Open Journal of Immunology
Vol.3 No.1(2013), Article ID:28677,4 pages DOI:10.4236/oji.2013.31006
Thyroid autoimmunity at the onset of type 1 diabetes mellitus in children
![]()
1Pediatric Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran *Corresponding Author: azimrezamand@yahoo.com
2Tabriz University of Medical Sciences, Tabriz, Iran
Received 19 November 2012; revised 24 December 2012; accepted 16 January 2013
Keywords: Newly Diagnosed Diabetes; Autoimmune Thyroid Disease; Children
ABSTRACT
Introduction: Studies that have investigated autoimmune thyroid disease in newly diagnosed type 1 diabetic children are few and reported prevalence rate ranges between 4.5 - 29.4 percent. Considering the effect of age, ethnic origin, and disease duration on the prevalence of autoimmune thyroid disease in diabetic subjects, we decided to investigate the thyroid autoimmunity in newly diagnosed type 1 diabetic children in our area of residence (North-West Iran). Methods: This cross-sectional study was carried out between 2008 and 2010. All of the children with newly diagnosed type 1 diabetes mellitus (T1DM) presenting to the outpatient pediatric-endocrinology clinic of Tabriz University of Medical Sciences (the only university-affiliated clinic for pediatric-endocrinology in North-west Iran), were investigated for serum levels of antiTPO, anti-Tg and TSH. Results: The study group included 99 children [mean age 7.75 ± 3.21 years (range 1.2 - 14), 45 boys (45.5%) and 54 girls (54.5%)]. About 9% of patients were seropositive for anti thyroid antibodies and females were affected more than males. The mean TSH level of subjects above 12 years of age (3.5 ± 2) was significantly (p = 0.037) higher than those below this age. Conclusion: Autoimmune thyroid disease and even hypothyroidism may accompany T1DM at its presenting time in children. This finding is more common in girls especially those above 12 years of age.
1. INTRODUCTION
Type 1 diabetes mellitus (T1DM) is an autoimmune disorder that results from immune destruction of pancreatic beta cells [1]. Because of the autoimmune nature of this disorder it can be associated with other autoimmune disease, for example pernicious anemia with hemoglobin level less than 10.5 g/dl [2]. Autoimmune thyroid disease (ATD) is the most frequent autoimmune disease associated with T1DM [3]. Prevalence of ATD determined by high anti-TPO and/or anti-TG titers in diabetic population is considerably higher than general population and varies depending on the age, sex and ethnic origin of the subjects and increases with duration of the disease [4-6]. Studies have showed a great variation in the prevalence of anti-thyroid antibodies in children with T1DM. There is no consensus regarding screening of ATD in patients with T1DM, especially in asymptomatic patients [4]. The prevalence of positive thyroid antibodies in children with T1DM varies between 3% and 54.3% in different countries [7,8]. The author’s previous study on thyroid autoimmunity in diabetic children and adolescents (mean age of 8.3 ± 3.7 years and mean diabetes duration of 1.6 ± 2.5 years), showed medium prevalence rate in Iranian subjects compared with those of other countries [9]. Studies that have investigated ATD in newly diagnosed type 1 diabetic children are few and reported prevalence rate ranges between 4.5 - 29.4 percents [10,11]. Considering the effect of age, ethnic origin, and disease duration on the prevalence of ATD in diabetic subjects, we decided to investigate the thyroid auto-antibodies and thyroid stimulating hormone (TSH) level in newly diagnosed type 1 diabetic children in our area of residence (North-West Iran). As previous studies reported a wide variations in the prevalence of ATD in new onset T1DM in children (between 4.5% and 29.4%), it is necessary to investigate this subject in any geographical areas and ethnic groups [5,11].
2. METHODS
This cross-sectional study was carried out between 2008 and 2010. All of the children with newly diagnosed T1DM presenting to the outpatient pediatric-endocrinology clinic of Tabriz University of Medical Sciences (the only university-affiliated clinic for pediatric-endocrinology in North-west Iran), were included. 99 patients, all newly diagnosed with T1DM were studied; which included 45 boys and 54 girls. The study protocol was approved by Ethic Committee and Research Vice Chancellor Office of Tabriz University of Medical Sciences.
Laboratory tests: Written informed consents were taken and blood samples were collected to assay the antiTPO, anti-Tg and serum thyrotropin (TSH) levels. The Diagnostics® thyroglobulin IgG ELISA kit and thyroid-peroxidase IgG ELISA kit (GENESIS, Cambridge, UK) used for evaluation of serum levels of anti-Tg and anti-TPO antibodies respectively. Values above 75 U/ml for anti-TPO and above 100 IU/ml for anti-Tg were considered positive and either one or both positive antibody level(s) were considered diagnostic for ATD. The AccuBindTM ELISA Microwells kit (MONOBIND, Costa Mesa, USA) was used for measurement of serum TSH level. The normal TSH level as determined by the instruction of this kit is 0.4 - 6.21 micIU/ml.
Statistical analysis: The data were analyzed using SP SS version 16 for windows software package. Statistical procedures used to analyze the data included Chisquare test, T-test and Pearson’s correlation. Quantitative variables are presented as mean ± SD and qualitative variables as percent. Differences between groups were considered significant when p < 0.05.
3. RESULTS
The study group included 99 children with newly diagnosed T1DM [mean age 7.75 ± 3.21 years (range 1.2- 14), 45 boys (45.5%) and 54 girls (54.5%)]. Difference between the mean age of males (7 ± 3.4) and females (8.3 ± 2.9) were significant (p = 0.042).
Table 1 shows the frequency of seropositive state for ATD regarding gender of the patients and Table 2 shows the age distribution of them and frequency of seropositive state for ATD, in different age groups.
As the tables show, about 9% of newly diagnosed type 1 diabetic children are seropositive for ATD and females are affected more than males.
Mean age of antibody positive group was 8.9 ± 4 and mean age of antibody negative group was 7.5 ± 3 (p = 0.226). Considering the age groups (<5, 5 - 10, and >10 years of old), although the difference between groups was not statistically significant, but half of the children above 12 years (4 out of 8) were seropositive and the difference was significant (p = 0.001). Five cases (M/F = 1/4) were seropositive for both anti-TPO and anti-TG antibodies and 3 of them were above 12 years.
The mean TSH level of patients was 2.44 ± 1.53 mic IU/ml. In one case it was above 6.2 and in another case it was above 10. Mean TSH level in seropositive and seronegative subjects was 3.31 ± 1.67 and 2.39 ± 1.52 mic IU/ml respectively (p = 0.090). The mean TSH of subjects above 12 years of age (3.5 ± 2) was significantly (p = 0.037) higher than those below this age (2.3 ± 1.4).
4. DISCUSSION
This study set out with the aim of assessing the prevalence of ATD in newly diagnosed type one diabetic children in North-West Iran. In reviewing the literatureTable 1. The frequency of seropositive state for ATD* regarding gender (N = 99).
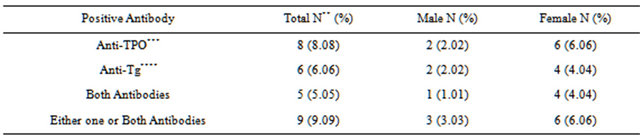
*Autoimmune thyroid disease, **Number, ***Thyroid peroxidase, ****Thyroglobulin.
Table 2. Age distribution of the patients and frequency of seropositive state for ATD, in different age groups.
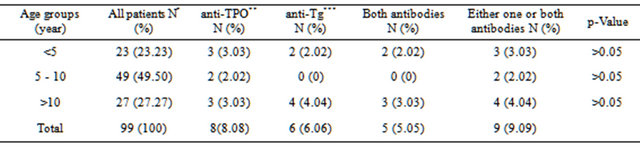
*Number, **Anti thyroid peroxidase, ***Anti thyroglobulin.
about 4.5 to 29.4% of children with newly diagnosed T1DM have positive levels of anti thyroid antibodies [5, 11]. This study found that in our area of residence, about 9% of children with T1DM have ATD at the beginning of diabetes. Another important finding was that the disorder is 2 folds more common in girls than in boys and is more prevalent in patients above 12 years of age. These findings of the current study are consistent with those of Kordonauri and et al. (2005) who found that anti-TPO in 15.4% and anti-Tg in 14.4% of children were positive at the beginning of their diabetes, which were more common in girls particularly above 12 years of age [12]. Czeniawska and et al. studied the prevalence of anti-TPO and anti-TG antibodies at the onset of T1DM in children, 17.8% of studied children had raised levels of one or both of mentioned antibodies. In that study the mean age of children with high titer of antibody was significantly more than those with negative antibody levels [13]. The least reported prevalence rate belongs to Kordonouri and et al study on 325 patients with T1DM. In that study, 15 subjects (4.5%) had anti thyroid antibody at initiation of diabetes with superiority of females [5]. Abrams and et al studied 157 subjects (10-39 years of age) with newly diagnosed T1DM, 17% had positive anti-TPO [14]. In a study from Turkey, 17.8% of patients had positive antiTPO [15]. The highest reported prevalence rate belongs to Kalicka-Kasperczyk and et al. study on 153 children (mean age 9.5 ± 3.9 years) with newly diagnosed T1DM, in which 29.4% of patients had positive anti-TPO level [11].
Regarding age and sex, this study produced results which corroborate the findings of a great deal of the previous works in this field [12,13,16-18]. However there are few studies that have shown no relation between the gender and thyroid dysfunction [17,19].
Only two of our patients (2.02%) had abnormal TSH levels, meanwhile the average of TSH in patients above 12 years of age was noticeably higher than those below this age. In Kalicka’s study on 85 girls and 68 boys with newly diagnosed T1DM (mean age 9.5 ± 3.5 years), 3.9% of patients had hypothyroidism [11]. In a Brazilian study on 214 children, teenagers and young adults with previously diagnosed T1DM , 55.5% of patients with positive anti TPO had abnormal TSH [20]. In Severinski and et al. study on diabetic children and teenagers with 12 years follow up, the mean age of ATD inception was 11.5 ± 5.2 years and average time between being diabetic and becoming hypothyroidism was 3.3 ± 2.5 years [21].
Results of current study indicate that ATD and even hypothyroidism may accompany T1DM at its presenting time in children. This finding is more common in girls especially those above 12 years of age. Because of the importance of normal thyroid function, it is advisable to investigate the ATD and hypothyroidism at the onset of T1DM in children, especially those above 12 years of age.
5. ACKNOWLEDGEMENTS
The authors acknowledge the vice chancellor office of Tabriz University of Medical Sciences and the Pediatric Health Research Center for financial support of this study.
REFERENCES
- Voltarelli, J.C., Couri, C.E.B., Stracieri, A.B.P.L., et al. (2007) Autologus nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus. Journal of the American Medical Association, 297, 1568-1576. doi:10.1001/jama.297.14.1568
- Ghorashi, Z., Nezami, N., Behbahan, A.G., et al. (2008) Supplemental food may not prevent Iron-Deficiency Anemia in infants. Indian Journal of Pediatrics, 75, 1121- 1124. doi:10.1007/s12098-008-0191-6
- Prazny, M., Skrha, J., Limonova, Z., et al. (2005) Sceening for associated autoimmunity in type 1 diabetes mellitus with respect to diabetes control. Physiological Research, 54, 41-48.
- Montovani, R.M., Montovani, L.M. and Dias, V.M. (2007) Thyroid autoimmunity in children and adolescents with type 1 diabetes mellitus: Prevalence and risk factors. Journal of Pediatric Endocrinology & Metabolism, 20, 669- 675.
- Hanukoglu, A., Mizrachi, A., Dalal, I., et al. (2003) Extrapancreatic autoimmune manifestations in type 1 diabetes patients and their first-degree relatives. Diabetes Care, 26, 1235-1240. doi:10.2337/diacare.26.4.1235
- Gonzalez, G.C., Capel, I., Rodriguez-Espinosa, J., et al. (2007) Thyroid autoimmunity at onset of type 1 diabetes as a predictor of thyroid dysfunction. Diabetes Care, 30, 1611-1612. doi:10.2337/dc07-1292
- Radetti, G., Paganini, C., Gentili, L., et al. (1995) Frequency of hashimoto’s thyroiditis in children with type 1 diabetes mellitus. Acta Diabetologica, 32, 121-124. doi:10.1007/BF00569570
- Menon, P.S., Vaidyanathan, B. and Kaur, M. (2001) autoimmune thyroid disease in Indian children with type 1 diabetes mellitus. Journal of Pediatric Endocrinology & Metabolism, 14, 279-286.
- Shiva, S. and Behbahan, A.G. (2009) Autoimmune thyroid disease in children and adolescents with type 1 diabetes mellitus in Northwest Iran. Saudi Medical Journal, 30, 673-676.
- Kordonouri, O., Charpenter, N. and Hartmann, R. (2011) GADA positivity at onset of type 1 diabetes is a risk factor for the development of autoimmune thyroiditis. Pediatric Diabetes, 12, 31-33. doi:10.1111/j.1399-5448.2010.00666.x
- Kalicka-Kasperczyk, A., Dziatkowiak, H., Bratnik-Mikuta, A., et al. (2002) Thyroid peroxidase antibodies and thyroid disease in children and adolescents with newly diagnosed type 1 diabetes. Przegląd Lekarski, 59, 509- 513.
- Kordonouri, O., Hartmann, R., Deiss, D., et al. (2005) Natural course of autoimmune thyroiditis in type 1 diabetes: Association with gender, age, diabetes duration, and puberty. Archives of Disease in Childhood, 90, 411-414. doi:10.1136/adc.2004.056424
- Czerniawska, E., Szalecki, M., Piatkowska, E., et al. (2003) Prevalence of thyroid antibodies (TPO and ATG) at the onset of type 1 diabetes mellitus in children treated in two diabetes centers in Lods and Kielce. Medycyna Wieku Rozwojowego, 7, 223-228.
- Abrams, P., De Leeuw, I., Vertommen, J., Belgian Diabetes Registry (1996) In new-onset insulin-dependent diabetic patients the presence of anti-thyroid peroxidase antibodies is associated with islet cell autoimmunity and the high risk haplotype HLA DQA1*0301-DQB1*0302. Diabetic Medicine, 13, 415-419. doi:10.1002/(SICI)1096-9136(199605)13:5<415::AID-DIA96>3.0.CO;2-X
- Erten, G., Gurol, A.O., Deniz, G., et al. (2007) Organ specific autoantibodies in preclinical and early clinical type 1 diabetes in Turkey. Upsala Journal of Medical Sciences, 112, 231-243. doi:10.3109/2000-1967-197
- Molina Lacasa, A., Fernandez Cestaner, M., Perez Maraver, M., et al. (1998) Autoimmune thyroid pathology in recently diagnosed diabetes mellitus type 1. Revista Clínica Española, 198, 812-821.
- Sumnik, Z., Drevinek, P., Sanjderova, M., et al. (2003) HLA-DQ polymorphisms modify the risk of thyroid autoimmunity in children with type 1 diabetes mellitus. Journal of Pediatric Endocrinology & Metabolism, 16, 851-858. doi:10.1515/JPEM.2003.16.6.851
- Kordonouri, O., Klinghammer, A., Lang, E.B., et al. (2002) Thyroid autoimmunity in children and adolescents with type 1 diabetes. Diabetes Care, 25, 1346-1350. doi:10.2337/diacare.25.8.1346
- Maugendre, D., Guilhem, I., Karacatsanis, C., et al. (2000) Anti-TPO antibodies and screening of thyroid dysfunction in type 1 diabetic patients. Annales d’Endocrinologie (Paris), 61, 524-530.
- Arauijo, J., Brandoa, L.A., Guimaraes, R.L., et al. (2008) Prevalence of autoimmune thyroid disease and thyroid dysfunction in young Brazilian patients with type 1 diabetes. Pediatric Diabetes, 9, 272-276. doi:10.1111/j.1399-5448.2008.00394.x
- Severinski, S., Banac, S., Severinski, N.S., et al. (2009) Epidemiology and characteristics of thyroid dysfunction in children and adolescents with type 1 diabetes. Collegium Antropologicum, 33, 273-279

