210 S. A. FANAEI ET AL.
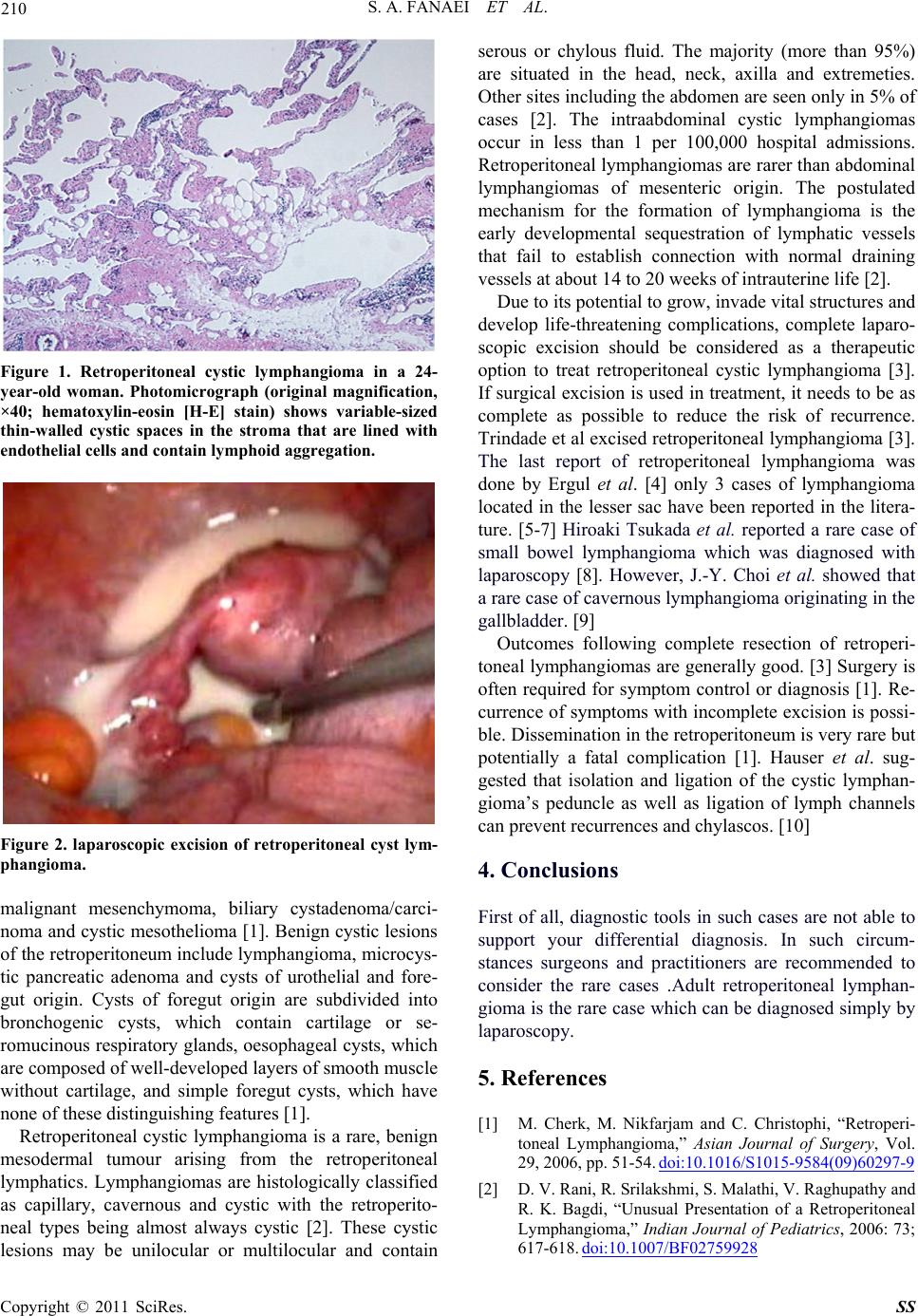
Figure 1. Retroperitoneal cystic lymphangioma in a 24-
year-old woman. Photomicrograph (original magnification,
×40; hematoxylin-eosin [H-E] stain) shows variable-sized
thin-walled cystic spaces in the stroma that are lined with
endothelial cells and contain lymphoid aggregation.
Figure 2. laparoscopic excision of retroperitoneal cyst lym-
phangioma.
malignant mesenchymoma, biliary cystadenoma/carci-
noma and cystic mesothelioma [1]. Benign cystic lesions
of the retroperitoneum include lymphangioma, microcys-
tic pancreatic adenoma and cysts of urothelial and fore-
gut origin. Cysts of foregut origin are subdivided into
bronchogenic cysts, which contain cartilage or se-
romucinous respirator y glands, oesophageal cysts, which
are composed of wel l -developed laye rs o f s mooth muscle
without cartilage, and simple foregut cysts, which have
none of these distingui s hi ng features [1].
Retroperitoneal cystic lymphangioma is a rare, benign
mesodermal tumour arising from the retroperitoneal
lymphatics. Lymphangiomas are histologically classified
as capillary, cavernous and cystic with the retroperito-
neal types being almost always cystic [2]. These cystic
lesions may be unilocular or multilocular and contain
serous or chylous fluid. The majority (more than 95%)
are situated in the head, neck, axilla and extremeties.
Other sites including the abdomen are seen only in 5% of
cases [2]. The intraabdominal cystic lymphangiomas
occur in less than 1 per 100,000 hospital admissions.
Retroperitoneal lymphangiomas are rarer than abdominal
lymphangiomas of mesenteric origin. The postulated
mechanism for the formation of lymphangioma is the
early developmental sequestration of lymphatic vessels
that fail to establish connection with normal draining
vessels at about 14 to 20 weeks of intrauterine life [2].
Due to its potential to grow, invade vital structures and
develop life-threatening complications, complete laparo-
scopic excision should be considered as a therapeutic
option to treat retroperitoneal cystic lymphangioma [3].
If surgical excision is u sed in treatment, it needs to be as
complete as possible to reduce the risk of recurrence.
Trindade et al excised retroperitoneal lymphangioma [3].
The last report of retroperitoneal lymphangioma was
done by Ergul et al. [4] only 3 cases of lymphangioma
located in the lesser sac have been reported in the litera-
ture. [5-7] Hiroaki Tsukada et al. reported a rare case of
small bowel lymphangioma which was diagnosed with
laparoscopy [8]. However, J.-Y. Choi et al. showed that
a rare case of cavernous lymphang io ma origin ating in the
gallbladder. [9]
Outcomes following complete resection of retroperi-
toneal lymphangiomas are generally good. [3] Surgery is
often required for symptom control or diagnosis [1]. Re-
currence of symptoms with incomplete excision is possi-
ble. Dissemination in the retroperitoneum is very rare but
potentially a fatal complication [1]. Hauser et al. sug-
gested that isolation and ligation of the cystic lymphan-
gioma’s peduncle as well as ligation of lymph channels
can prevent recurrences and chylascos. [10]
4. Conclusions
First of all, diagnostic tools in such cases are not able to
support your differential diagnosis. In such circum-
stances surgeons and practitioners are recommended to
consider the rare cases .Adult retroperitoneal lymphan-
gioma is the rare case which can be diagnosed simply by
laparoscopy.
5. References
[1] M. Cherk, M. Nikfarjam and C. Christophi, “Retroperi-
toneal Lymphangioma,” Asian Journal of Surgery, Vol.
29, 2006, pp. 51-54. doi:10.1016/S1015-9584(09)60297-9
[2] D. V. Rani, R. Srilakshmi, S. Malathi, V. Raghupathy and
R. K. Bagdi, “Unusual Presentation of a Retroperitoneal
Lymphangioma,” Indian Journal of Pediatrics, 2006: 73;
617-618. doi:10.1007/BF02759928
Copyright © 2011 SciRes. SS