Open Journal of Obstetrics and Gynecology
Vol.4 No.7(2014), Article ID:46319,4 pages DOI:10.4236/ojog.2014.47056
Late Presentation of Acardiac Twin: A Case Report and Review of Literature
Marieke den Hartog1,2*, Toon Toolenaar1, Yves Jacquemyn3
1Department of Obstetrics and Gynecology, Albert Schweitzer Hospital, Dordrecht, The Netherlands
2Department of Obstetrics and Gynecology, Van Weel Bethesda Hospital, Dirksland, The Netherlands
3Department of Obstetrics and Gynecology Antwerp University Hospital, Antwerp, Belgium
Email: *marieke_den_hartog@hotmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 3 April 2014; revised 2 May 2014; accepted 9 May 2014
ABSTRACT
Acardiac twinning or TRAP-sequence is a rare complication of monochorionic twin pregnancy. We present a case in which fetal demise of one fetus of a twin pregnancy had been wrongly diagnosed in the first trimester as a vanishing twin. This resulted in the unexpected occurrence of an acardiac twin in the third trimester, culminating in an acardiac twin with a birth weight higher than that of the normal twin. A review is presented on therapeutic opportunities including ligation of the umbilical cord under ultrasound or fetoscopy. This case report highlights the need for correct and early ultrasonographic diagnosis of chorionicity and detailed ultrasonographic follow-up of twin pregnancies.
Keywords:Acardiac Twin, Twin Reversed Arterial Perfusion Sequence, Monochorionic Twin Pregnancy, Ultrasound

1. Introduction
Acardiac twinning or twin reversed arterial perfusion sequence (TRAP-sequence) is a rare complication of monochorionic twin pregnancies eventually threatening survival of the normal twin. An acardiac twin has no functional own heart and blood circulation is supported through placenta anastomosis by the other surviving twin.
2. Case Report
A 24-year-old G1 P0 without any relevant medical history was first seen at 8 weeks gestational age for an early pregnancy ultrasound at a primary care center. A twin pregnancy was noted with one amorphic embryo without heart activity compacted in the uterine fundus, the surviving embryo had a crown-rump length of 19 mm, in accordance with 8 weeks gestational age. The status was diagnosed as diamniotic twin pregnancy with early demise of one embryo. Follow-up was organized at the primary care center with routine structural ultrasound at 20 weeks, at that moment no anomalies had been noted. At 27 weeks, still at the primary care center, intrauterine growth retardation was suspected and the patient was referred for specialist care. The patient was followed by weekly ultrasound and home cardiotocography. At 34 weeks, a fetus in breech presentation was noted, biometry was in accordance with 31 weeks and an expected fetal weight of 1800 grams, a hydropic placenta was noted and the patient was sent to a tertiary care center where a perinatal specialist performed a third level ultrasound. A second amorphic fetus without cardiac action, a length of about 18 cm, was seen that had mistakenly been regarded as a hydropic placenta. At that moment, the diagnosis of acardiac twinning was made. It was decided to follow the pregnancy by further intensive monitoring of the surviving fetus and looking for eventual signs of cardiac decompensation. Due to suspected large volume of the acardiac twin, primary caesarean section was planned.
At 35 weeks and 4 days, the patient presented herself with spontaneous rupture of membranes and preterm labour. A caesarean section was performed. First the surviving fetus was delivered in breech presentation, male weighing 1855 grams. Apgar score of 8 after 1 minute and of 9 after 5 minutes, umbilical artery pH 7.21. The baby was transferred to the neonatology department. Further development and extraction of the acardiac twin posed some technical problems due to the large volume. Only after ten minutes, the acardiac twin was born, and weight was 1940 grams. The acardiac twin had no head, only a rump and severely malformed limbs (Figure 1). Examination of the placenta demonstrated vascular connections between donor and acceptor.
Autopsy of the acardiac twin confirmed the absence of cardiac and pulmonary tissues. There was a rudimentary vertebral column with 5 thoracic vertebrae and some spinal cord. Diaphragm, liver, spleen and adrenals were absent. Bladder, kidneys, anus and testes were present. The intestinum was rotated and in both arms and legs, some bone formation was present.
3. Discussion
The incidence of cardiac twinning is about 1 in 35000 pregnancies or 1% of all monochorionic twins [1] -[7] . In the Netherlands, this constitutes 6 to 20 acardiac twins per year [1] . An acardiac is always severely malformed and never has a functioning heart, blood flow is supported through placental anastomosis by the other fetus called pump twin [1] [2] . Acardiac twinning is also called TRAP-sequence (twin reversed arterial perfusion). More or less large arterial anastomoses on the placental surface pump oxygen-poor blood from the donor twin to the acardiac twin mean that the direction of blood flow in the umbilical cord of the acardiac is reversed as compared to normal. Blood flow is from the acardiac twin back to the donor twin through veno-venous anastomosis. The acardiac twin can be considered a parasite with some tissues surviving due to the cardiac function of the donor. It is often noted that the lower half of the body is better developed as the oxygen-poor blood from the
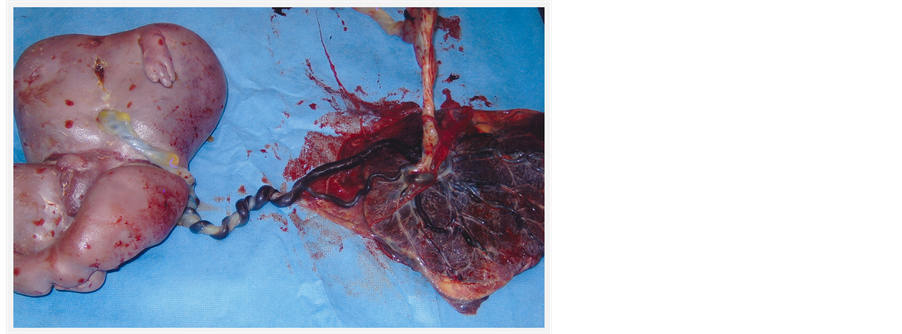
Figure 1. Examination of the placenta demonstrated vascular connections between donor and acceptor.
umbilical artery and aorta from the acardiac first supplies the lower part and is almost completely depleted of oxygen when it reaches head, heart and arms. In general, a diagnosis can be made early with ultrasound, and doppler measurements will show retrograde flow in the umbilical arterial of the acardiac [3] -[6] . Our case demonstrates that missing the diagnosis early in the pregnancy can result in both diagnostic and therapeutic difficulties later in the pregnancy. The exact etiology is not completely clear. One hypothesis is that primary cardiac failure at the stage of embryogenesis is present, resulting in an acardiac twin surviving as a parasite on the pump twin from early beginning. Another theory states that the unbalance between both fetal circulations results in cardiac atrophy in the acardiac twin and secondary abnormal anatomy. Unfavorable prognostic factors for the surviving twin are a relatively high weight of the acardiac (particularly when this is more than 70% of the donor twin), a quickly developing acardiac mass and some morphological features such as a developing head and upper limbs [1] [3] [5] -[7] . A high resistance index in the umbilical artery of the acardiac twin is considered favorable. Possible complications for the surviving pump twin are cardiac failure, polyhydramnios, preterm birth, intrauterine fetal death (in up to 25% of cases), perinatal death (in 35 to 50% of cases), due to cardiac failure and hypoxemia [1] -[5] .
Historically, uterotomy and removal of the acardiac twin has been described [1] . Later, endoscopic ligation of the umbilical artery and fetoscopic coagulation or ablation of the placental anastomosis have been described [1] -[3] [5] -[7] . Fetal survival after laser coagulation is around 76%, mean gestational age at birth is 34 weeks and the failure rate is about 10%. There is a high risk for preterm rupture of the membranes resulting in preterm or immature birth (up to 10%). Intrafetal ablation is technically easier and safer and more effective in comparison to more invasive techniques for umbilical artery occlusion [3] . Intrafetal ablation has been described by alcohol injections, monopolar diathermy, ultrasound guided laser and radiofrequency [3] . The most recent development is percutaneous ablation of the acardiac through radiofrequency. This is an effective way to treat TRAP-sequence but does not prevent eventual knotting of umbilical cords [2] . Neonatal survival after this treatment is between 80 and 88% and the mean gestational age at delivery is 36 weeks [2] [4] . Recently, high intensity focused ultrasound (HIFU) has been described as a non-invasive treatment for occlusion of the blood flow in the acardiac twin [8] . No comparative studies with HIFU exist.
As pregnancy progresses, interventions become more and more difficult due to the enlarging diameter of the blood vessels. The optimal timing for treatment seems to be between 16 and 20 weeks gestational age [3] . This necessitates early diagnosis and referral to a specialist centre. Due to the low incidence of this specific complication in twin pregnancies, early referral for detailed ultrasound in twin pregnancy should be advised to avoid missing the diagnosis, as demonstrated by this case.
A non-invasive option is close observation with frequent ultrasound and termination of pregnancy as soon as the surviving twin shows signs of heart failure [1] [4] [6] [7] .
4. Conclusion
This case demonstrates the importance of correct early diagnosis of acardiac twinning to avoid later complications. Referring every twin pregnancy for a detailed early ultrasound to a specialist center can avoid diagnostic and therapeutic difficulties later in the pregnancy. Probably the late diagnosis resulting in the enormous volume of the acardiac twin in our case is due to the misdiagnosis at the first ultrasound. Centralization for specialized ultrasound in case of twin pregnancies could possibly prevent this kind of late diagnosis.
References
- Vandenbussche, F.P.H.A., Deprest J.A., Klumper, F.J.C.M., Vandenbroucke, W.V.A., Sollie, K.M. and Kanhai, H.H.H. (2003) Minimaal invasieve intra-uteriene chirurgische behandeling bij vier monochoriale tweelingzwangerschappen gecompliceerd door een acardiacus. Nederlands Tijdschrift voor Geneeskunde, 147, 931-936.
- Lee, H., Bebbington, M. and Crombleholme, T.M. (2013) The North American Fetal Therapy Network Registry Data on Outcomes of Radiofrequency Ablation for Twin-Reversed Arterial Perfusion Sequence. Fetal Diagnosis and Therapy, 33, 224-229. http://dx.doi.org/10.1159/000343223
- Tan, T.Y.T. and Sepulveda, W. (2003) Acardiac Twin: A Systematic Review of Minimally Invasive Treatment Modalities. Ultrasound in Obstetrics & Gynecology, 22, 409-419. http://dx.doi.org/10.1002/uog.224
- Lewi, L., Valencia, C., Gonzalez, E., Deprest, J. and Nicolaides, K.H. (2010) The Outcome of Twin Reversed Arterial Perfusion Sequence Diagnosed in the First Trimester. American Journal of Obstetrics & Gynecology, 203, e1-e4.
- Prasad, R.H.S., Prasad, T.R. and Kumar, K.D. (2012) TRAP-Sequence—An Interesting Entity in Twins. Journal of Clinical Imaging Science, 2, 56. http://dx.doi.org/10.4103/2156-7514.100997
- Hartge, D.R. and Weichert, J. (2012) Prenatal Diagnosis and Outcome of Multiple Pregnancies with Reversed Arterial Perfusion (TRAP-Sequence). Archives of Gynecology and Obstetrics, 286, 81-88. http://dx.doi.org/10.1007/s00404-012-2283-9
- Sullivan, A.E., Varner, M.W., Ball, R.H., Jackson, M. and Silver, R.M. (2003) The Management of Acardiac Twins: A Conservative Approach. American Journal of Obstetrics & Gynecology, 189, 1310-1313. http://dx.doi.org/10.1067/S0002-9378(03)00597-0
NOTES

*Corresponding author.

