Open Journal of Anesthesiology
Vol.3 No.4(2013), Article ID:32565,4 pages DOI:10.4236/ojanes.2013.34053
Comparison of Postoperative Throat and Neck Complaints after the Use of the i-Gel versus the Traditional Laryngeal Mask
![]()
1Anesthesiologist at Hospital del Niño, Panama City, Panama; 2Anesthesiologist at Hospital Santo Tomás, Panama City, Panama.
Email: anasofia113@gmail.com
Copyright © 2013 Ana Sofía Del Castillo Sardi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 11th, 2013; revised April 20th, 2012; accepted May 15th, 2013
Keywords: i-Gel; Laryngeal Mask; Cervical Pain; Sore Throat
ABSTRACT
Introduction: One of the most important jobs of an anesthesiology is to preserve an adequate gaseous exchange. With the coming in the 80’s of the laryngeal mask airway, a less invasive technique was introduced for this end. There are a lot of variants of these supraglotic issues, being the i-gel a no inflate mask; witch principle is to provide a perilaryngel stamp that reduced the incidence of sore throat, cervical pain compared with the traditional laryngeal mask. Method: A group of 121 ASA I-II patients with general anesthesia administration, where divided in two groups, one of 60 patients where a traditional laryngeal mask airway was used, and a second group of 61 patients where an i-gel mask was used. In both groups the presence of postoperative sore throat, cervical pain and dysphonia; number of attempts and pressure in the airway tract was measured. Results: The group of patients where the i-gel was used present lower incidence of sore throat (11% vs 27%) and cervical pain (3% vs 9%) and lower values of pressure on the airway tract compared with the group in which the conventional laryngeal mask was used. On the other hand there was no difference in the presence of dysphonia, trauma or number of attempts used to insert the mask. Conclusions: The i-gel larygeal mask demonstrated to be a safe issue, with low incidence of morbidity to administrated general anesthesia.
1. Introduction
One of the essential job of the anesthesiologist is to keep an adequate gas interchange; and guarantee a permeable airway. To achieve purpose is necessary for the knowledge if the airway anatomy and the different ways to approach it.
In the 80’s with the invention of the Dr. Charlie Brain; the laryngeal mask appears as an easy, safe and less invasive technique to the access and keeping of the airway; being now an indispensable device to the anesthesiologist.
Although in medical literature is registered the safety and efficiency when the laryngeal mask is used; it’s not exempt of complications. Example of these complications is the present of postoperative odynophagia and cervical pain, [1-3] with an incidence from 5.8% to 42% for the first one and 15% to 20% to the second one. Other frequent complications are dysphonia and mouth and laryngeal trauma [4-6].
The i-gel is a new single use, supraglotic not inflate device; with a peri-laryngel stamp that is designed to reduced the incidence of postoperative odinophagia and cervical pain.
The following article evaluated the safety and the incidence of complications using the i-gel versus the conventional laryngeal mask.
2. Method
After institutional ethical approval and informed consent of each patient was obtained, 121 ASA I-II patients scheduled for elective procedure in which general anesthesia with a laryngeal mask was going to be performed were enrolled in this prospective, randomized simple blind study.
The calculation of the required sample was using as the universe the total general anesthesia performed with a supraglotic device in the Santo Tomas Hospital for the 2009 elective year. Exclusion criteria were:
• Patients with neck, airway or digestive tract pathology;
• Corporal mass index > 35 kg/m2;
• Patients with sleep obstructive apnea history;
• Full stomach patients;
• Patients with gastroeshophagical reflux.
All the patients were premedicated with 2 mg of midazolam iv; after pre-oxygenation, the anesthetic induction was performed with fentanyl 1 μg/kg I.V. and propofol (2 - 2.5 mg/kg) I.V. The anesthesia maintenance was with oxygen, air and sevoflurane. Then the anesthesiologist of the case decided if spontaneous breathing or mechanical ventilation (no more than 8 mL/kg and respiratory rate of 12 - 14) was assigned to each patient using his criteria.
Using simple aleathorization the patients were assigned to two groups:
• Group A: A lubricated conventional laryngeal mask according to the patient weight was inserted with the forefinger after the mandible was opened. The cuff was inflated according to the LMA size and the intracuff pressure was measure with a calibrated aneroid manometer (Carrón médica® instrumental control RSA), to guarantee it was less than 40 mmHg.
• Group B: A lubricated i-gel laryngeal mask according to the patient weigh was inserted.
The perioperative monitoring for both groups was with: electrocardiogram, pulse oximetry, noninvasive arterial pressure and capnography. The anesthesiologist of the case report the number of attempt necessary to insert the supraglotic device and the airway pressures managed during the procedure.
After the surgery was performed, the patients were lead to the post-anesthetic unit, where two hours later, a trained nurse that didn’t know which supraglotic device was inserted to the patient ask him about the present of odynophagia, cervical pain, disphonya and inspect the presence of laryngeal or mouth trauma.
The result of the incidence of each complication was registered. The comparisons between two qualitative variables were performed with the Pearson’s chi-square test. A p value < 0.05 was considered to be statistically significant. For those cases were the p value < 0.05, the number need to threat (NNT) was calculated.
3. Results
A total of 60 patients were assigned to the group A (conventional laryngeal mask) and 61 patients were assigned to the group B (i-gel laryngeal mask). Most of the patients of the study were young women in both groups (Tables 1 and 2). Both devices have high rate of success at the first attempt (Table 3) and the conventional LMA manage superior airway pressures that the i-gel LMA (Table 4). The most common complication for both groups was odynophagia; and the less common was dysphonia. When the Pearson’s chi-square test was applied to compare the qualitative values between the conventional LMA and the i-gel LMA we found that the i-gel LMA present less odynophagia, cervical pain and airway pressure than the conventional LMA. The Number Need to Treat (NNT) for these variables were lower than ten (Table 5).
4. Discussion
The laryngeal was designed to create a device more practical than the facial mask, but less penetrating that the tracheal cannula. Since its development in 1981 by the British anesthesiologist Dr. Archie Brain in the Royal London Hospital Whitecjaple as a modified device of the dental Goldman mask [7], the laryngeal mask has earn more followers than detractors in all the anesthesia services of the great centers of the world [8].
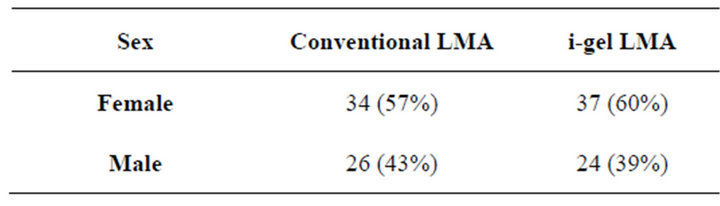
Table 1. Distribution by sex.
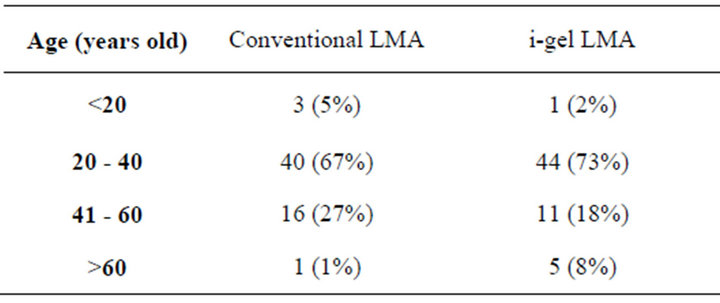
Table 2. Distribution by age.
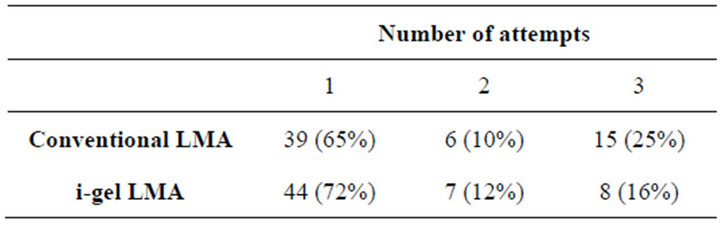
Table 3. Distribution by number of attempts.
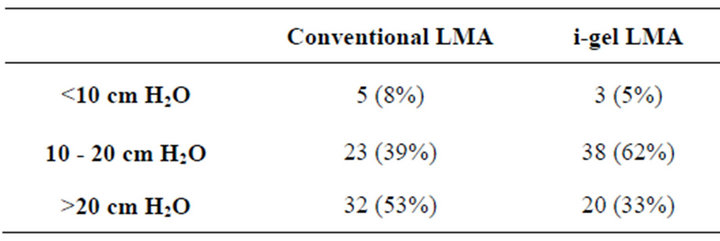
Table 4. Distribution by airway pressure.
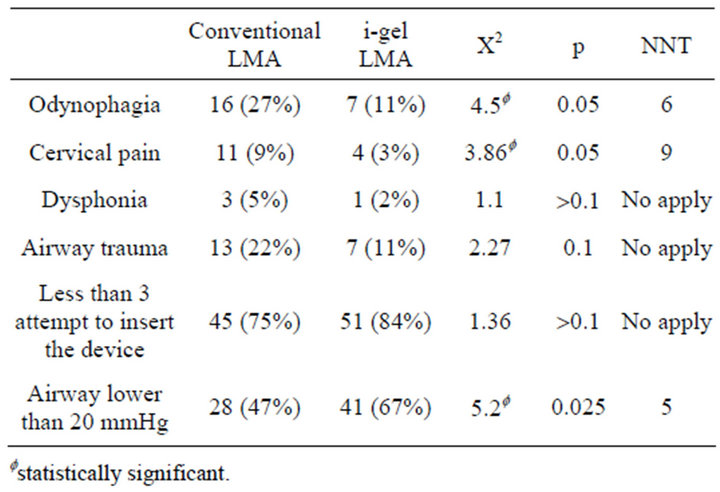
Table 5. Complications observed in the groups.
The laryngeal mask was throw to the Great England market in 1988 and 12 months later, is was used in more than 500 hospitals. Nowadays it has become a first line device to the administration of general anesthesia and incorporated to the difficult airway algorithm [9,10].
As all the medical devices, the laryngeal mask also has complications. The more common are: odynophagia (5%, 8% to 42%), cervical pain, dysphonia (15% to 20%) and mouth and laryngeal trauma. A very rare complication mentioned in the literature is the theoretical risk of ischemia of the pharyngeal mucosa produce by the pressure of the mask over it, it can be avoid keeping pressure values under the los 35 ± 20 cm H2O or 44 mmHg; which is the perfusion pressure of the pharynx capillaries [11-15].
The i-gel laryngeal mask is a supraglotic device made with a soft and transparent thermoplastic elastomeric gel kind [9,16]. This LMA was designed to create an anatomic stamp without the need of the fill of the pharynx, laryngeal and perilaryngeal structures. The strength of the tube section and its natural oropharyngeal curvature allows that the cannula to be inserted using its proximal edge, without the introduction of the fingers and through the rigid palate, pharynx and hipopharynx [16-18].
Several studies have validated the efficacy and safely of the i-gel LMA [7,19,20], reporting high successful insertion rate at the first attempt, with acceptable mean airway pressure, and low incidence of complications.
In our study in both group the cases were young women; because most of the procedures in our hospital that used general anesthesia with LMA are Gynecology and Obstetrics procedures, preferring regional anesthesia for patients over the 60 years old. The global incidence of odynophagia reported in this study was 38%; coherent with the international publications (5.8% to 42%). Our global incidence of cervical pain (12%) and dysphonia (7%) was slightly lower than the literature reports (15% for cervical pain and 12% for dysphonia) [4-6].
When we compared de incidence of complications between the traditional laryngeal mask versus the i-gel laryngeal mask we found less odynophagia, cervical pain and lower airway pressures in the i-gel LMA group. We didn’t found different between the groups in dysphonia, airway trauma and number of attempts to insert the device. Cristiaan Keijzer et al. [1] also found in a study with 118 patients less odynophagia and cervical pain in the group using the i-gel LMA versus the traditional LMA, although Keizjer found larger differences than in our study, in the presence of odynophagia between the groups. (6% versus 32% in Keizjer study; 11% versus 27% in our study).When the NNT was calculated we found values under 10, a good result for clinical experience.
5. Conclusion
The i-gel LMA demonstrated to be a confiable and safe supraglotic device for the administration of general anesthesia, presenting a good profile to decrease important complications like the postoperative odynophagia and cervical pain.
REFERENCES
- C. Keizger, et al., “A Comparison of Postoperative Throat and Neck Complaints after the Use of the i-Gel and the La Premiere Disposable Laryngeal Mask: A DoubleBlinded, Randomized, Controlled Trial,” Anesthesia and Analgesia, Vol. 109, No. 4, 2009, pp. 1092-1095. doi:10.1213/ANE.0b013e3181b6496a
- P. P. Higgins, F. Chung and G. Mezei, “Postoperative Sore Throat after Ambulatory Surgery,” British Journal of Anaesthesia, Vol. 88, No. 4, 2002, pp. 582-584. doi:10.1093/bja/88.4.582
- L. G. Theiler, et al., “Crossover Comparison of the Laryngeal Mask Supreme™ and the i-gel™ in Simulated Difficult Airway Scenario in Anesthetized Patients,” Anesthesiology, Vol. 111, No. 1, 2009, pp. 55-62. doi:10.1097/ALN.0b013e3181a4c6b9
- R. M. Levitan and W. C. Kinkle, “Initial Anatomic Investigations of the i-Gel Airway: A Novel Supraglottic Airway without Inflatable Cuff,” Anaesthesia, Vol. 60, No. 10, 2005, pp. 1022-1026. doi:10.1111/j.1365-2044.2005.04258.x
- A. M. Cross, R. Pitti, C. Concil, D. Giraud, et al., “Severe Dysphonia after Use of Laryngeal Mask Airway,” Anesthesiology, Vol. 86, No. 2, 1997, pp. 498-500. doi:10.1097/00000542-199702000-00027
- J. Brimacombe and C. Keller, “Recurrent Laryngeal Nerve Injury with the Laryngeal Mask,” Anästhesiol Intensivmed Notfallmed Schmerzther, Vol. 34, No. 3, 1999, pp. 189-192. doi:10.1055/s-1999-176
- B. Richez, et al., “A New Single Use Supraglottic Airway Device with a Noninflatable Cuff and an Esophageal Vent: An Observational Study of the i-Gel,” Anesthesia & Analgesia, Vol. 106, No. 4, 2008, pp. 1137-1139. doi:10.1213/ane.0b013e318164f062
- N. M. Wharton, B. Gibbison, D. A. Gabbott, G. M. Haslam, et al., “i-Gel Insertion by Novices in Manikins and Patients,” Anaesthesia, Vol. 63, No. 9, 2008, pp. 991-995. doi:10.1111/j.1365-2044.2008.05542.x
- I. Cordero, “Estado Actual del Arte de la mÁscara Laríngea,” Revista Cubana de Anestesiología y Reanimación, Vol. 3, No. 3, 2004, pp. 43-46.
- M. Emmerich and R. Dummler, “Use of the i-Gel Laryngeal Mask for Management of a Difficult Airway,” Anaesthesist, Vol. 57, No. 8, 2008, pp. 779-781. doi:10.1007/s00101-008-1386-y
- J. Brimacombe, C. Keller, W. Roth and A. Loeckinger, “Large Cuff Volumes Impede Posterior Pharyngeal Mucosal Perfusion with the Laryngeal Tube Airway,” Canadian Journal of Anesthesia, Vol. 49, No. 10, 2002, pp. 1084-1087.
- J. Brimacombe and C. Keller, “A Comparison of Pharyngeal Mucosal Pressure and Airway Sealing Pressure with the Laryngeal Mask Airway in Anesthetized Adult Patients,” Anesthesia & Analgesia, Vol. 87, No. 6, 1998, pp. 1379-1382.
- A. Rieger, B. Brunne and H. W. Striebel, “Intracuff Pressures Do Not Predict Laryngopharyngeal Discomfort after Use of the Laryngeal Mask Airway,” Anesthesiology, Vol. 87, No. 1, 1997, pp. 63-67. doi:10.1097/00000542-199707000-00009
- E. Figueredo, M. Vivar-Diago and F. Munoz-Blanco, “Laryngopharyngea Complaints after Use of Laryngeal Mask Airway,” Journal of Clinical Anesthesia, Vol. 9, No. 1, 1997, pp. 42-47. doi:10.1016/S0952-8180(96)00209-7
- E. Seet, “Use of Manometry for Laryngeal Mask Airway Reduces Postoperative Pharyngolaryngeal Adverse Events,” Anesthesiology, Vol. 112, No. 3, 2010, pp. 652-657. doi:10.1097/ALN.0b013e3181cf4346
- C. A. Hagberg, “Comparison of i-Gel to the Laryngeal Mask Airway (i-Gel),” Clinical Trials Government, The University of Texas Health Science Center, Houston, 2008.
- P. Michalek, “A Comparison of the i-Gel Supraglottic Airway as a Conduit for Tracheal Intubation with the Intubating Laryngeal Mask Airway,” Resuscitation, Vol. 81, No. 1, 2009, pp. 74-77.
- D. Gabbott and R. Beringer, “The i-Gel™ Supraglottic Airway: A Potential Role for Resuscitation?” Resuscitation, Vol. 73, No. 1, 2007, pp. 161-162. doi:10.1016/j.resuscitation.2006.10.026
- M. R. Nott, P. D. Noble, et al., “Reducing the Incidence of Sore Throat with the Laryngeal Mask Airway,” European Journal of Anaesthesiology, Vol. 15, No. 2, 1998, pp. 153-157.
- J. Brimacombe, C. Keller and F. Puerhringer, “A Fibreoptic Evaluation of the Posterior Pharynx in Anesthetized Adult Patients with a Modified Cuffed Oropharyngeal Airway,” Anesthesiology, Vol. 91, No. 6, 1999, pp. 1661- 1665. doi:10.1097/00000542-199912000-00018

