, PaCO2 < 70 mmHg) along with transient bilateral lung ventilation.
Although operative time in the prone position was shorter as compared with the lateral position in a previous study [5], no difference in operative time was observed between the groups in our study. Along with accumulation of additional experience with the prone method, its lower level of invasiveness may be reinforced by a shorter operative time.
The present study has some limitations. The number of patients was relatively small and they were not randomized for grouping, thus a large randomized controlled trial is necessary. As for postoperative course, we obtained clinical laboratory data only during the early period following surgery. Additional investigation of postoperative courses of treated patients may better reveal the degree of invasiveness of a thoracoscopic esophagectomy in the prone position performed with a pneumothorax procedure.
In summary, we compared intraoperative findings and postoperative courses between patients who underwent a thoracoscopic esophagectomy in the prone position with a concomitant pneumothorax procedure and those who underwent that esophagectomy in a lateral position. The prone position was shown to be more advantageous for oxygenation and is a promising method to reduce postoperative respiratory complications.
REFERENCES
- J. D. Luketich, M. Alvelo-Rivera, P. O. Buenaventura, et al., “Minimally Invasive Esophagectomy: Outcomes in 222 Patients,” Annals of Surgery, Vol. 238, 2003, pp. 486- 494. doi:10.1097/01.sla.0000089858.40725.68
- T. Fabian, A. A. McKelvey, M. S. Kent and J. A. Federico, “Prone Thoracoscopic Esophageal Mobilization for Minimally Invasive Esophagectomy,” Surgical Endoscopy, Vol. 21, 2007, pp. 1667-1670. doi:10.1007/s00464-007-9193-0
- A. Cuschieri, “Thoracoscopic Subtotal Oesophagectomy,” Endoscopic Surgery & Allied Technologies, Vol. 2, 1994, pp. 21-25.
- C. Palanivelu, A. Prakash, R. Senthilkumar R, et al., “Minimally Invasive Esophagectomy: Thoracoscopic Mobilization of the Esophagus and Mediastinal Lymphadenectomy in Prone Position-Experience of 130 Patients,” Journal of the American College of Surgeons, Vol. 203, 2006, pp. 7-16. doi:10.1016/j.jamcollsurg.2006.03.016
- T. Fabian, J. Martin, M. Katigbak, A. A. McKelvey and J. A. Federico, “Thoracoscopic Esophageal Mobilization during Minimally Invasive Esophagectomy: A Head-to-Head Comparison of Prone versus Decubitus Positions,” Surgical Endoscopy, Vol. 22, 2008, pp. 2485-2491. doi:10.1007/s00464-008-9799-x
- T. Akaishi, I. Kaneda, N. Higuchi, et al., “Thoracoscopic en Bloc Total Esophagectomy with Radical Mediastinal Lymphadenectomy,” Journal of Thoracic and Cardiovascular Surgery, Vol. 112, 1996, pp. 1533-1540. http://dx.doi.org/10.1016/S0022-5223(96)70012-0
- T. Fukunaga, A. Kidokoro, M. Fukunaga, K. Nagakari, M. Suda and S. Yoshikawa, “Kinetics of Cytokines and PMNE in Thoracoscopic Esophagectomy,” Surgical Endoscopy, Vol. 15, 2001, pp. 1484-1487. doi:10.1007/s00464-001-0039-x
- H. Osugi, M. Takemura, M. Higashino, N. Takada, S. Lee and H. Kinoshita, “A Comparison of Video-Assisted Thoracoscopic Oesophagectomy and Radical Lymph Node Dissection for Squamous Cell Cancer of the Oesophagus with Open Operation,” British Journal of Surgery, Vol. 90, 2003, pp. 108-113. doi:10.1002/bjs.4022
NOTES
*Declaration: The contents of this manuscript have not been published nor are being submitted elsewhere. The final version of the study has been read and approved by all co-authors.
#Corresponding author.

