 Vol.3, No.7, 423-431 (2011) doi:10.4236/health.2011.37070 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Health T cell responses to der f 2 mite allergens in thai allergic patients Duangthep Thongdee1, Jundee Rabablert1*, Tharit Muninnobpamas2, Piyalarp Wasuwat2, Rachanoo Pipatchaipaisan1, Supathra Tiewchareon3, Nat Malainual3 1Department of Biology, Faculty of Science, Silpakorn University, Bangkok, Thailand; *Corresponding Author: jundee@su.ac.th 2Department of Otolaryngology, Pramongkutklao Hospital, Bangkok, Thailand; 3Department of Parasitology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand. Received 3 May 2011; revised 31 May 2011; accepted 27 June 2011. ABSTRACT Dermatophagoides farinae group 2 (Der f2) is a highly polymorphic allergen that shows a dis- tinct pattern of sequence divergence. The effect of the v ar iant s on a nti bo dy a nd T cel l res pon s es has not been compared. The aim of the present study w as to evaluate IgE binding, transcription and translations for IL-5, IFN- and TGF- in- duced by mite allergens. Sera from 24 HDM- allergic patients and 20 non-allergic subjects were measured for IgE reactivity by ELISA. PBMC was cultured with mite allergens (Df, rDerf2) and mitogen (PHA). The supernatants and cell pellet obtained were evaluated for cy- tokine production by ELISA and cytokine gene expression by RT-PCR, respectively. Four pa- tients showed IgE reactivity to both allergens. Five patients showed IgE reactivity to Df. Other allergic patients and all non-allergic subjects did not show IgE reactivity to mite allergens. Both aller g ens show ed similar levels of IL-5 and IFN- transcriptions in allergic patients and non- -allergic subjects. The rDer f2 induced IL-5 pro- tein from allergic patients higher than non- al- lergic subjects, while Df showed IL-5 protein from allergic patients similar to non-allergic subjects. Df induced IFN- protein from allergic patients higher than non-allergic subjects whe- reas rDer f2 induced IFN- protein from allergic patients similar to non-allergic subjects. The ratio of IFN- to IL-5 production after stimulation with rDer f2 was higher in non-allergic subjects than in allergic patients. Our data demonstrated that the changes in the sequence of rDer f2 compared with native Df had effect on cytokine production in both allergic patients and non- -allergic subjects. Keywords: Dermatophagoides Farinae; IgE; IL-5; IFN- ; TGF- 1. INTRODUCTION Dermatophagoid es farinae is a species of house dust mites (HDM) which belong to the family Pyroglyphidae. The mite has been ubiquitously found in common houses in Tropical and subtropical areas [1]. D. farinae has been recognized as important source of allergens associated with allergic diseases such as asthma, rhinitis, and atopic dermatitis [2]. Group 2 allergen (Der f2 from D. farinae) is products of single gene, but it shows fre- quent allelic variation affecting several amino acids. Recombinant Der f2 (rDer f2) is a convenient molecule for investigat- ing polymorphic proteins. It can be read- ily produced as a highly allergenic recombinant protein which has been used for X-ray crystallography and other conformational analyses [3]. Seven amino acid substitu- tion differences from native Df are S57N, L58I, D59N, I63V, F75Y, V76I, and I88A. Different variants of Der f2 have dif- ferent immunoglobulin E binding activities [4]. The amino acid substitutions can render T cell epitopes ac- tive or inactive. The cytokine pattern of T cell re- sponses induced by different variants of rDer f2 was also found to differ even with a single amino acid substitu- tion [5]. Allergen specific T cell producing Th1 and Th2 cyto- kines can be detected in blood of atopic adults [6,7]. The cause of this allergen-specific Th2 predominance in atopic could be related to a dysfunction of the regulatory cytokine that modulate Th1 and Th2 responses. Experi- mental and theoretical data support the idea that activa- tion of Th2 cells leads to production of IL-4, IL-5 and IL-13 that are cytokines involved in the synthesis of specific IgE and eosinophylic inflammation [8]. On the  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 424 other hand, Th1 cells, that produce IFN-γ, inhibit the biological effects of Th2 cytokine and are involved on delay type hypersensitivity [9]. In spite of this observa- tion and of their mutual inhibitory properties, the Th1/ Th2 differentiation does not explain some features such as increasing IFN- production by PBMC stimulated by Der f antigens in atopic children [10] and the presence of activated Th1 cells in asthmatic patients with bronchial inflammation and hyper-responsiveness [11] and in some experimental models of asthma [12]. TGF- inhibits T cell differentiation and proliferation of both Th1 and Th2 cells and attracts macrophages, dendritic cells and other inflammatory cells to sites of antigen exposure. TGF- inhibits the function of these cells once they are acti- vated [13]. The increased levels of regulatory cytokines TGF- in atopic patients suggest attempts to control the inflammatory response [14]. The major diagnosis methods of allergic diseases in- clude skin pick tests (SPT) and serum specific IgE de- tection. Since the SPT possesses simple, quick, inexpen- sive and highly sensitive characteristics, it has long been one of most essential methods for diagnosis of type I allergic diseases in spite of the rapid development of science and technology over the past century [15,16]. SPT allows the detection if IgE-mediated sensitivity with simple device and low risk of causing an allergic reaction [15,16]. Enzyme linked immunosorbent assays (ELISA) is accurate and precise measurement of IgE and cytokine production. Reverse transcriptase-polymerase chain reaction (RT-PCR) allows detection of cytokine gene expression due to it has good reproducibility and specificity [17]. The aims of the present study were to evaluate hu- moral and cellular immune responses to D. farinae in allergic patients and non-allergic subjects by determine- ing the levels of specific IgE to Df and rDer f2, the cyto- kine (IL-5, IFN- and TGF- ) gene expression and pro- duction by PBMC stimulated with both allergens. 2. METERIALS AND METHODS 2.1. Mite Extracts Total HDM extracts of D. farinae (Df) was obtained from mite cultures provided by Siriraj Dust Mite Center of Services and research, Department of Parasitology, Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand. Briefly, mite culture was stirred in phosphate buffered saline (PBS), pH 7.4 for overnight at 4 degree Celsius (˚C). The mixture was centrifuged for 20 min at 12,000 xg at 4˚C. The supernatant was filtered through No.1 Whatman paper and through 0.22 μ filter. The ster- ile mite extract was then stored frozen at –20˚C [18]. 2.2. Recombinant Allergen Group 2 of Dermato-phagoides Farinae (rDer f 2) rDer f2 was produced by donated from Assistant Pro- fessor Surapon Piboonpocanun from the Institute of Molecular Biosciences, Mahidol University, Thailand. The positive transformants containing the integration of interested genes were selected for small-scaled expres- sion. Briefly, positive transformants (rDer f 2) and plas- mic vecter (pPICZ) of Pichia pastoris (P. pastoris) [19] were grown in yeast extract peptone dextrose (YPD) containing 100 g/mL ZeocinTM at 30˚C with vigorous shaking for approximately 2 days. The starter cultures were added into 5 mL of fresh buffered minimal glycerol complex medium (BMGY) until the absorbance of BMGY was 0.1 at optical density (OD) 600 nanometer (nm). After that, the starter culture with OD 0.1 was cul- tured until the absorbance of BMGY was 5.0. The BM- GY cultures were centrifuged at 10,000xg for 5 min, and the cell pellets were resuspended in buffered minimal methanol complex medium (BMMY) using 1/5 volume of the original culture volume (approximately 1 mL). To induce expression of recombinant allergens, absolute methanol was added to a final concentration of 3% v/v to the BMMY culture every 24 h. The culture media were collected after 3 day induction. The collected culture media were centrifuged at 12,000 xg in a bench-top mi- cro centrifuge for 3 min at room temperature. The su- pernatant was dialyzed. The proteins were separated by SDS-PAGE followed by transferring the fractionated proteins to a nitrocellu- lose membrane using method as described by the manu- facturer with a wet blotting apparatus (Bio-Rad, USA). The blotted membrane was blocked overnight at 4˚C. The membrane was further incubated with monoclonal anti-group 2 antibodies (mAb 1D8 clone, Indoor bio- technologies Ltd, Manchester, UK). The membrane was incubated with Biotinylated rabbit-anti mouse IgG solu- tion (1:5000) (SouthernBiotech, Birmingham, USA) and BCIP/NBT 1 component substrate (KPL, USA). 2.3. Subject A total of 24 patients with perennial allergic rhinitis and a positive Skin prick test (SPT) to house dust mite allergen (Der p and Der f), were selected for this invest- tigation by Dr. Tharit Muninnobpamas of Department of Otolaryngology, Pramongkutklao Hospital, Bangkok, Thailand. As the control group, 20 healthy subjects with no history of allergic diseases and a negative SPT to all aeroallergen extracts tested were included. The study donor was approved by the Ethics committee in Human Research of the Phramongkutklao Hospital and written informed consent was obtained from all volunteers.  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 425 2.4. Skin Prick Test and Serum Sample The commercial extract of Der p (Dermatophagoides pteronyssinus) and Der f (D. farinae), CR (American Cockroach), Grass (Bermuda grass pollen), Dog (Dog Epithelium), Cat (Cat pelt), Weed, Smut (Sporobolus indicus), M (Penicillium notatum, Aspergillus niger, Drechslera, Cladosprium spharospermum, Alternaria), manufactured by allertech, Australia. Histamine dihy- drochloride (10 mg/mL) was used as positive control and normal saline (0.9% w/v) was used as negative control. A mean wheal 3 mm in diameter larger than the negative control (diluents) was considered to be positive. In par- allel, blood samples (5 mL) were collected from all indi- viduals and the serum was stored at –20˚C. 2.5. Measurement of Specific IgE IgE reactivity to a panal of proteins from Df and rDer f2 was determined by ELISA [5]. Briefly, dilute each allergen in coating buffer (50 nM carbonate/bicarbonate buffer) at concentration of 1000 ng/mL Two-hundred l of each allergen was coated in each well of 96-well poly polystyrene microtiter wells (NuncTM, Denmark) and incubated at 4˚C overnight. The blocking buffer was added into each well and incubated at 37˚C for 60 min. The sera at dilution of 1: 10 was added into the well and incubated at 37˚C for 120 min. biotinylated-labeled mouse anti-human IgE antibody (SouthernBiotech, Bir- mingham, USA) at dil 1: 1000 was added into each well and incubated at 37˚C for 60 min. During each step, the plates were washed with PBs-Tween20 for 5 times. The plates was added with streptavidin-peroxidase solution at dil 1: 1000 and incubated at 37˚C for 60 min. The color reaction was developed by adding ABTS® peroxidase substrate (KPL, USA). Absorbance of IgE antibody was measurced at OD405nm with a Wallac 1420 microplate reader (Auto DELFIA Wallac 1420; Wallac, Turku, Fin- land). 2.6. Cell Culture PBMC dissolved in AIM-V medium seeded into 12-well plates at 1 × 106 cells/mL per well were stimu- lated with 100 µL allergen extracts (30 µg) (Df and rDer f), mitogens (PHA), or medium alone and then incubated at 37˚C in 5% CO2. The cells were harvested using cen- trifugation at 250 × g for 15 min 4˚C at 1, 3, 5 and 7 days post-incubation. The supernatants and the cell pel- lets were frozen at –80˚C until required. 2.7. Enzyme-Linked Immunosorbent Assay (ELISA) The concentration of IL-5, IFN-γ and TGF- in the supernatant were measured with ELISA Ready-SET-Go kits (eBioscience, Minneapolis, MN) according to man- ufacturer instructions using an ELISA reader (Auto DELFIA Wallac 1420; Wallac, Turku, Finland). All as- says were performed in two independent experiments. The concentration was calculated using a linear-regres- sion equation obtained from the standard absorbance values. 2.8. Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) The total RNA was extracted from the cell pellets using TRI Reagent (Molecular research center, USA) ac- cording with the manufacturer’s instructions. The total RNA (1 µg) was incubated at 45˚C for 60 min using the first-strand cDNA synthesis kit (Intron Biotechnology, Korea) to prepare the cDNA. The primer sequences were as follows: IL-5, 5’-GAG GAT GCT TCT GCA TTT GAG TTT-3’ and 5’-GTC AAT GTA TTT CTT TAT TAA GGA CAA-3’; IFN- , 5’-AGC TCT GCA TCG TTT GGG TTC-3’ and 5’-GTT GGC CCC TGA GAT AAA GCC-3’; TGF- , 5’-ACC ACT GCC GCA CAA CTC CGG TGA C-3’ and 5’-ATC TAT GAC AAG TTC AAG CAG AGT A-3’; β-Actin, 5’-ATC TGG CAC ACT TCT ACA-3’ and 5’-GTT TCG TGG ATG CCA CAG GAC-3’. PCR was carried out with an initial denatura- tion at 95 for 5 min for 5 min, then 35 cycles of denatu- ration at 95 for 30 sec, annealing at 55 for 30 sec, exten- sion at 72 for 30 sec and final exten- sion at 72 for 10 min. β-Actin was used as an internal control for each PCR reaction. The final PCR products were separated on 1% agarose gels and then visualized by ethidium bromide staining. 2.9. Statistical Analysis Data were expressed as the means (±SEM). The sta- tistical differences were analyzed using the Mann- Whitney U-test in the SPSS statistical software package (Version 13 Chicago, IL, USA). A significant value was defined as p < 0.05. 3. RESULTS 3.1. Subject Characteristics The demographic and clinical characteristics of the study subjects (Tabl e 1 ) were distributed into two groups according to SPT positivity to commercial HDM-total extract: 1) HDM+ group: patients with positive SPT to HDM-total; 2) HDM- group: Non-allergic subjects with negative SPT to HDM-total and aeroallergens. Rhinitis was the most frequent clinical diagnosis observed in HDM+ group but not be observed in HDM-group. The  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. http://www.scirp.org/journal/HEALTH/ 426 Table 1. Demographic and clinical characteristics of the study subject. Characteristics Groups HDM+ HDM- Number of subject (N) 24 20 Age (years, means ± SD) 35.17 ± 12.06 30.75 ± 5.46 Gender (male/female) Openly accessible at 10/14 9/11 Clinical diagnosis (N, %) 24, 100% 20, 100% Categorized by allergens (N, %) Der f, Der p, 9, 37.50% 0 Der f, Der p, CR, Dust, 6, 25.00% 0 Der f, Der p, CR, Dust, Smut 2, 8.33% 0 Der f, Der p, CR 2, 8.33% 0 Der f, Der p, CR, Weed 1, 4.17% 0 Der f, Der p, Cat, Dog 1, 4.17% 0 Der f, Der p, CR, Smut 1, 4.17% 0 Dust, Der f, Der p, CR, Dog 1, 4.17% 0 Dust, Der f, Der p, CR, Weed, Cat, Dog 1, 4.17% 0 HDM+; HDM-allergic subjects, HDM-; Non-allergic subjects, Dust; House dust, Der f; Dermatophagoides farina, Der p; Dermatophagoides ptero- nyssinus, CR; American Cockroach, Smut; Sporobolus indicus, Dog; Dog epithelium, Cat; Cat pelt. HDM+ group showed the mean wheal size to HDM-total and histamine dihydrochloride (positive control) were ≥ 3 mm. In contrast, all subjects did not show the mean wheal size to normal saline which was used as negative control. HDM-group showed a negative SPT to mite extracts as well as other aeroallergens tested according to the selection criteria used. The highest SPT was observing at 37.5% from patients suffering from two HDM-totals (Der f and Der p) whereas the least SPT was observing at 4.17% from patients suf- fering from two HDM-total and other aeroal lergens. 3.2. T Cell Responses to Df and rDer f2 Allergens at Molecular Level IL-5, IFN- , TGF- cytokine genes from allergic pa- tients and control subjects were stimulated with PHA, Df, rDer f2, pPICZ and Medium alone by RT-PCR. The re- sults revealed that PHA, Df, rDer f2, pPICZ and Me- dium alone induced IL-5,and IFN- genes in both al- lergic patients and control subjects. In contrast, PHA, Df, rDer f2 pPICZ and Medium alone did not induce TGF- gene in either allergic patients or control subjects (Fig- ure 1). It was suggesting that IL-5, IFN- , TGF- genes from allergic patients were similar to those from non-allergic subjects at molecular level. 3.3. T Cell Responses to Df and rDer F2 Allergens at Cellular Level IL-5, IFN- , TGF- cytokine protein production from allergic patients and control subjects were stimulated with PHA, Df and rDer f2 by ELISA. For allergic pa- tients, PHA, Df and rDer f2 induced IL-5 production at 217.76 ± 27.84, 7.47 ± 0.61 and 58.33 ± 4.92 pg/mL, respectively. For non-allergic subjects, PHA, Df and rDer f2 induced IL-5 production at 165.50 ± 16.61, 4.43 ± 0.174 and 6.31 ± 0.85 pg/mL, respectively (Ta b l e 2 ). Correlation between PHA and rDer f2 were found in allergic patients (r = 0.253; p < 0.05) but not found in non-allergic subjects (Figure 2). No correlation between PHA and Df were found in allergic patients and non-allergic subjects (data not shown). For allergic pa- (a) (b) Figure 1. IL-5, IFN- and TGF- gene expression to PHA, Df, rDer f2, pPICZ and medium com- pared with -actin house keeping gene in PBMC of allergic patients (a) and control subjects (b). (a) Allergic patients, (b) Control subjects.  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 427 (a) (b) Figure 2 Correlation of IL-5 production of PBMCs from HDM-allergic patients (a) and Non-allergic subjects (b) to PHA and rDer f2 (r = 0.253; p < 0.05). (a) HDM-allergic patients, (b) Non-allergic subjects. tients, PHA, Df and rDer f2 induced IFN- production at 863.98 ± 67.78, 70.32 ± 6.74 and 619.62 ± 61.43 pg/mL, respectively. For non-allergic subjects, PHA, Df and rDer f2 induced IFN- production at 1142.61 ± 78.40, 6.16 ± 0.45 and 410.73 ± 48.56 pg/mL, respectively. No correlation between PHA and Df as well as PHA and rDer f2 was found in allergic patients and non-allergic subjects (data not shown). For allergic patients and non-allergic subjects, PHA, Df and rDer f2 showed level of TGF- from PBMC of allergic patients and non-al- lergic subjects at <60 pg/m (Table 2). To analyze the effect on Th1/Th2 bias the responses the allergic patients and non-allergic subjects, the data showed that the cytokine release to PHA did not differ from allergic patients and non-allergic subjects. The Df allergen showed IFN- /IL-5 ratio from allergic patients (7.16 ± 0.70) higher than non-allergic subjects (1.43 ± 0.1), suggesting that Df allergen slightly induced Th1/ Th2 bias in allergic patients, but not good enough for non-allergic patients. The reverse rDer f2 allergen sho- wed IFN- /IL-5 ratio from non-allergic subjects (53.57 ± 9.71) higher than allergic patients (11.25 ± 1.08), sug- gesting that rDer f2 induced Th1/Th2 bias in non-al- lergic subjects better than allergic patients. 3.4. Specific IgE Reactivity to Df and rDer f2 Allergens Level of specific IgE from allergic patients and non-allergic subjects to Df and rDer f2 were measured by ELISA. As shown in Table 3, of 24 allergic pa- tients who had been SPT positivity to commercial HDM-total extract, only 4 patients (No. 3, 5, 6 and 7) showed specific IgE to both Df and rDer f2. Only 5 pa- tients (No. 2, 11, 14, 15 and 16) showed IgE binding to Df whereas no patient showed specific IgE to rDer f2. Fifteen patients showed specific IgE values below 0.35 kUA/L to Df and rDer f2. It was suggesting that the SPT positivity to commercial HDM-total extract was not related to IgE-binding reactivity to HDM allergens in al- lergic patients. Of 20 non-allergic subjects, all subjects showed specific IgE values below 0.35 kUA/L to Df and rDer f2 (data not shown). It was suggesting that the SPT negatively to commercial HDM-total extract was related to specific IgE reactivity to HDM allergens in non-al- lergic subjects. No correlation between the level of IL-5 production and the degree of IgE-binding to the rDer f2 from HDM-allergic patients and non-allergic subjects were observed (Figure 3). Table 2. Cy tokine protein responses to the PHA and house dust mite allergens from HDM-allergic and non-allergic subjects*. IL-5 (pg/mL) IFN- (pg/mL) TGF- (pg/mL) IFN- /IL-5 ratio Allergic Non-allergic Allergic Non-allergic Allergic Non-allergic Allergic Non-allergic PHA 217.76 ± 27.84 165.50 ± 16.61 863.98 ± 67.781142.61 ± 78.40<60.00 <60.00 6.83 ± 1.49 10.06 ± 2.98 Df 7.47 ± 0.61‡ 4.43 ± 0.174 70.32 ± 6.74†‡ 6.16 ± 0.45‡ <60.00 <60.00 7.16 ± 0.70† 1.43 ± 0.12‡ rDer f2 58.33 ± 4.92† 6.31 ± 0.85 619.62 ± 61.43410.7 ± 48.56 <60.00 <60.00 11.25 ± 1.08† 53.57 ± 9.71 *Results are presented as means (±SEM), † Significant differences between Allergic Non-allergic groups. ‡ Significant differences between Df and rDer f2 allergens. Cut off of IL-5= 4 pg/mL, IFN- = 4 pg/mL and TGF- = 60 pg/mL.  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 428 Table 3. IgE-binding to HDM allergens in HDM-allergic patients. IgE –binding (kUA/L) No. SPT Allergic history Df rDer f2 1. + Dust, Der f, Der p, CR, Smut 11.24 3.42 2. + Der f, Der p 11.07 0.40 3. + Dust, Der f, Der p, CR, 6.09 3.40 4. + Dust, Der f, Der p, CR, Dog 5.27 3.18 5. + Der f, Der p, CR, Smut 5.74 <0.35 6. + Der f, Der p, Cat, Dog 5.09 <0.35 7. + Dust, Der f, Der p, CR, 3.39 <0.35 8. + Der f, Der p, CR, Weed 1.88 <0.35 9. + Dust, Der f, Der p, CR, 0.99 <0.35 10. + Der f, Der p, CR, Weed <0.35 <0.35 11. + Dust, Der f, Der p, CR, Smut <0.35 <0.35 12. + Dust, Der f, Der p, CR, <0.35 <0.35 13. + Dust, Der f, Der p, CR, <0.35 <0.35 14. + Dust, Der f, Der p, CR, <0.35 <0.35 15. + Der f, Der p, CR, <0.35 <0.35 16. + Der f, Der p, CR, <0.35 <0.35 17. + Der f, Der p <0.35 <0.35 18. + Der f, Der p <0.35 <0.35 19. + Der f, Der p <0.35 <0.35 20. + Der f, Der p <0.35 <0.35 21. + Der f, Der p <0.35 <0.35 22. + Der f, Der p <0.35 <0.35 23. + Der f, Der p <0.35 <0.35 24. + Der f, Der p <0.35 <0.35 *SPT, skin prick tests; +, SPT wheal response diameter was more than 3 mm; *Dust; House dust, Der f; Dermatophagoides farina, Der p; Dermatophagoides pteronyssinus, CR; American Cockroach, Smut; Sporobolus indicus, Dog; Dog epithelium, Cat; Cat pelt, *Cut off of IgE –binding; 0.35 kUA/L. (a) (b) Figure 3 No correla tion (r = 0.01) betw een the level of IL-5 production and the degree of IgE-binding to the rDer f2 from HDM-allergic patients (a) and Non-allergic subjects (b) were observed. (a) HDM-allergic patients; (b) Non-al- lergic subjects.  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 429 4. DISCUSSIONS House dust mites (HDMs) as a source of allergens and their contribution to allergic diseases, particularly asthma and rhinitis, have been recognized for many years [20]. Allergic rhinitis is an inflammatory reaction of the nasal mucosa, in consequence of an IgE mediated hypersensi- tive reaction to inhaling allergens, involving different mediators and cytokine cells [21]. Positive skin tests and/or serum IgE antibodies to HDM have been widely demonstrated in genetically predisposed individuals. In the present study, we found only 37.5 % allergic patients presenting positive SPT to both mites (Df and Dp), while 62.5 % of allergic patients sensitized to a panel of aero- allergen. These results were similar to those of our pre- vious studies carried out in another group of allergic patients from Police hospital in Bangkok [2], confirming that the high rate of this concurrent sensitization has certainly complicated the evaluation of the role of D. farinae and D. pteronyssinus in these patients, particu- larly in tropical and subtropical regions where both mites coexist. Owing to glycosylated antigens have been shown to play a crucial role in different pathologies, particularly in fungal infections and allergic diseases [20]. In this context, Df-total extract was fractioned by SDS-PAGE and confirmed by Western blot analysis us- ing 1D8 monoclonal antibody. The recombinant Der f2 allergen derived from P. pastoris was also fractioned by SDS-PAGE and confirmed by Western blot analysis. The recombinant Der f2 allergens presented predominantly molecular weight at 14 kDa. Both allergens were used to detect IgE antibody in allergic patients and healthy sub- jects. We found levels of specific IgE antibody detected by Df extract were higher than those by recombinant Der f2 allergen in allergic patients. These results are consis- tent with report of Almedida et al. [22] and Pipatchaipai- san, [2]. It is implied that specific IgE antibody could be related to natural allergen exposure, thus reflecting a normal consequence of immediate hypersensitivity reac- tions in allergic patients in vivo [22]. In our data, we found that IgE are preferentially involved in this cross- reactivity in some allergic patients to both Df extract and recombinant Der f2 allergen. This result indicated that IgE might be recognizing same epitope in the extract allergen and recombinant allergen. Several reports revealed that both the IgE-dependent early response and antigen-primed Th2 cells are neces- sary for a persistent atopic inflammation characterized by the accumulation of activated inflammatory cells [23]. Previous studies have highlighted the role of IL-5 in the development of the chronic phase of atopic inflamma- tion and in the expression of allergic diseases [24-26]. The hypothesis of our study was that immunotherapy may induce the functional modification from Th2 to Th1 phenotype in PBMC. To investigate the modifications of cellular immunity in the mechanism of HDM allergens, we evaluated intracellular IL-5, and IFN-γ gene expres- sion as well as production from the PBMC of the allergic patients relative to healthy subjects. We did not find sig- nificantly difference in IL-5 or IFN-γ gene expression from PBMC of allergic patients and healthy control sub- jects. This data is consistent with other investigators [21]. However, we found that IL-5 production induced by Df extract was slightly positively correlated in both allergic patients and healthy subjects. On the other hand, we found that IL-5 production induced by recombinant Der f2 allergen was significantly increased in allergic pa- tients relative to healthy subject. This data was consis- tent with the evidence that activated T cells and the Th2 cytokine IL-5 production is increased in lung of atopic asthmatic subjects [24,27,28]. We found no correlation between serum HDM-specific IgE levels and IL-5 pro- duction stimulated in either allergic patients or healthy subjects. This is agreement with data from some but not all studies [6,10,29]. Investigations of allergen-simulated release of IFN- from PBMC have produced mixed results. Some studies found decreased IFN- production in subjects with atopic diseases relative to healthy control subjects [14,30,31], whereas other studies reported no difference [32,33]. In our study, there was no significant difference in recombinant Der f2-stimulated IFN- production be- tween allergic patients and control subjects, while we found that degree of Df-total extract-stimulated IFN- production was higher in allergic patients than in the control subjects. It has been reported that IFN- produc- tion closely correlated with atopic dermatitis in infants [10]. No absolute definition of a Th1- or Th2-type cyto- kine response was demonstrated. An excess of Th2 cyto- kines relative to the Th1 cytokine is implicated in the cause of atopy [34,35]. Studies with PBMC have also analyzed allergen-stimulated cytokine production as the amount of IL-5, Th2 cytokine relative to IFN- , Th1 cytokine [30]. We analyzed cytokine production induced by HDM allergens as the ratio of the IL-5 to IFN- pro- duction in each culture that had a positive response to the stimulators and expressed this ratio as a Th2/ Th1cytokine index. We found that for allergic patients and control subjects, the Th2/Th1cytokine index was induced by both HDM allergens, although different de gree of Th2/Th1cytokine index was observed, suggest- ing that HDM is the Th2-type stimulators that are con- sistent with other reports [36]. Additionally, we found that there is a lower frequency of HDM allergen-re- sponsive T cells in healthy control subjects than in aller- gic patients. Evidence of our data focuses research atten-  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 430 tion on mechanisms of T-cell recognition of, and activa- tion by, HDM allergens. It is concluded that both aller- gic patients and normal subjects had a Th2-type cytokine response to HDM allergen; our data does suggest that patients with atopic asthma have an enhanced Th2 cyto- kine response to HDM allergen relative to healthy con- trol subjects. Therefore, both HDM allergens increased IL-5 production and Th2/Th1cytokine index in patients with allergic rhinitis compared with normal subjects. 5. CONCLUSIONS The major findings of this study are as follows. First, PBMC from allergic patients with allergic rhinitis and healthy control subjects have the Th2-type cytokine re- sponse to HDM allergens. Second, allergic patients do have an enhanced Th2-type cytokine response to HDM compared with control subjects. These data indicate that using of both HDM allergens in immunotherapeutic procedures in allergic patients and healthy subjects can- not be recommended. 6. ACKNOWLEDGEMENTS This study was supported by the Thailand Research Funding No. MRG-WII 525S092 and a partial funding from TRF No. MRG- -WII505S061. This study was also supported by Grants No. RGP- 2552-06 from Faculty of Science, Silpakorn University The authors would like to thank the patients and nurses from Department of Oto- laryngology, Pramongkutklao Hospital, Bangkok. We also thank the students from Silpakorn University. Furthermore, we thanks Associate Professor Dr. Darawan Wanachiwanawin, Department of Parasitology, Faculty of Medicine Siriraj Hospital, Mahidol University for labora- tory facility. REFERENCES [1] Thomas, W.R., Smith, W.A., Hales, B.J., Mills, K.L. and O’Brien, R.M. (2002) Characterization and immunobi- ology of house dust mite allergens. International Ar- chives of Allergy and Immunology, 129, 1-18. doi:10.1159/000065179 [2] Phiphatchaipaisarn, R., Rabablert, J., Bramarapravati, K., Thongdee, D., Wongpitoon, N., Durongpisitkul, W. and Malainual, N. (2010) Development of time-resolved im- munofluorometric assays for the detection of house dust mite-allergic IgE in human sera. Health, 2, 1280-1286. doi:10.4236/health.2010.211190 [3] Hales, B.J., Shen, H. and Thomas, W.R., (2000) Cytokine responses to Der p 1 and Der p 7: House dust mite aller- gens with different IgE-binding activities. Clinical & Experimental Allergy, 30, 934-943. doi:10.1046/j.1365-2222.2000.00901.x [4] Piboonpocanun, S., Malainual, N., Jirapongsananuruk, O., Vichyanond, P. and Thomas, W.R. (2006) Genetic poly- morphisms of major house dust mite allergens. Clinical & Experimental Allergy, 36, 510-516. doi:10.1111/j.1365-2222.2006.02464.x [5] Hales, B.J., Hazell, L.A., Smith, W. and Thomas, W.R. (2002) Genetic variation of Der p 2 allergens: effects on T cell responses and immunoglobulin E binding. Clinical & Experimental Allergy, 32, 1461-1467. doi:10.1046/j.1365-2745.2002.01500.x [6] Till, S., (1997) Immunotherapy: Readdressing the bal- ance between TH2 and TH1 cells. Clinical & Experi- mental Allergy. 27, 1007-1015. doi:10.1111/j.1365-2222.1997.tb01244.x [7] Rudin, A., Macaubas, C., Wee, C., Holt, B.J., Slya, P.D. and Holt, P.G., (2001) “Bystander” amplification of PBMC cytokine responses to seasonal allergen in poly- sensitized atopic children. Allergy, 56, 1042-1048. doi:10.1034/j.1398-9995.2001.00991.x [8] Romagnani, S. (2000) The role of lymphocytes in aller- gic disease. Journal of Allergy and Clinical Immunology, 105, 399-408. doi:10.1067/mai.2000.104575 [9] Romagnani, S. (2000) T-cell subsets (Th1 versus Th2). Annals of Allergy, Asthma & Immunology, 85, 9-18. doi:10.1016/S1081-1206(10)62426-X [10] Kimura, M., Tsuruta, S. and Yoshida, T., (1998) Unique profile of IL-4 and IFN-gamma production by peripheral blood mononuclear cells in infants with atopic dermatitis. Journal of Allergy and Clinical Immunology, 102 , 238- 244. doi:10.1016/S0091-6749(98)70092-2 [11] Liu, L., Jarjour, N.N., Busse, W.W. and Kelly, E.A. (2004) Enhanced generation of helper T type 1 and 2 chemoki- nes in allergen-induced asthma. American Journal of Respiratory and Critical Care Medicine, 169, 1118-1124. doi:10.1164/rccm.200312-1659OC [12] Sugimoto, T., Ishikawa, Y., Yoshimoto, T., Hayashi, N., Fujimoto, J. and Nakanishi, K. (2004) Interleukin 18 acts on memory T helper cells type 1 to induce airway in- flammation and hyperresponsiveness in a naive host mouse. The Journal of Experimental Medicine, 199, 595- 545. doi:10.1084/jem.20031368 [13] Letterio, J.J. and Roberts, A.B. (1998) Regulation of immune responses by TGF-beta. Annual Review of Im- munology, 16, 137-161. doi:10.1146/annurev.immunol.16.1.137 [14] Mello, L.M., Bechara, M.I., Solé, D. and Rodrigues, V. (2009) TH1/TH2 balance in concomitant immediate and delayed-type hypersensitivity diseases. Immunology Let- ters, 124, 88-94. doi:10.1016/j.imlet.2009.04.011 [15] Grammer, L.C., Ditto, A.M., Tripathi, A. and Harris, K.E, (2002) Prevalence and onset of rhinitis and con- junctivi- tis in subjects with occupational asthma caused by tri- mellitic anhydride (TMA). Journal of Occupational and Environmental Medicine, 44, 1179-1181. doi:10.1097/00043764-200212000-00013 [16] Tripathi, A. and Grammer, L.C., (2001) Extrinsic allergic alveolitis from a proteolytic enzyme. Annals of Allergy, Asthma & Immunology, 86, 425-427. doi:10.1016/S1081-1206(10)62489-1 [17] Mamoni, R.L. and Blotta, M.H., (2005) Kinetics of cyto- kines and chemokines gene expression distinguishes Pa- racoccidioides brasiliensis infection from disease. Cy- tokine, 32, 20-29. doi:10.1016/j.cyto.2005.07.006 [18] Chapman, M.D., Heymann, P.W., Wilkins, S.R., Brown, M.J. and Platts-Mills, T.A. (1987) Monoclonal immuno- assays for major dust mite (Dermatophagoides) allergens,  D. Thongdee et al. / Health 3 (2011) 423-431 Copyright © 2011 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 431 Der p I and Der f I, and quantitative analysis of the aller- gen content of mite and house dust extracts. Journal of Allergy and Clinical Immunology, 80, 184-194. doi:10.1016/0091-6749(87)90128-X [19] Tanyaratsrisakul, S., Malainual, N., Jirapongsananuruk, O., Smith, W.A., Thomas, W.R. and Piboonpocanun, S. (2009) Structural and IgE binding analyses of recom- bi- nant der p 2 expressed from the hosts escherichia coli and pichia pastoris. International Archives of Allergy and Immunology, 29, 190-198. doi:10.1159/000242356 [20] Alves, R., Silva, D.A., Fernandes, J.F., Almeida, K.C., Ynoue, L.H., Bernardes, C.T., Moreira, P.F., Gen- nari-Cardoso, M.L., Sung, S.J. and Taketomi, E.A. (2008) Humoral and cellular immune responses to Blomia trop- icalis and concanavalin A-binding fractions in atopic pa- tients. Brazilian Journal of Medical Biological Research, 41, 773-781. doi:10.1590/S0100-879X2008000900006 [21] Silva, T.M., Guimarães, R.E., Nascimento, E., Becker, H.M., Araújo, R.N. and Nunes, F.B. (2009) RT-PCR cy- tokine study in patients with allergic rhinitis. Brazilian Journal of Otorhinolaryngology, 75, 24-29. doi:10.1590/S0034-72992009000100004 [22] Almeida, K.C., Silva, D.A., Gennari-Cardoso, M.L., Cunha-Júnior, J.P., Alves, R., Ynoue, L.H., Resende, R.O., Sung, S.J. and Taketomi, E.A. (2006) Responses of IgE, IgG1, and IgG4 to concanavalin A-binding Blomia tropicalis antigens in allergic patients. Brazilian Journal of Medical Biological Research, 39, 1445-1454. [23] O’Byrne, P.M. and Wood, L. (1999) Interleukin-5 and allergic inflammation. Clinical & Experimental Allergy, 29, 573-575. doi:10.1046/j.1365-2222.1999.00556.x [24] Weber-Chrysochoou, C., Crisafulli, D., Almqvist, C., Li, Q., Kemp, A.S., Britton, W.J. and Marks, G.B. (2007) IL-5 T-cell responses to house dust mite are associated with the development of allergen-specific IgE responses and asthma in the first 5 years of life. Journal of Allergy and Clinical Immunology, 120, 286-292. doi:10.1016/j.jaci.2007.06.034 [25] Kim, H.B., Jin, H.S., et al. (2009) The effect of rush immuno-therapy with house dust mite in the production of IL-5 and IFN-gamma from the peripheral blood T cells of asthmatic children. Journal of Korean Medical Scien- ce, 24, 392-397. doi:10.3346/jkms.2009.24.3.392 [26] Kimura, M., Okafuji, I. and Yoshida, T. (2003) Theophyl- line suppresses IL-5 and IL-13 production, and lympho- cyte proliferation upon stimulation with house dust mite in asthmatic children. International Archives of Allergy and Immunology, 131, 189-194. doi:10.1159/000071485 [27] Krug, N., Jung, T., Napp, U., Wagner, K., Schultze-Wern- inghaus, G., Heusser, C., Rieger, C.H., Schauer, U. and Fabel, H. (1998) Frequencies of T cells expressing inter leukin-4 and interleukin-5 in atopic asthmatic children. Comparison with atopic asthmatic adults. American Journal of Respiratory and Critical Care Medicine, 158, 754-759. [28] Olivenstein, R., Taha, R., Minshall, E.M. and Hamid, Q.A. (1999) IL-4 and IL-5 mRNA expression in induced sputum of asthmatic subjects: comparison with bronchial wash. Journal of Allergy and Clinical Immunology, 103, 238-245. doi:10.1016/S0091-6749(99)70497-5 [29] Würtzen, P.A., van Neerven, R.J., Arnved, J., Ipsen, H., Sparholt, S.H. (1998) Dissection of the grass aller- gen-specific immune response in patients with allergies and control subjects: T-cell proliferation in patients does not correlate with specific serum IgE and skin reactivity. Journal of Allergy and Clinical Immunology, 101 , 241- 249. doi:10.1016/S0091-6749(98)70389-6 [30] Matsui, E., Kaneko, H., Teramoto, T., Fukao, T., Inoue, R., Kasahara, K., Takemura, M., Seishima, M. and Kon- do, N. (2000) Reduced IFNgamma production in re- sponse to IL-12 stimulation and/or reduced IL-12 pro- duction in atopic patients. Clin Exp Allergy, 30, 1250- 1256. doi:10.1046/j.1365-2222.2000.00931.x [31] Yamaguchi, T., Soma, T., Takaku, Y., Nakagome, K., Hagiwara, K., Kanazawa, M. and Nagata, M. (2010) Salbutamol modulates the balance of Th1 and Th2 cyto- kines by mononuclear cells from allergic asthmatics. In- ternational Archives of Allergy and Immunology, 152, 32-40. doi:10.1159/000312123 [32] Kimura, M., Tsuruta, S. and Yoshida, T. (2000) IL-4 pro- duction by PBMCs on stimulation with mite allergen is correlated with the level of serum IgE antibody against mite in children with bronchial asthma. Journal of Al- lergy and Clinical Immunology, 105, 327-332. doi:10.1016/S0091-6749(00)90083-6 [33] Bullens, D.M., De Swerdt, A., Dilissen, E., Kasran, A., Kroczek, R.A., Cadot, P., Casaer, P. and Ceuppens, J.L. (2005) House dust mite-specific T cells in healthy non- atopic children. Clinical & Experimental Allergy, 35, 1535-1541. doi:10.1111/j.1365-2222.2005.02352.x [34] Yazdanbakhsh, M., van den Biggelaar, A. and Maizels R.M. (2001) Th2 responses without atopy: Immunoregu- lation in chronic helminth infections and reduced allergic disease. Trends in Immunology, 22 , 372-377. doi:10.1016/S1471-4906(01)01958-5 [35] Ling, E.M., Smith, T., Nguyen, X.D., Pridgeon, C., Dallman, M., Arbery, J., Carr, V.A. and Robinson, D.S. (2004) Relation of CD4+CD25+ regulatory T-cell sup- pression of allergen-driven T-cell activation to atopic status and expression of allergic disease. Lancet, 363, 608-615. doi:10.1016/S0140-6736(04)15592-X [36] Duramad, P., Tager, I.B., Leikauf, J., Eskenazi, B. and Holland, N.T. (2006) Expression of Th1/Th2 cytokines in human blood after in vitro treatment with chlorpyrifos, and its metabolites, in combination with endotoxin LPS and allergen Der p1. Journal of Applied Toxicology, 26, 458-465. doi:10.1002/jat.1162
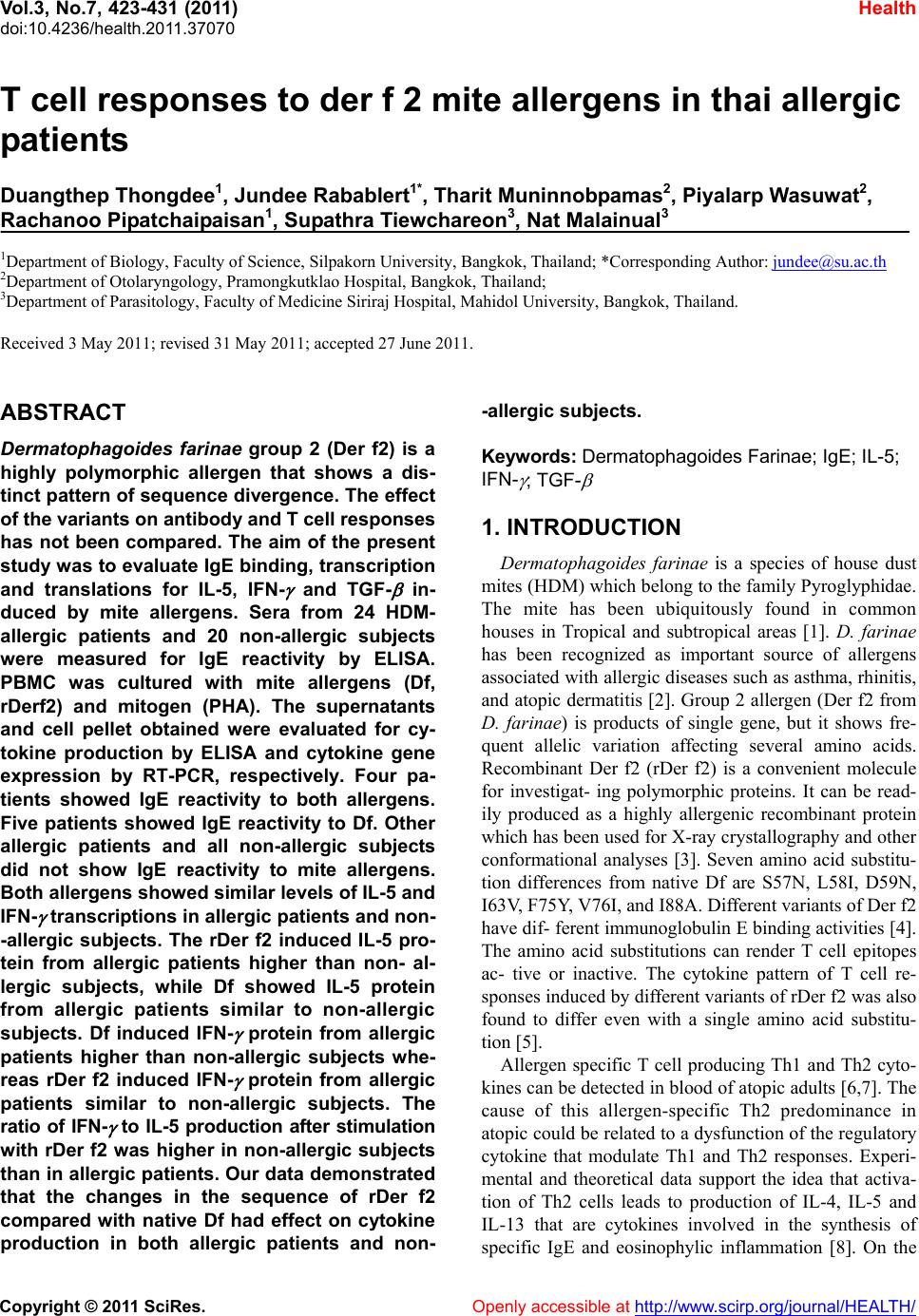
|