Open Journal of Pediatrics
Vol.3 No.4(2013), Article ID:40107,7 pages DOI:10.4236/ojped.2013.34057
Lack of correlation between obesity and gastroesophageal reflux disease (GERD) in a pediatric cohort*
![]()
1Department of Pediatrics, Division of Gastroenterology, Hepatology and Nutrition, State University of New York, New York, USA
2Department of Pathology, State University of New York, New York, USA
3Scientific Computing Center, State University of New York—Downstate Medical Center, New York, USA
Email: #Simon.Rabinowitz@Downstate.edu
Copyright © 2013 Simon S. Rabinowitz et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 27 September 2013; revised 24 October 2013; accepted 2 November 2013
Keywords: Pediatric; GERD; Obesity; Endoscopy; Histopathology
ABSTRACT
Objectives: Previous reports correlating obesity with gastroesophageal reflux disease (GERD) in children have yielded conflicting results. This study examined whether increasing BMI (body mass index) correlated with increasing grades of endoscopic and/or histopathologic GERD in a cohort of inner city children. Designs and Methods: 340 consecutive children (1 - 18 years) were classified as obese (BMI > 95%) for age and gender. Both endoscopic findings and esophageal histopathology were characterized by graded adult GERD scoring systems. Normal and abnormal grades were then stratified based on BMI. Results: In the study cohort (mean age 10.5 ± 4.7 yrs), 29% were obese (BMI > 95%) and 24% of the total cohort demonstrated endoscopic features of GERD. With increasing severity of endoscopic GERD (from normal to advanced), the percentage of obese patients at each grade did not increase (Grade 0 = 30%, Grade 1 = 26%, Grades 2 - 4 = 30%). Histopathologic findings consistent with GERD were noted in 21% of the total population studied. Again, the percentage of obese children in each diagnostic category (Grades 0 - 3) did not increase with increasing severity of inflammation. Conclusions: In this cohort of inner city children, obesity was not associated with an increased prevalence of GERD as defined by adult scoring systems.
1. INTRODUCTION
Obesity, defined by body mass index (BMI) [1-6] or by abdominal circumference [7,8], is an established risk factor for gastroesophageal reflux disease (GERD) [1-8] and for its complications [1,2,3,7] in adults. However, the published data analyzing the relationship between obesity and GERD in children have yielded conflicting results. Part of this controversy is related to the fact that, while GERD in children is frequently diagnosed and treated, the accepted diagnostic criteria are somewhat subjective, making evidence based conclusions challenging. Two recent pediatric publications, one a clinical practice guideline issued jointly by the North American and European Societies for Pediatric Gastroenterology, Hepatology and nutrition [9], and the second international consensus [10], defined pediatric GERD as “when the reflux of gastric contents causes worrisome symptoms or complications”. The joint guideline also concluded that “history and physical examination may be sufficient to diagnose GERD if the symptoms are typical” [9]. Both publications acknowledged that in children: 1) reflux tests may identify variations from normal, but cannot predict symptom severity, natural history or response to therapy; 2) daily GERD symptom questionnaires have some value, but are not validated; 3) no validated or universally accepted endoscopic findings exist to diagnose GERD; and 4) histologic findings are neither sufficiently sensitive nor specific to diagnose reflux esophagitis and conversely, absence of these histologic changes does not rule out GERD. Hence, publications investigating GERD in children have employed a variety of criteria to define cohorts and determine epidemiologic associations.
Among the three published studies that have demonstrated a positive correlation between obesity and GERD in children, there is no uniformity in how the investigators diagnosed GERD [11-13]. A questionnaire given to 236 obese (ages 7 - 16 years) children attending the Yale pediatric clinic yielded a significantly higher reflux symptom score (13.1%) compared to their control patient group (2%) [11]. A large study utilizing a coding diagnosis of GERD from over 690,000 children reported a GERD odds ratio of 1.3 for GERD in obese children ages 6 - 19 years, compared with normal weight subjects. In contrast, obesity was not significantly associated with an increased risk for GERD in children aged 2 - 5 years in the same study [12]. A third retrospective chart review, conducted at the Texas Children’s Hospital, identified 627 urban children (ages 2 - 17 years) with GERD based on upper gastrointestinal endoscopic evaluations (n = 131) or on clinical symptoms (n = 496). The authors concluded, regardless of the defining criteria, a positive association existed between childhood obesity and GERD [13].
In contrast to the above associations, two recent pediatric studies that employed histopathologic diagnostic criteria, failed to show a positive correlation between obesity and GERD. A retrospective review of a predominantly Caucasian cohort of 738 children (mean age 10.6 ± 3.4 years) from West Virginia, utilizing distal esophageal biopsies, and analyzed with an adult GERD scoring system, concluded that reflux esophagitis was not associated with increased BMI [14]. Another review of distal esophageal tissue from 230 New York City children (2 - 20 years) employed a modification of a different adult GERD histology scoring scale [15]. These authors also found a similar prevalence of reflux esophagitis (23.9%) in their overweight (BMI > 85%) and normal weight group (24.5%) [16].
The impact of any potential association between BMI and disease is highlighted by the alarming increase in the prevalence of obesity in children in the United States [17]. While this epidemic is widespread, the greatest increases have been documented in Mexican American and Non-Hispanic African-American children and teenagers [18]. According to New York City Department of Health data from 2007, the prevalence of obesity in Brooklyn children is 26%, significantly higher than the national average [19]. Since the majority of the patients treated in our hospital come from the most vulnerable ethnic group, inner-city African-Americans, determining whether increased BMI predisposes to the onset and severity of GERD in this population is of particular importance. This report describes the prevalence of GERD as a function of BMI in a cohort of inner city children who underwent upper endoscopy and biopsy. As validated quantitative scoring systems for diagnosing and characterizing pediatric GERD do not exist, and since the significance of any association between obesity and GERD will ultimately be determined by whether pediatric GERD is a true precursor to the complications seen in adults, this study measured GERD utilizing endoscopic [20] and histologic [15] grading systems employed in the adult literature.
2. PATIENTS AND METHODS
A retrospective analysis of the medical records of all 367 children who underwent an upper endoscopy for symptoms consistent with GERD between Jan 1, 2007 and Dec 31, 2009 was performed. Although the chart review did not include ethnicity, the medical center and our division sees almost 80% African American and African-Caribbean patients, with the majority of the remaining children being Hispanic. The only children excluded were those less than 1 year of age, those without anthropometric data, and those in whom esophageal biopsies were not available for review. We identified 340 eligible patients for whom a complete data set was available including demographic data (age, gender, height, weight and a calculated BMI), endoscopy reports, histopathology reports and slides for review. The mean age of the entire group was 10.5 ± 4.7 years. Combining the two highest BMI groups, 43% of the total cohort was obese or overweight. The patients were divided into 3 age groups: 1 - 5 years, 6 - 10 years, and 11 - 18 years. All of the esophageal biopsies performed were independently reviewed for this study by two blinded pathologists (AN, XZ). The patients’ gender-specific BMI percentiles were calculated, based on the Centers for Disease Control (CDC) values reported for year 2000 [21]. Groups were defined as follows: underweight (BMI < 5th%), normal weight (BMI for age >5th% to <85th%), overweight (BMI for age ≥85% to <95%) and obese (BMI for age ≥95%).
In these analyses, endoscopic and histologic esophageal abnormalities were graded using scoring systems developed for classifying GERD in adults. The Hetzel-Dent scoring system [20] was used to characterize the endoscopic features of GERD. This scoring system is commonly applied to adult patients, and it has been recommended for use in children by consensus panels [9,10]. Classification of distal esophageal histopathology was determined utilizing the criteria developed by Zentilin et al. to diagnose GERD in adults [15]. In both, Grade 0 is considered normal with increasing scores (Grades 1 - 4 endoscopic and Grades 1 - 3 histopathologic) defining increasing severity. The study was approved by the Institutional Review Board of State University of New York, Health Science Center at Brooklyn, New York.
3. STATISTICAL ANALYSIS
The statistical analysis employed the ordinal nature of the variable grades of endoscopic (Grades 0 - 4) and histopathologic (Grades 0 - 3) abnormalities. Spearman correlation coefficients for associations between BMI and GERD features were calculated and found to be not significant (data not shown). Therefore, in order to control for the potentially confounding variable of age, generalized Cochran-Mantel-Haenszel tests [22] determined significant associations between BMI and either histology or endoscopy. A two sided p value < 0.05 was considered statistically significant. Data were analyzed with SAS software, version 9.2 (SAS Institute, Cary, NC).
4. RESULTS
The demographic characteristics of the study population (mean age, gender, and BMI) are shown in Table 1. In this cohort of children aged 1 - 18 years, 29% were obese, 14% were overweight, 51% were in the normal range and 6% were underweight. These values highlight the increasing BMIs in inner-city cohorts and are consistent with previously published data for the borough of Brooklyn [19]. Figure 1 shows the BMI of the entire range of the cohort and defines the sub-cohorts of obese, overweight, healthy (i.e. normal) weight and underweight. The indications for endoscopy (abdominal and/or chest pain, regurgitation and/or emesis, or both) were independent of the patients’ BMIs. For obese, overweight, and normal children the percent studied for regurgitation/emesis was: 17%, 23%, and 18%. The percent with only pain was: 74%, 69%, and 76% stratified by the same weight group distribution, and for children with both pain and emesis the prevalence was 6%, 8%, and 6%. The remaining few had dysphagia. Figure 2 examines the distribution of BMI of the study patients based on three different age groups: 1 - 5 years, 6 - 10 years and 11 - 18 years. While a high prevalence of obesity was observed in all age groups, it was highest (41%) in the 6 - 10 years group. This prevalence is greater than twice the (20%) reported in the NHANES 2007-2008 data set for American children aged 6 - 11 [17].
As discussed under methods, adult scoring systems were employed in this study. Of the total number of 340 study subjects, 258 (76%) had normal (Grade 0) endoscopic findings. Thirty percent of the patients with nor-
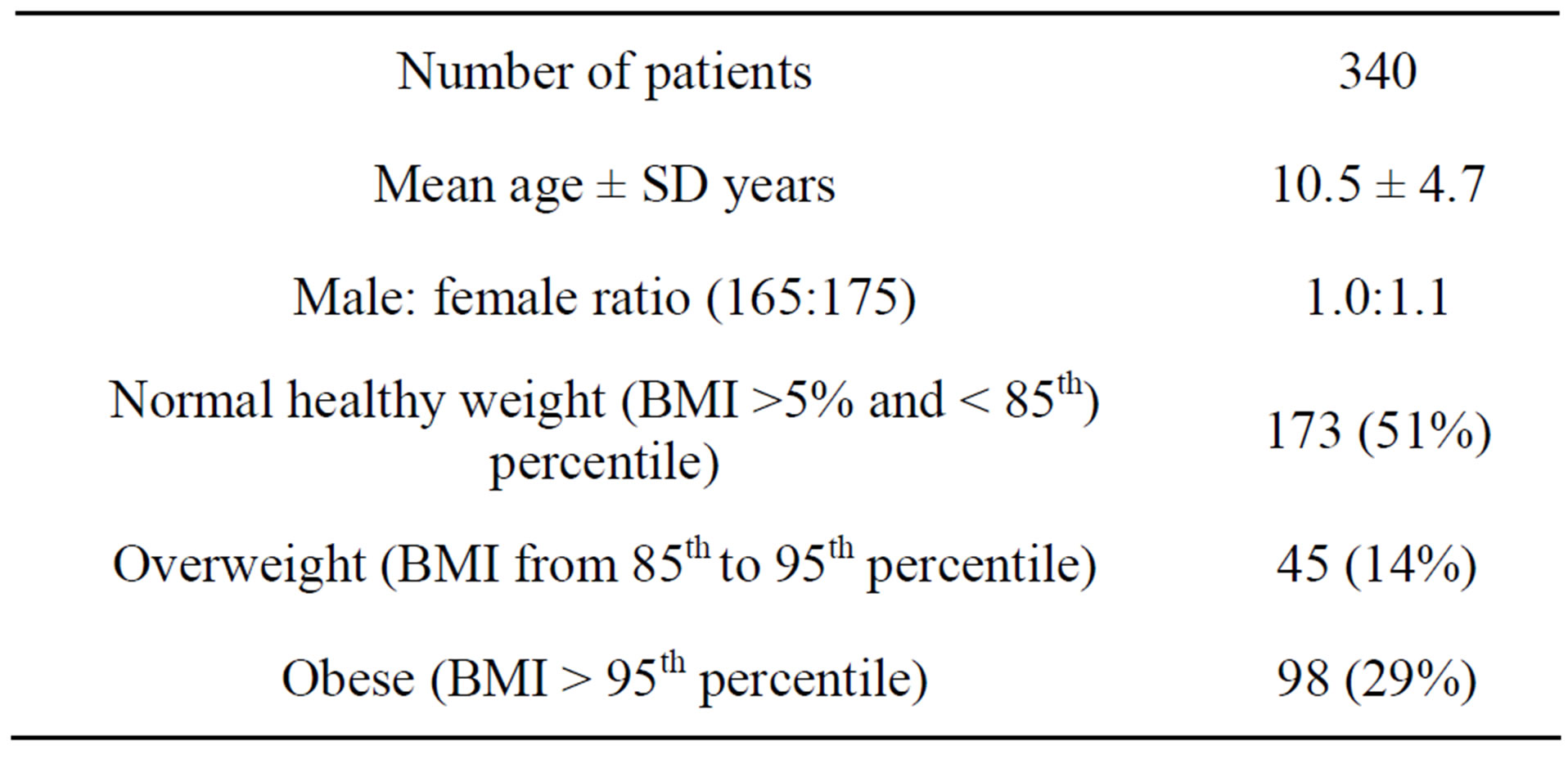
Table 1. Demographic characteristics of study population.
mal mucosa were obese. Based on the adult criteria, 82 children (24% of the total cohort) demonstrated endoscopic abnormalities (Figure 3). Almost all of the findings, 72/82 (88%) had the mildest findings, consistent with Grade 1 GERD. As the remaining groups were so small, endoscopic Grades 2 (n = 6), 3 (n = 4), and 4 (n = 0) were pooled and are presented together. The percentage of obese children in each diagnostic category (Grades 0, 1, and 2 - 4) did not increase with increasing severity of mucosal involvement. Furthermore, no significant overall association was found between BMI and endoscopic grade (p = 0.75).
Histopathologic grading of esophageal biopsies is shown in Figure 4. Of the total cohort of 340 patients, 270 (79%) were classified Grade 0, without any histopathologic findings of GERD. Among the 270 normal studies, 30% were obese and 15% were overweight. Again, as the histopathologic severity of GERD increased, no increase in the proportion of obese children in each diagnostic category was noted (Figure 4). In addition, even after controlling for age, no significant correlations were found between BMI and the grade of histopathologic abnormality (p = 0.16).
5. DISCUSSION
In adults, numerous meta-analyses and/or large scale population studies have established a positive correlation between obesity and GERD [1-8]. Because any significant GERD related morbidity in obese children will likely be similar in nature to GERD related morbidity in obese adults, and because no quantitative, validated criteria to diagnose pediatric GERD have been established, this study employed adult endoscopic and histologic criteria. The most reliable endoscopic feature of GERD in adults, visible breaks in the esophageal mucosa [23], has been employed to develop an endoscopic scoring system that has been recommended for use in children [9,10]. Although expert consensus panels maintained that esophageal histopathology is unable to diagnose or to exclude pediatric GERD [9,10], a recent multicenter Italian study on GERD in children concluded that the histopathologic finding of esophageal inflammation is often a more sensitive criterion than endoscopic appearance [24]. These authors also found that both the endoscopic and the histologic scores of esophagitis improved after acid suppression therapy. The interpretation of esophageal biopsies in our cohort employed a quantitative histopathologic scoring system that has a high sensitivity (84%) and specificity (85%) for diagnosing GERD in adults [15]. This same scoring system had also been previously adopted for use in children [16].
Our inner city population referred for upper endoscopy included a large proportion (43%) of children with BMI
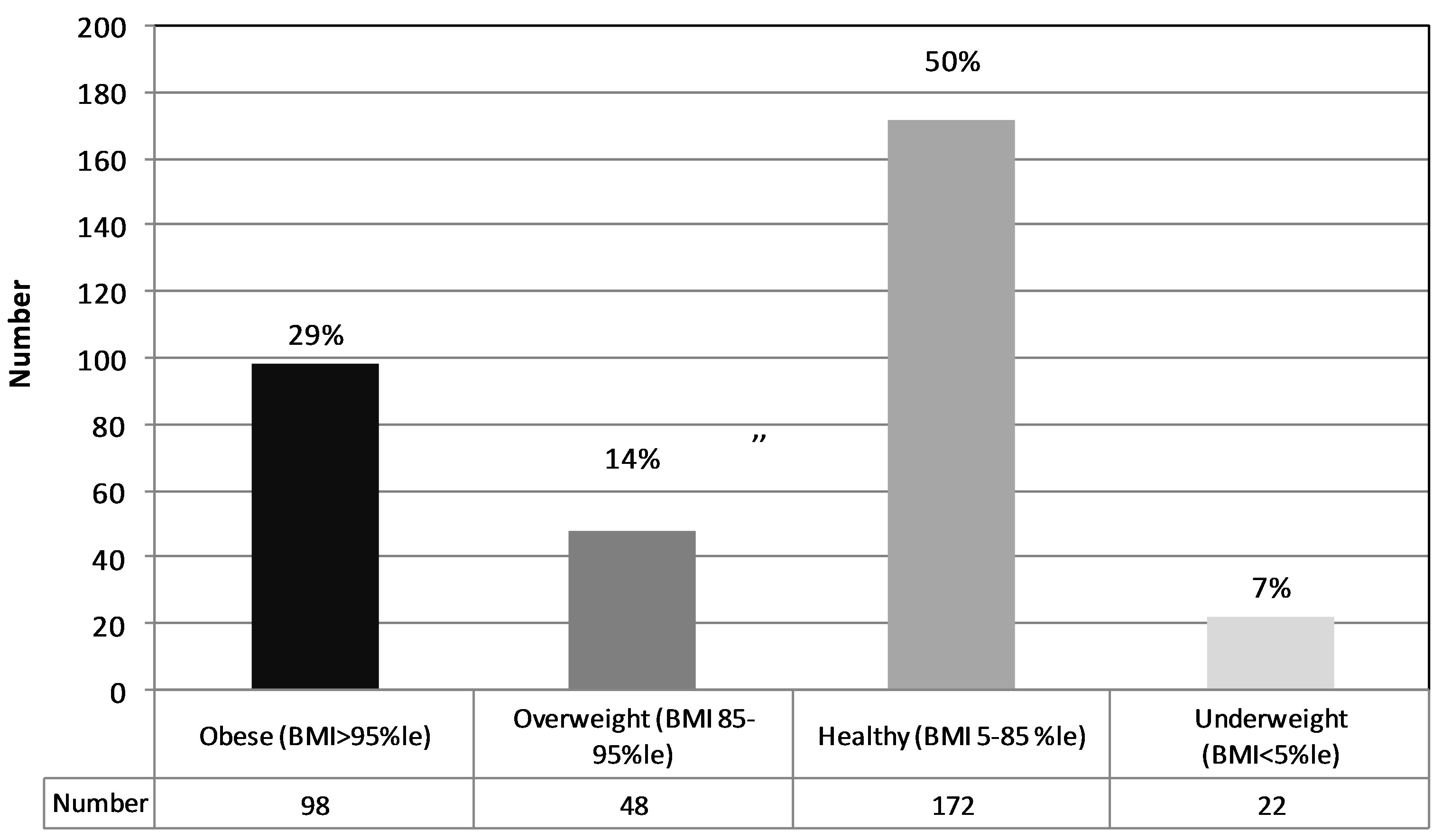
Figure 1. The distributions of BMIs in the study population. The classifications of BMIs were based on the percentiles found on the standardized CDC growth curves developed from 2000 data. The same representation of the different BMI groups is maintained throughout the paper.
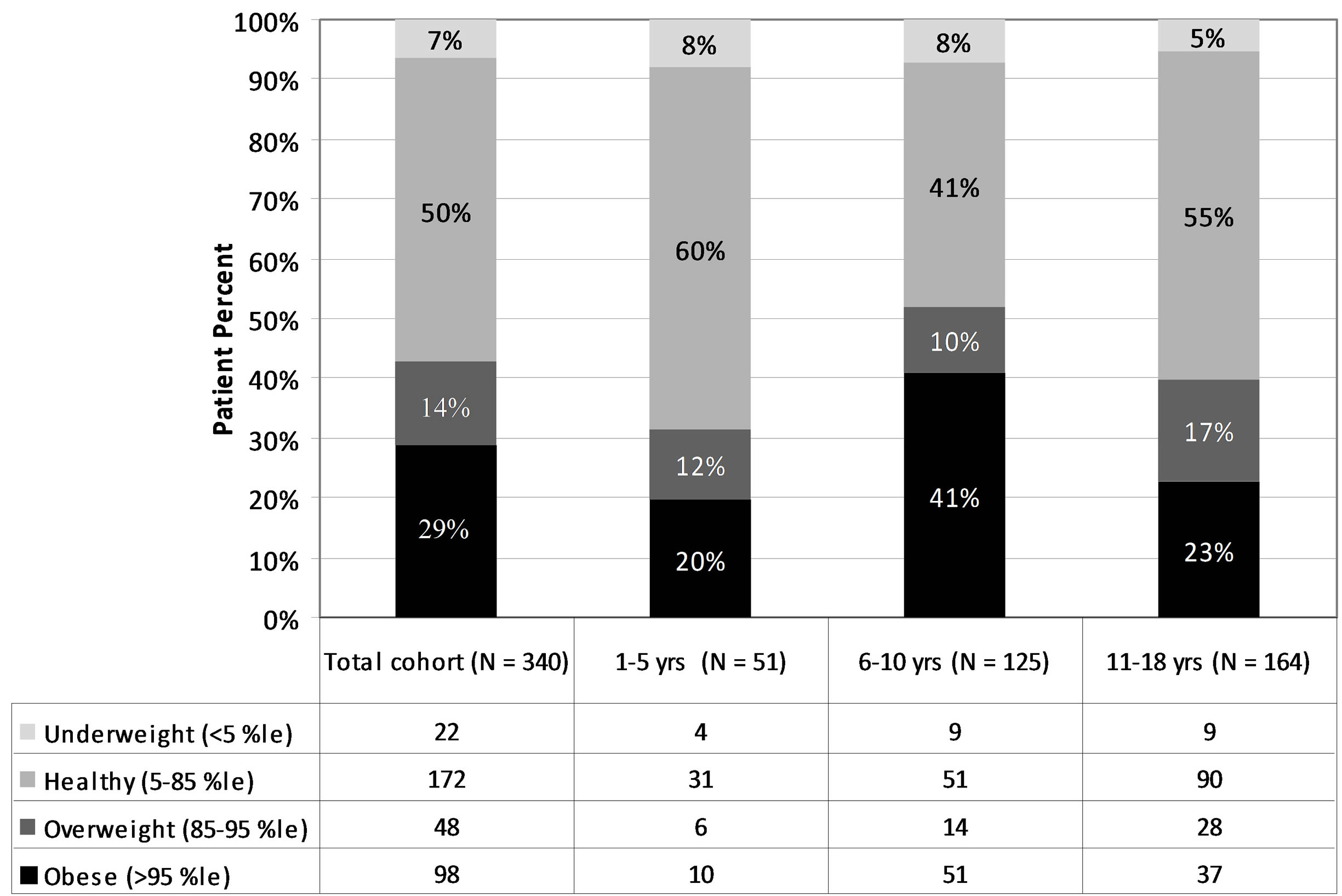
Figure 2. The individual distributions of BMIs based on the ages of the children in the study. In the age group 6 - 10 years, the prevalence of obesity is statistically greater (p < 0.01) than the other two aged groups.
in the overweight-obese range. This provided us with the opportunity to compare the presence and severity of GERD among normal weight, overweight, and obese children. In this study, neither endoscopic nor histopathologic GERD increased with increasing BMI. In addition, neither macroscopic nor microscopic disease severity showed an overall correlation with increasing BMI. This same conclusion had been previously reached in both rural [14] and urban [16] American children and would seem to be inconsistent with the extensive data associating these conditions in adults.
Several explanations could account for the variance between the correlation of obesity with adult GERD and our findings. All of the potential problems alluded to above in diagnosing GERD in children, and/or the theoretical limitations in applying adult scoring systems to
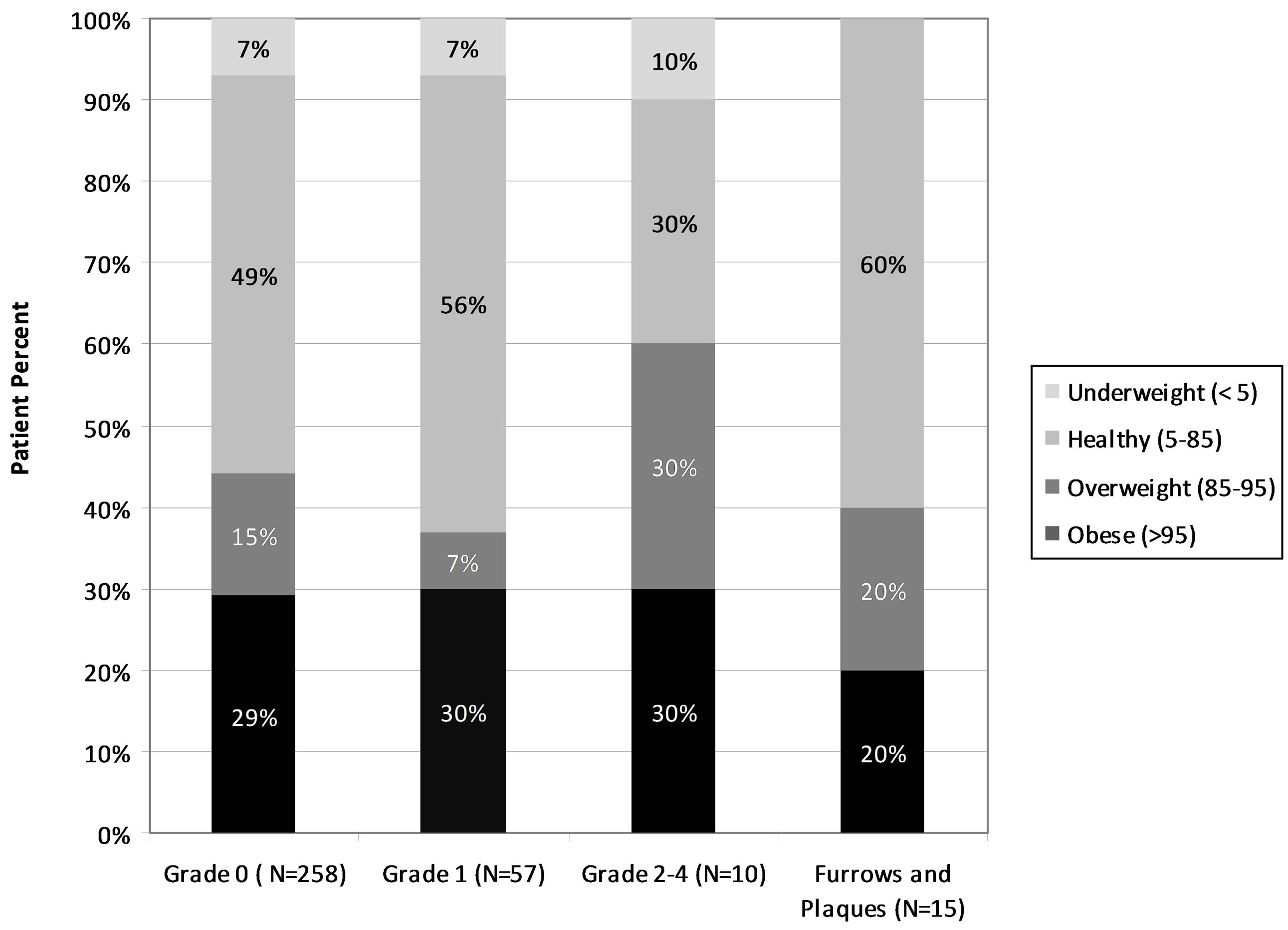
Figure 3. The percentages of obese, overweight, and healthy weight children with various grades of distal esophageal endoscopic findings. Higher grades indicate greater degrees of abnormality as described in methods. All of the p-values comparing the proportions of obese patients among the various groups are not significant, p > 0.05.
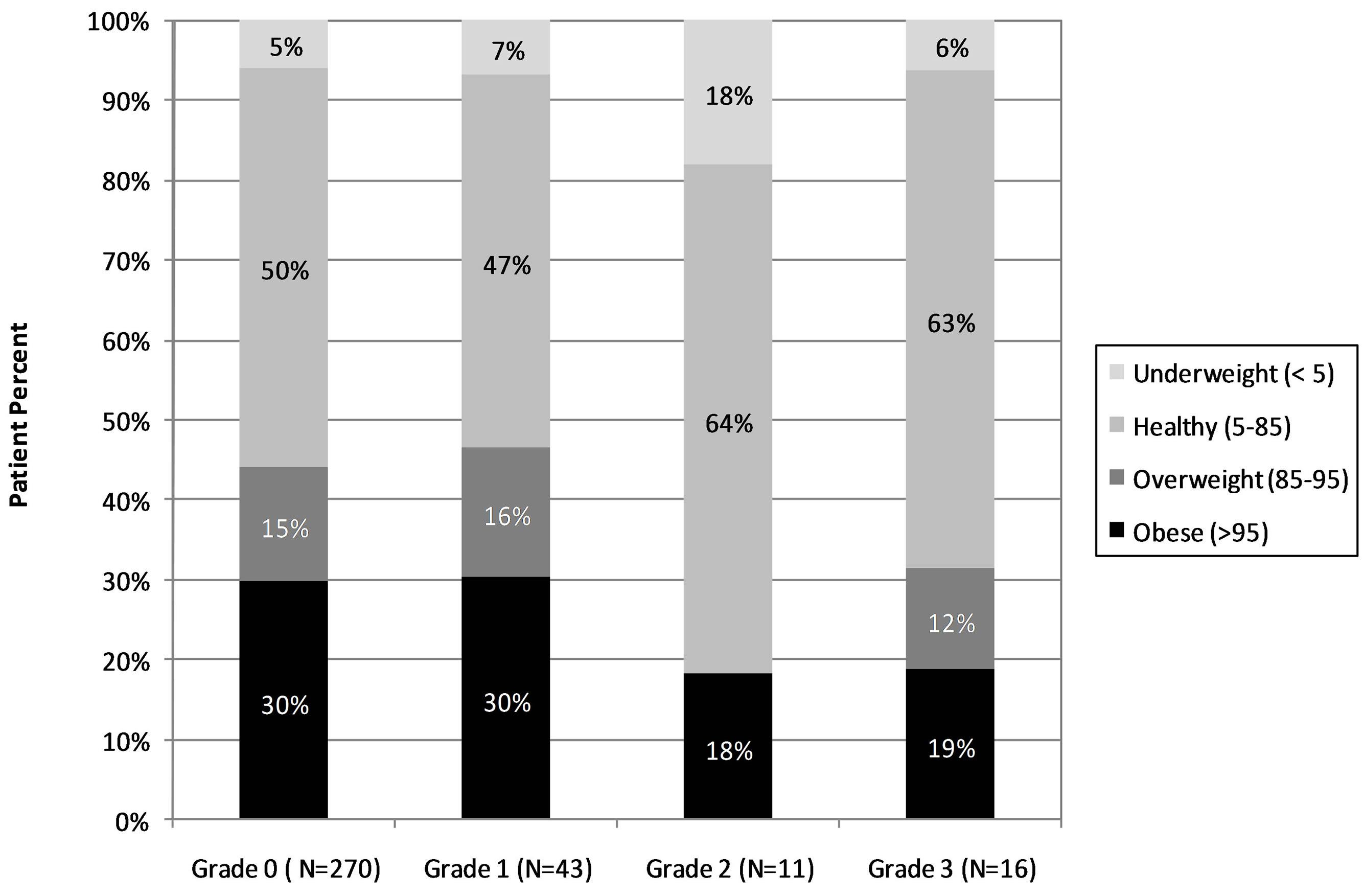
Figure 4. The percentages of obese, overweight, and healthy weight children with various degrees of distal esophageal histopathology. Higher grades reflect greater degrees of esophagitis as described in the methods. All of the p-values comparing the proportions of obese patients among the various groups are not significant, p > 0.05.
pediatric subjects, could conceal a relationship that exists. These theoretical limitations are particularly relevant, as relatively few of our children had the advanced degrees of either endoscopic or histologic esophageal disease frequently encountered in adults. Additionally, variations in the documentation of endoscopic esophagitis, the biopsy protocols employed, and the staining and interpretation of biopsy specimens have been widely recognized [9,10]. Any or all of these assessment variables may have potentially obscured a true association. While not universally confirmed, one study failed to find a correlation between obese African Americans adults and GERD [8]. Hence, a conclusion in our population may not be able to be generalized to Caucasian children. Finally, several authors have reported, in adults, that increasing abdominal circumference is a more sensitive variable than BMI to correlate with GERD [7,8]; unfortunately, that data are not available for our cohort. However, we speculate that the inability to correlate obesity and GERD in children may be related to the same factors that have confounded prior attempts to stringently define pediatric GERD.
While GERD is universally recognized as a pathologic state resulting from the retrograde passage of gastric contents into the esophagus, the etiopathogenesis of this phenomenon has substantial variability based on age. Among adults with GERD, hiatal hernia and age-related weakening of the lower esophageal sphincter (LES) had previously been proposed as primary risk factors; however, presently the most widely accepted predisposing event involves transient, inappropriate LES relaxations. In children, the specificity of the accepted pediatric GERD diagnostic criteria is inherently compromised by the more frequent occurrence of infections, allergies, respiratory conditions, and dietary intolerance that can all transiently impair upper gastrointestinal physiology and yield “worrisome symptoms”. It is also probable that the large majority of pediatric GERD, as in the present study, have milder objective findings, which could potentially compromise the sensitivity of the currently accepted diagnostic criteria.
Although the results of our retrospective study fail to demonstrate an association between pediatric GERD and obesity, they do not address the possibility that obese children, especially those that remain morbidly obese, may have reflux that is more likely to persist beyond adolescence. The chronicity of the condition could put them at higher risk for the complications noted in obese adults. Although the pediatric consensus definition discusses obesity in the section for conditions predisposing for severe, chronic GERD [10], this is based only on adult data. Given the epidemic of overweight, obese, and morbidly obese children who are at risk for becoming obese adults, prospective, long-term studies on the natural history of GERD and its complications in this cohort are desirable. Ideally, these will employ universally validated or consensus driven guidelines to objectively and quantitatively diagnose and measure pediatric GERD.
REFERENCES
- Sharma, P., Vakil, N., Monyak, J.T. and Silberg, D.G. (2013) Obesity does not affect treatment outcomes with proton pump inhibitors. Journal of Clinical Gastroenterology, 47, 672-677. http://dx.doi.org/10.1097/MCG.0b013e31827e46be
- Cai, N., Ji, G.Z., Fan, Z.N., Wu, Y.F., Zhang, F.M., Zhao, Z.F., Xu, W., Liu, Z. (2012) Association between body mass index and erosive esophagitis: A meta-analysis. World Journal of Gastroenterology, 18, 2545-2453. http://dx.doi.org/10.3748/wjg.v18.i20.2545
- Hampel, H., Abraham, N.S. and El-Serag, H.B. (2005) Meta-analysis: Obesity and the risk for gastroesophageal reflux disease and its complications. Annals of Internal Medicine, 143, 199-211. http://dx.doi.org/10.7326/0003-4819-143-3-200508020-00006
- Ayazi, S., Hagen, J.A., Chan, L.S., DeMeester, S.R., Lin, M.W., Ayazi, A., Leers, J.M., Oezcelik, A., Banki, F., Lipham, J.C., DeMeester, T.R. and Crookes, P.F. (2009) Obesity and gastroesophageal reflux: Quantifying the association between body mass index, esophageal acid exposure, and lower esophageal sphincter status in a large series of patients with reflux symptoms. Journal of Gastrointestinal Surgery, 13, 1440-1447. http://dx.doi.org/10.1007/s11605-009-0930-7
- Peura, D.A., Pilmer, B., Hunt, B., Mody, R. and Perez, M.C. (2013) The effects of increasing body mass index on heartburn severity, frequency and response to treatment with dexlansoprazole or lansoprazole. Alimentary Pharmacology & Therapeutics, 37, 810-818. http://dx.doi.org/10.1111/apt.12270
- Eslick, G.D. (2012) Gastrointestinal symptoms and obesity: A meta-analysis. Obesity Reviews, 13, 469-479. http://dx.doi.org/10.1111/j.1467-789X.2011.00969.x
- Cook, M.B., Greenwood, D.C., Hardie, L.J., Wild, C.P. and Forman, D. (2008) A systematic review and metaanalysis of the risk of increasing adiposity on Barrett’s esophagus. American Journal of Gastroenterology, 103, 292-300. http://dx.doi.org/10.1111/j.1572-0241.2007.01621.x
- Corley, D.A., Kubo, A. and Zhao, W. (2006) Abdominal obesity, ethnicity and gastro-oesophageal reflux symptoms. Gut, 56, 756-762. http://dx.doi.org/10.1136/gut.2006.109413
- Vandenplas, Y., Rudolph, C., Di Lorenzo, C., Hassall, E., Liptak, G., Mazur, L., Sondheimer, J., Staiano, A., Thomson, M., Veereman-Wauters, G. and Wenzl, T. (2009) Pediatric gastroesophageal reflux clinical practice guidelines: Joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN). Journal of Pediatric Gastroenterology and Nutrition, 49, 498-547.
- Sherman, P.M., Hassall, E., Fagundes-Neto, U., et al. (2009) A global, evidence based consensus on the definition of gastroesophageal reflux disease in the pediatric population. American Journal of Gastroenterology, 104, 1278-1295. http://dx.doi.org/10.1038/ajg.2009.129
- Pashankar, D.S., Corbin, Z., Shah, S.K. and Caprio, S. (2009) Increased prevalence of gastroesophageal reflux symptoms in obese children evaluated in an academic medical center. Journal of Clinical Gastroenterology, 43, 410-413. http://dx.doi.org/10.1097/MCG.0b013e3181705ce9
- Koebnick, C., Getahun, D., Smith, N., Porter, A.H., DerSarkissian, J.K. and Jacobsen, S.J. (2011) Extreme childhood obesity is associated with increased risk for gastroesophageal reflux disease in a large population based study. International Journal of Pediatric Obesity, 6, e257-e263. http://dx.doi.org/10.3109/17477166.2010.491118
- Malaty, H., Fraley, J.K., Abudayyeh, S., Fairly, K.W., Javed, U.S., et al. (2009) Obesity and gastroesophageal reflux disease and gastroesophageal reflux symptoms in children. Clinical and Experimental Gastroenterology, 2, 31-36. http://dx.doi.org/10.2147/CEG.S4715
- Elitsur, Y., Dementieva, Y., Elitsur, R. and Rewalt, M. (2009) Obesity is not a risk factor in children with reflux esophagitis: A retrospective analysis of 738 children. Metabolic Syndrome and Related Disorders, 7, 211-214. http://dx.doi.org/10.1089/met.2008.0069
- Zentililn, P., Savarino, V., Mastracci, L., Spaggiari, P., et al. (2005) Reassessment of the diagnostic value of histology in patients with GERD, using multiple biopsy sites and an appropriate control group. American Journal of Gastroenterology, 100, 2299-2306. http://dx.doi.org/10.1111/j.1572-0241.2005.50209.x
- Patel, N., Ward, M., Beneck, D., Cunningham-Rundles, S., et al. (2010) The association between childhood overweight and reflux esophagitis. Journal of Obesity, 2010, Article ID: 136909. http://dx.doi.org/10.1155/2010/136909
- Ogen, C. and Carroll, M. (2010) Prevalence of obesity among children and adolescents: United States, trends 1963-1965 through 2007-2008. NCHC Health E-Stat. http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.htm
- Ogden, C., Flegal, K., Carroll, M. and Johnson, C. (2002) Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA, 288, 1728-1732. http://dx.doi.org/10.1001/jama.288.14.1728
- Matte, T., Noyes, P., Karpati, A., Selenic, D., et al. (2007) Obesity in Bedford-Stuyvesant and Bushwick: A look across generations. New York City Department of Health and Mental Hygiene, New York.
- Hetzel, D.J., Dent, J., Reed, W.D., Narielvala, F.M., et al. (1988) Healing and relapse of severe peptic esophagitis after treatment with omeprazole. Gastroenterology, 95, 903-912.
- Kuczmarski, R.J., Ogden, C.L., Grummer-Strawn, L.M., et al. (2000) CDC growth charts: United States. Advance Data, 314, 1-27.
- Agresti, A. (2002) Categorical data analysis. 3rd Edition, John Wiley & Sons, New York. http://dx.doi.org/10.1002/0471249688
- Vakil, N., Van Zanten, S.V., Kahrilas, P., et al. (2006) The Montreal definition and classification of gastroesophageal reflux disease: A global evidence based consensus. American Journal of Gastroenterology, 101, 1900- 1920. http://dx.doi.org/10.1111/j.1572-0241.2006.00630.x
- Lombardi, G., Angelis, G., Rutigliano, V., Guariso, G., et al. (2007) Reflux oesophagitis in children: The role of endoscopy A multicentric Italian survey. Digestive and Liver Disease, 39, 864-871. http://dx.doi.org/10.1016/j.dld.2007.05.018
NOTES
*Disclosures and conflicts: none of the authors have any reported conflicts of interest.
#Corresponding author.

