B. Enya et al. / Health 3 (2011) 362-365
Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/
364
tivity among rural-urban dwellers did not establish any
significance (p = 0.416).
4. DISCUSSION
In developing countries, the extent of maternal rubella
infection is largely unknown. There are very few clinical
records of rubella infection and or congenital rubella
syndrome (CRS). Clearly, the first step in determining an
appropriate immunization policy for a given population
is to carry out a serologic survey, in order to determine
the seroprevalence of rubella antibodies [7]. In Nigeria,
rubella vaccine is not a component of the routine immu-
nization policy despite its being safe, effective and could
be readily added to national immunization programme at
minimal extra cost.
Rubella outbreaks may continue to occur unnoticed in
highly unimmunized populations due to efficient trans-
mission of the virus among susceptible individuals [8].
This study shows that the incidence of rubella virus
among patients with febrile rash illness in Akwa Ibom
State, Nigeria is high and that the incidence varied con-
siderably between age groups, sex and community set-
tings (urban and rural). The incidence of 12% found in
this study is slightly lower than 17.5% reported in Adane
province Turkey [9], but higher than 8.6% reported in
another study in Sana’a, Yemen [10] and 3.4% reported
in Eastern Turkey [11]. The reason for the observed dif-
ferences may be attributed to geographical variations
and different levels of rubella immunization coverage.
The yearly rise observed in the incidence of rubella
IgM antibodies from 8.7% in 2006 to 14.3% in 2009
may be due to the introduction of rubella case-based
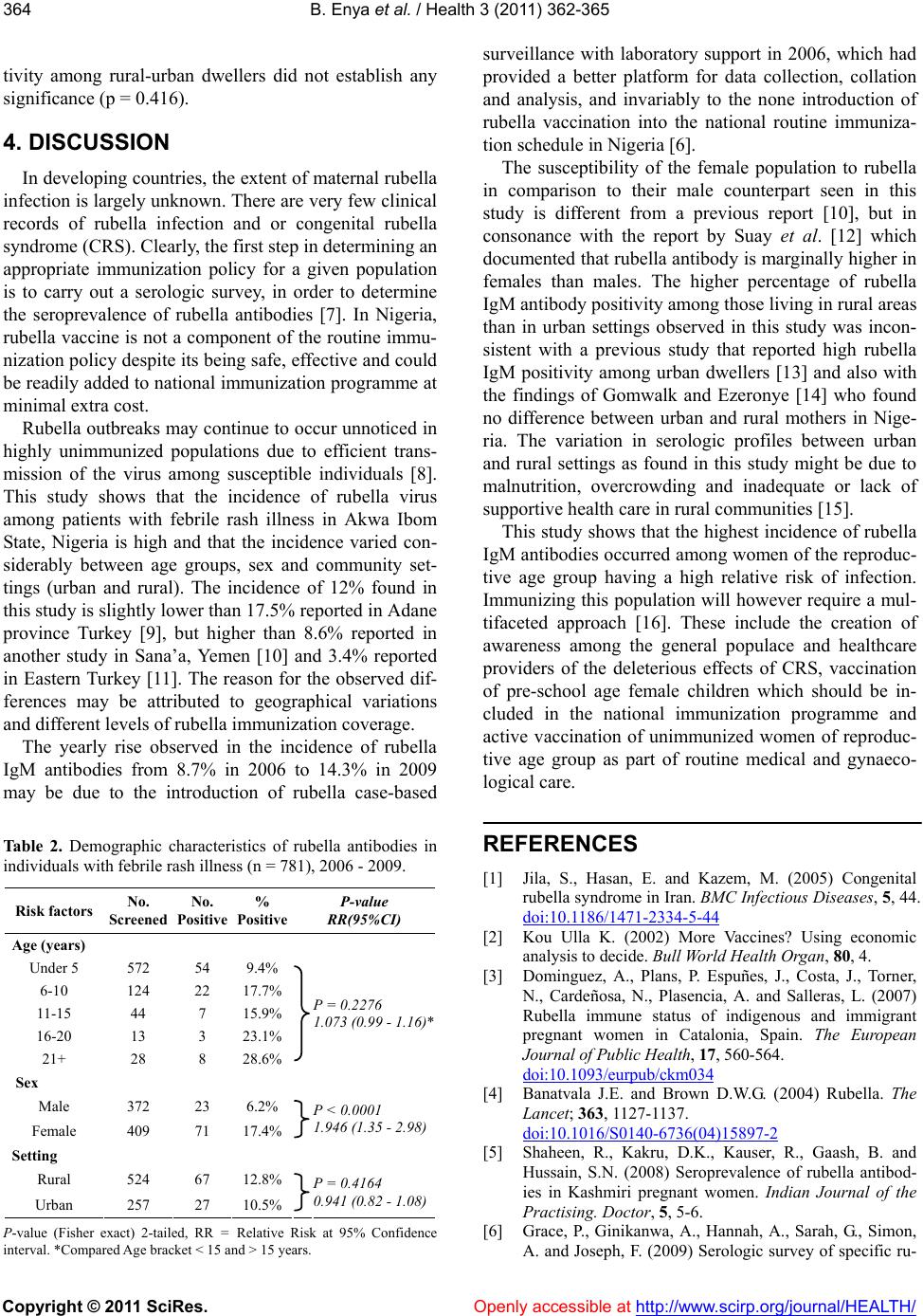
Table 2. Demographic characteristics of rubella antibodies in
individuals with febrile rash illness (n = 781), 2006 - 2009.
Risk factors No.
Screened No.
Positive %
Positive P-value
RR(95%CI)
Age (years)
Under 5 572 54 9.4%
6-10 124 22 17.7%
11-15 44 7 15.9%
16-20 13 3 23.1%
21+ 28 8 28.6%
P = 0.2276
1.073 (0.99 - 1.16)*
Sex
Male 372 23 6.2%
Female 409 71 17.4%
P < 0.0001
1.946 (1.35 - 2.98)
Setting
Rural 524 67 12.8%
Urban 257 27 10.5%
P = 0.4164
0.941 (0.82 - 1.08)
P-value (Fisher exact) 2-tailed, RR = Relative Risk at 95% Confidence
interval. *Compared Age bracket < 15 and > 15 years.
surveillance with laboratory support in 2006, which had
provided a better platform for data collection, collation
and analysis, and invariably to the none introduction of
rubella vaccination into the national routine immuniza-
tion schedule in Nigeria [6].
The susceptibility of the female population to rubella
in comparison to their male counterpart seen in this
study is different from a previous report [10], but in
consonance with the report by Suay et al. [12] which
documented that rubella antibody is marginally higher in
females than males. The higher percentage of rubella
IgM antibody positivity among those living in rural areas
than in urban settings observed in this study was incon-
sistent with a previous study that reported high rubella
IgM positivity among urban dwellers [13] and also with
the findings of Gomwalk and Ezeronye [14] who found
no difference between urban and rural mothers in Nige-
ria. The variation in serologic profiles between urban
and rural settings as found in this study might be due to
malnutrition, overcrowding and inadequate or lack of
supportive health care in rural communities [15].
This study shows that the highest incidence of rubella
IgM antibodies occurred among women of the reproduc-
tive age group having a high relative risk of infection.
Immunizing this population will however require a mul-
tifaceted approach [16]. These include the creation of
awareness among the general populace and healthcare
providers of the deleterious effects of CRS, vaccination
of pre-school age female children which should be in-
cluded in the national immunization programme and
active vaccination of unimmunized women of reproduc-
tive age group as part of routine medical and gynaeco-
logical care.
REFERENCES
[1] Jila, S., Hasan, E. and Kazem, M. (2005) Congenital
rubella syndrome in Iran. BMC Infectious Diseases, 5, 44.
doi:10.1186/1471-2334-5-44
[2] Kou Ulla K. (2002) More Vaccines? Using economic
analysis to decide. Bull World Health Organ, 80, 4.
[3] Dominguez, A., Plans, P. Espuñes, J., Costa, J., Torner,
N., Cardeñosa, N., Plasencia, A. and Salleras, L. (2007)
Rubella immune status of indigenous and immigrant
pregnant women in Catalonia, Spain. The European
Journal of Public Health, 17, 560-564.
doi:10.1093/eurpub/ckm034
[4] Banatvala J.E. and Brown D.W.G. (2004) Rubella. The
Lancet; 363, 1127-1137.
doi:10.1016/S0140-6736(04)15897-2
[5] Shaheen, R., Kakru, D.K., Kauser, R., Gaash, B. and
Hussain, S.N. (2008) Seroprevalence of rubella antibod-
ies in Kashmiri pregnant women. Indian Journal of the
Practising. Doctor, 5, 5-6.
[6] Grace, P., Ginikanwa, A., Hannah, A., Sarah, G., Simon,
A. and Joseph, F. (2009) Serologic survey of specific ru-