Health
Vol.6 No.6(2014), Article ID:43600,14 pages DOI:10.4236/health.2014.66071
Vascular Trauma in the Amazon Region: A Two Years Cases Review from a Single Institution*
Adenauer Marinho de Oliveira Góes Jr.#, Allan Dias Vasconcelos Rodrigues, Fábio Brito Braga, Mariseth Carvalho de Andrade, Simone de Campos Vieira Abib
Department of Surgery (CESUPA), Belém, Brazil
Email: #adenauer-junior@ibest.com.br
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 14 December 2013; revised 20 January 2014; accepted 30 January 2014
ABSTRACT
Introduction: Vascular injuries are among the main mechanisms of death in trauma. In Brazil, the general surgeon is in charge of emergencies procedures in most hospitals, but many times these surgeons are not familiarized with more complex vascular surgical techniques that often require a vascular surgeon. Pará State is the most populated one in the Brazilian Amazon region and a single hospital with vascular surgeons permanently on call is available. Objectives: To evaluate demographic data on vascular trauma victims; to establish the mechanism, anatomic location, injury pattern and surgical techniques used to manage the vascular lesions treated at the Metropolitan Emergency Hospital; to ascertain associated non-vascular injuries and victim’s clinical outcome. Methods: Medical records retrospective analysis of patients treated for vascular injuries from February 2011 to February 2013 at the institution in case. All arterial and venous injuries were analyzed. Patients who were not operated by the vascular surgery team, iatrogenic injuries and those who underwent primary or sustained traumatic amputation were excluded. Results: 173 cases; 95.95% were male; 54.90% were between 25 and 49 years; penetrating trauma mechanisms were found in 88.44%; lower limb was the most affected topography (41.50%); the most injured vessels were the superficial femoral and ulnar arteries (in 15.75% of cases each) and the superficial femoral vein (17.77%); autologous vein graft was the most performed technique for arterial repair (36.57%) and ligature was performed in 85.00% of venous trauma; amputation rate was 15.60% and mortality rate was 6.35%. Conclusions: Vascular injuries occurred predominantly in men from 24 to 49 years old; penetrating mechanisms were most frequent; lower limb was the most affected topography; the most frequently injured vessels were the ulnar and superficial femoral arteries and the superficial femoral vein; complete vessel transection was the most common injury pattern; arterial trauma was most frequently treated by autologous venous graft interposition and ligature was performed for most of venous injuries; fractures were the most common associated lesions; the majority of patients recovered uneventfully, ischemic and infectious complications were the most frequent ones; deaths were caused by hypovolemic and septic shocks.
Keywords:External Causes; Wounds and Injuries; Vascular System Injuries; Blood Vessels; Amazon

1. Introduction
Trauma due to violence and vehicle accidents represents the major cause of mortality and morbidity related to external causes all around the world [1] [2] . In Brazil, violence and vehicle accidents are more frequent on urban areas, which concentrate around 75% of violent causes of death [3] .
According to the Brazilian Public Health System, hospitalization due to traumas had a near 30% increase in the last 5 years [4] .
Vascular injuries are among the most frequent death mechanisms on traumatized patients [5] , representing a considerable demand on civilian and military hospitals [6] -[9] .
Vascular injuries mechanisms can be classified into blunt, as vehicle accidents, and penetrating, as firearms projectile wounds [10] . Many studies have shown that penetrating mechanisms prevail and that lower limbs are the most frequent sites of injury [11] -[15] .
A Brazilian cardiovascular trauma study, which analyzed cases from 1998 to 2005, showed that 45.1% of injuries were due to firearms projectiles and 30.8% due to blades or glass, 23.2% were blunt traumas and 1.1% were iatrogenic injuries. This paper presented a 75% peripheral injury incidence with a 38.4% lower limb rate [16] .
Blunt trauma usually carries worse prognosis because of the high kinetic energy that is involved in motor vehicle accidents and falls from great high [17] and also the fact that as external bleeding is commonly absent, there can be no obvious sing of vascular trauma at the initial evaluation of the multi injured patient [18] .
Limb amputation rate related to vascular lesions differs for penetrating (10%) and blunt trauma (30%) [19] .
Concomitants non-vascular injuries are frequent. Fractures, nerve and muscle injuries are the most common ones. These associations increase amputation probability [20] -[22] .
Irreversible striated muscle ischemia usually develops 6 hours after trauma [23] , but this period depends on the arterial injury anatomic location, trauma mechanism, collateral circulation, hemorrhagic shock severity and vessel spasm. In order to optimize functional outcome, limb revascularization must be undertaken before this interval [14] [24] .
According to the Brazilian Geographic and Statistic Institute, the Pará state is the second largest state in Brazil. It has a 1,247,954,666 km2 area (twice the territory of France), and is the most populated state in the Brazilian Amazon region; its capital, Belém, and surroundings concentrates a 2.1 million population [25] . A single trauma center with vascular surgeons permanently on duty is available statewide.
The Metropolitan Emergency Hospital, at Ananindeua (a city at the metropolitan area of Belém) is the state reference for median and high complexity traumas and burn victims; around 2000 patients are monthly treated [26] .
2. Objectives
The aims of this study were to evaluate demographic data on vascular trauma victims; to establish the mechanism, anatomic location, injury pattern and surgical techniques used to manage the vascular lesions treated at the Metropolitan Emergency Hospital (MEH); to ascertain associated non-vascular injuries and patients clinical outcome.
3. Methods
Transversal, descriptive and retrospective study. Data were collected by reviewing medical records of patients treated at the MEH from February 2011 to February 2013. The University Center of Pará ethics committee approved the research.
The authors used a research protocol with questions regarding the date of trauma, patient gender and age, mechanism and anatomic topography of injury (cervical, thoracic, abdominal, upper and lower limbs), the traumatized vessel, associated non-vascular injuries, vascular injury pattern description (total or partial transection, thrombosis, pseudoaneurysm, arterial-venous fistula), surgical management employed, post-operatory clinical evolution and need for surgical re-intervention.
Inclusion criteria: patients submitted to surgical procedures for arterial or venous injuries at the MEH from February 2011 to February 2013 by the vascular surgery team.
Exclusion and not inclusion criteria: if surgical exploration revealed no vascular injury; iatrogenic vascular injuries; traumatic limb amputation; primary limb amputation (limbs that were amputated as first choice treatment); patients proceeding from the burn treatment unit and vascular injuries treated by other surgeons that not the vascular specialist.
Patients were grouped by age, according to the following intervals: 0 to 12, 13 to 18, 19 to 24, 25 to 49, 50 to 60 and older than 60 years.
Regarding the trauma mechanism, injuries were classified as firearm’s projectile wound (FPW) (inflicted by firearms of any kind), cutting wounds (CW) (inflicted by blades, glass or other sharped surface object), traffic accidents (TA) (running overs, collisions between motor vehicles and motorcycle falls) and falls.
Arterial and venous lesions were classified as compressible vascular injuries (CVI), if hemorrhage could be interrupted by direct wound compression or by tourniquet, and as non-compressible vascular injuries (NCVI), if bleeding could not be contained by these maneuvers.
For statistical analysis purposes, only patients with operative site hematoma and/or infection that required abscess or clot surgical drainage, debridement and/or limb amputation were considered as presenting hematoma or infection as post-operative complications.
In case of patient’s death, the cause of death and if it has occurred during or after the vascular surgical procedure was ascertain. If death happened at the post-operative period, cases were grouped according to the following intervals: less than 6 hours (h), 6 to 24 h, 24 to 72 h and latter than 72 h after surgery.
For surgical re-interventions only those related to the vascular injury (it’s treatment or consequences) as, for example, amputations after revascularization failure or fasciotomies were analyzed. A second surgery indicated for treatment of non-vascular injuries as, for example, a re-laparotomy to manage an intestinal fistula in a patient treated for an inferior vena cava injury was not considered.
To establish vascular injuries mortality, patients who sustained non-vascular injuries at a different topography than the vascular injury one (for example, a patient with a superficial femoral artery and a brain injury secondary to firearm’s projectile) were excluded.
Bioestat® 5.0 and Excel®2010 software were used for statistical analysis. The non-parametric chi-square and G-test of independence tests were used; statistical significance was considered when p < 0.05.
4. Results
During the period considered for this study, the vascular surgery team operated 304 patients; 131 were excluded after exclusion criteria appliance; the remaining 173 cases were analyzed.
Male gender patients accounted for 166 cases (95.95%—p < 0.0001 chi-square test) and female for 7 cases (4.05%).
Age ranged from 8 to 70 years old, with mean age of 28.92 years; 2 patients were younger then 12 years old (1.16%); 25 were between 13 and 18 (14.45%); 43 patients were between 19 and 24 (24.86%); 95 were between 25 and 49 (54.90%—p < 0.0001 chi-square test); 6 patients were between 50 and 59 (3.47%) and 2 were older than 60 years old (1.16%) (Table 1).
Penetrating trauma mechanism were the most frequent ones: firearm’s projectile wounds (FPW) were present in 82 patients (47.40%—p < 0.0001 chi-square test) and 71 patients sustained cutting wounds (CW) (41.04%). Among blunt mechanisms there were 15 traffic accidents (8.67%) cases and 2 falls from great high cases (1.16%). Three cases accounted for other trauma mechanisms (1.73%) that were not sufficiently well described on medical chart (Figure 1).
Penetrating trauma was the most common for all topographies. There was no register of thoracic or abdominal vascular injuries by blunt mechanisms. FPWs were present in 66.67% of all abdominal vascular injuries, 61.02%
Table 1. Patients distribution according to age.
Statistical Test: Chi-square; n: Number of cases; * = p-value < 0.05; %: Percentage of cases.
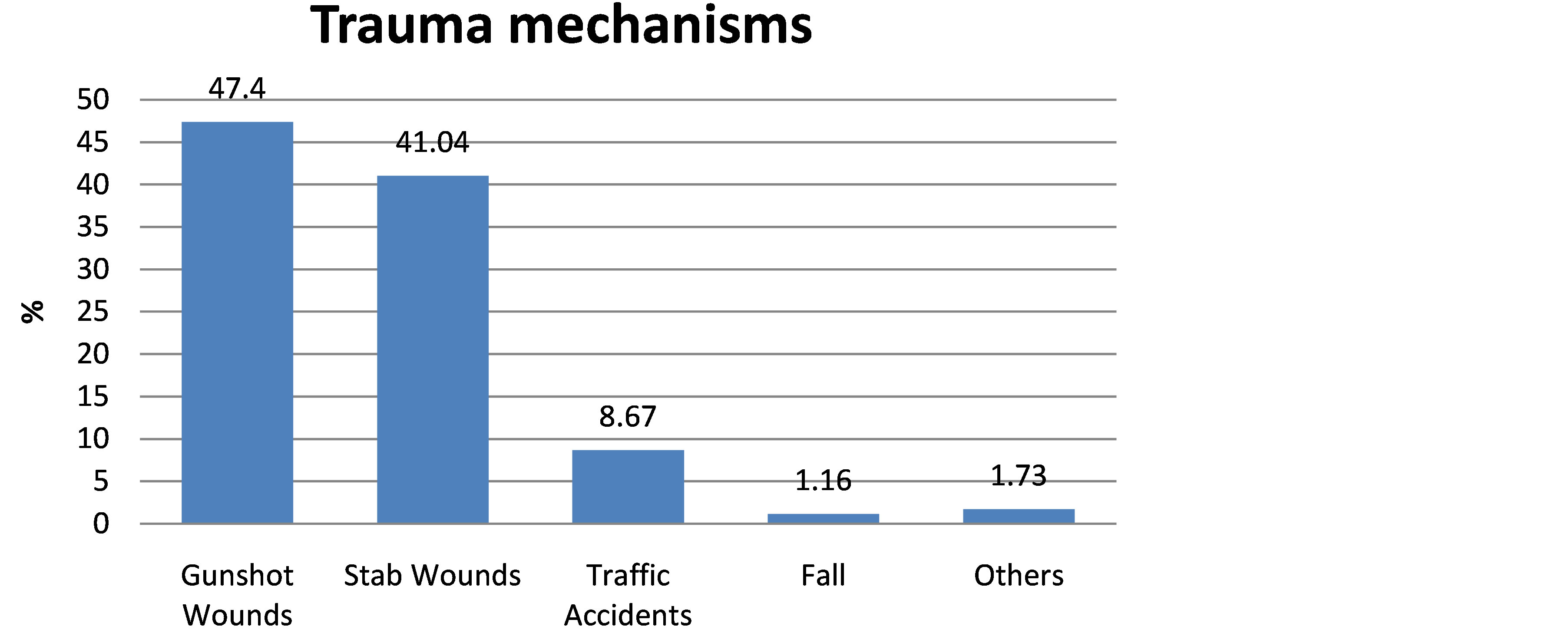
Figure 1. Trauma mechanism of patients treated for vascular injuries.
of lower limbs and 80% of thoracic vascular injuries. CWs were responsible for 70.76% of upper limbs (p < 0.0001 chi-square test) and 50% of cervical vascular traumas.
Topographic analysis revealed that 83.23% of vascular traumas were peripheral; from these, 79 patients (45.66%—p < 0.0001 chi-square test) sustained lower limbs and 65 patients (37.57%) presented upper limbs vascular injuries. There were 12 cases (6.94%) of abdominal vascular injuries, 09 cases (5.20%) of thoracic vascular lesions and 08 (4.62%) of cervical vascular injuries (Figure 2).
Six patients sustaining abdominal vascular injuries died (50%); 02 patients with lower limbs vascular trauma (2.53%); 01 patient presenting neck vascular lesion (12.5%); 02 patients with thoracic vascular injuries (22.22%) died. None of the upper limb’s vascular traumas leaded to death. As the incidence of death was this low, statistical analysis was not possible to be applied.
Amputation was necessary in 21 patients with lower limb’s vascular injuries (26.58%—p = 0.0071 chi-square test) and in 6 patients with upper limb’s vascular injuries (9.23%).
Isolated arterial injury was found in 97 patients (56.07%—p < 0.0001chi-square test), while exclusively venous trauma happened in 20 patients (11.56%). Simultaneous arterial and venous trauma was found in 56 cases (32.37%) (Figure 3).
Simultaneous non-vascular trauma was found in 75 patients (43.35%—p = 0.0944 chi-square test) (Table 2). Bone fractures were the most common association; it was present in 44 patients (25.43%) and accounted for 49.07% (p = 0.0008 chi-square test) of all associated non-vascular injuries. Peripheral nerve lesions happened in 15.6% of patients, representing 27.28% of all associated non-vascular injuries and thoracic and abdominal organs were injured in 7.51% of patients (23.15% of all associated non-vascular injuries) (Table 2).
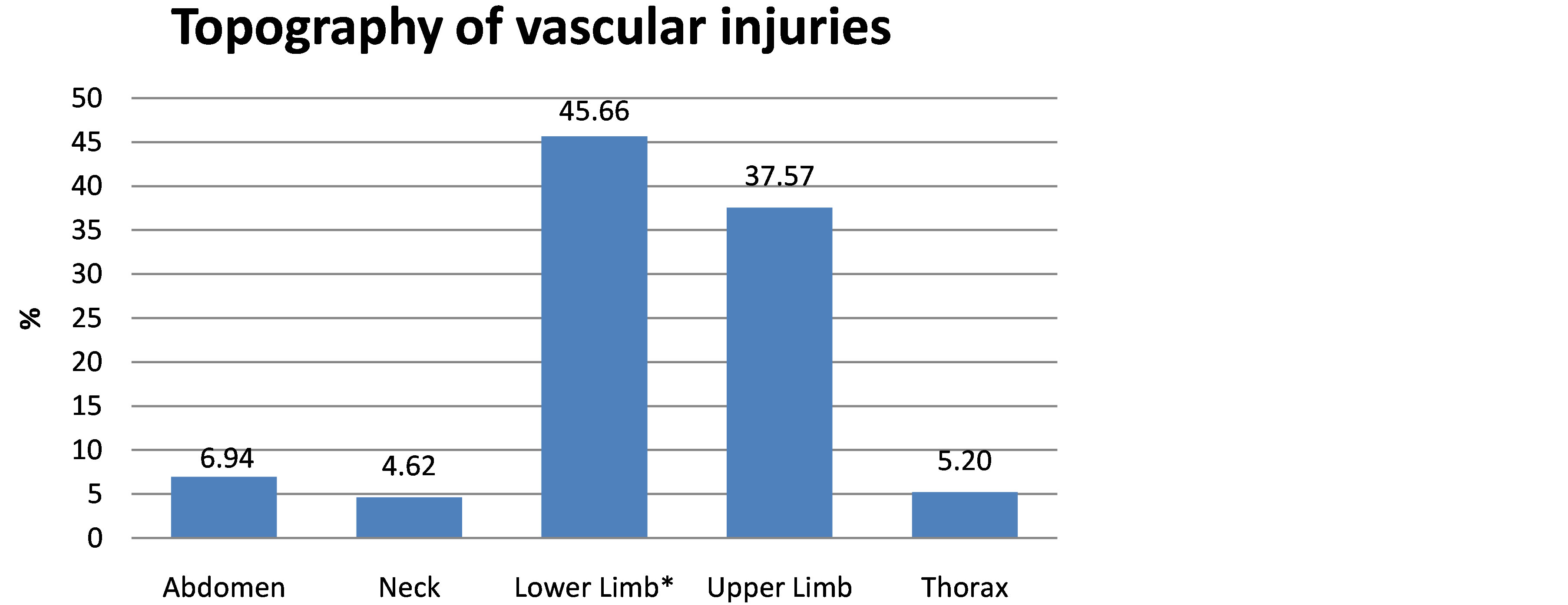
Figure 2. Topography of vascular injuries.
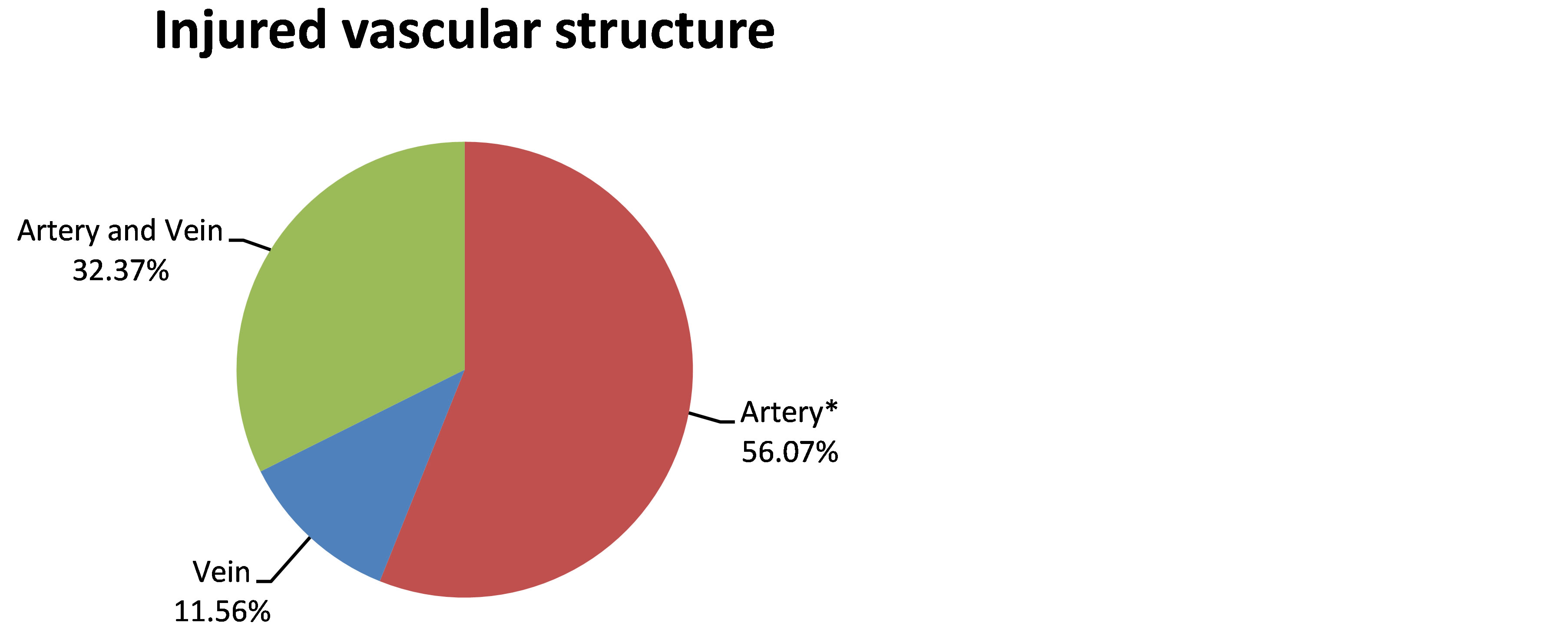
Figure 3. Injured vascular structures in patients treated for vascular traumas.
Table 2. Associated non-vascular injuries in patients treated for vascular traumas.
Statistical Test: Chi-square; n: Number of cases; * = p-value < 0.05; %: Percentage of cases; **Thoracic and abdominal structures (thoracic duct, large bowel, small bowel, bladder, liver and pancreas) were analyzed as a single group because of the low incidence of each specific injury.
Compressible vascular injuries (CVI) were more frequent, accounting for 143 (86.67%) of all arterial and 63 (70%) of all venous injuries. Among non-compressible vascular injuries (NCVI) there were 22 arterial lesions (13.33%) and 27 venous traumas (30.00%). Difference between CVI and NCVI for arterial and venous lesions was statistically significant with p < 0.0001 and p = 0.0002 respectively (chi-square test).
The most frequently injured arteries were the superficial femoral and the ulnar, each accounting for 26 cases (15.75% of all arterial lesions—p < 0.0001chi-square test).Others arterial injuries are listed below (Table 3).
Among patients submitted to lower limb’s amputation, femoral superficial artery was injured in 23.80% of cases, 14.29% had associated fractures. The popliteal artery was injured in 33.33% of cases, 9.52% had associated fractures. Below the knee arteries injuries were present in 14.29% of lower limb’s amputation cases and associated fractures were present in 9.52%.
In 28.57% of all lower limbs amputation cases, patients presented limb ischemia but the injured artery’s description was not found on medical records. There was no statistical difference between amputation rates regarding the association or not to bone fractures for none of the traumatized arteries (Table 4).
The most frequently injured veins were the superficial femoral with 16 cases (17.77%) and the popliteal with 13 (14.44%) of all venous lesions. Others venous injuries are listed below (Table 5). There was no statistical difference between the venous injuries rates (p > 0.05 chi-square test).
Among the 173 studied cases, 129 (74.57%) had a description regarding the vascular injury pattern. Among these cases 91 (52.00%—p < 0.0001 chi-square test) presented total vessel transection, 48 (27.43%) had partial vessel transection, 19 (10.86%) presented pseudoaneurysms and 17 (9.71%) had vessel thrombosis.
The most frequently used surgical technique for arterial injuries management was autologous vein graft interposition (64 cases = 36.57%—p < 0.0001chi-square test) and the great saphenous vein was the most frequently used graft for this procedure (57.14%). The superficial femoral (33.33%), brachial (23.33%) and popliteal (18.33%) arteries were the most common sites of vein graft interposition. No patient was treated with synthetic graft interposition.
Other surgical procedures for arterial injuries included 30 end-to-end anastomosis (17.14%), 13 throboembolectomies (7.42%), 07 arteriorrhaphies (4.00%) and 01 case of temporary intravascular shunt (0.57%) as damage control technique. In 02 cases arterial injury management was not completed because of patient’s death during surgery (1.14%). In 06 patients, operated for bone fractures, an arterial injury was not promptly diagnosed
Table 3. Arterial injuries anatomic locationin patients treated for vascular traumas.
Statistical Test: Chi-square; n: Number of cases; * = p-value < 0.05; %: Percentage of cases; ONCA: Other non-compressible arteries. Each one presented less than 05 cases (common carotid, external carotid, hypogastric, external iliac and renal). OCA: Other compressible arteries. Each one presented less than 05 cases (tibiofibular trunk, fibular and common femoral). **Percentage of total affected arteries. ***p-value obtained by comparison of arteries with at least 05 cases.
Table 4. Lower limbs amputation rate according to injured arteries and its association to simultaneous bone fractures.
Statistical Test: Independence G Test; n: Number of cases; %: Percentage of cases; **Patients operated by the orthopedics team, presented limb ischemia and were amputated without the identification of the vascular injury. Therefore, they were excluded from the statistical analysis.
Table 5. Anatomic location of venous injury in patients treated for vascular trauma.
Statistical Test: Chi-square; n: Number of cases; * = p-value < 0.05; %: Percentage of cases; Adapted from Markov et al. (2012). ONCV: Other Non-Compressible Veins. Each one presents less than 05 cases (external iliac, external jugular, internal jugular, common iliac, internal iliac, subclavian and hypogastric). OCV: Other Compressible Veins. Each one presents less than 05 cases (fibular, anterior tibial, ulnar, basilica, cephalic, deep femoral and radial). **Percentage of total affected veins. ***p-value obtained by comparison of veins with at least 05 cases.
(3.42%); these patients developed limb ischemia and were submitted to amputation (Table 6).
Arterial ligature was performed in 51 cases (29.14%); most of than were upper limb’s traumas with radial or ulnar injuries (22 cases) and lower limb’s traumas with injured below the knee arteries (21 cases).
For venous injuries treatment, ligature was the most frequent surgical technique (68 cases = 85.00%—p < 0.0001chi-square test). Venorrhaphy was performed in 11 cases (13.75%). In 01 case venous injury management was not completed because of patient’s death during surgery (1.25%) (Table 7).
Forty-four patients needed surgical re-interventions (25.43%), most of them because of ischemia, infectious complications and compartmental syndrome. The majority of patients were re-operated for limb amputation (39.13%—p < 0.0001 chi-square test); debridement was performed in 31.88%, skin grafts in 11.59% and fasciotomies in 7.25% of re-operations.
The majority of patients (109 cases = 63%) developed no postoperative complications and the remaining 64 (37%) presented at least one postoperative complication. Infection was the most common complication (40.74% —p < 0.0001 chi-square test). Postoperative limb ischemia was present in 22.22% and neurological deficit in 16.04% of patients (Table 8).
Among all analyzed patients, 27 (15.60%) were submitted to amputations. Lower limbs were more frequently amputated (21 = 77.77%—p = 0.0071 chi-square test) than upper limbs (06 = 22.23%). Fractures were present in 17 amputated limbs (62.96%): 13 were lower limbs (61.90%) and 04 were upper limbs (66.67%); although most of the amputated limbs had associated fractures, this difference was not statistically significant (p = 0.7911 G-test of independence) (Figure 4).
Eleven patients died; hence, the overall mortality was 6.36%. Cause of death was hypovolemic shock in 09 cases (81.82%—p < 0.0348 chi-square test) and sepsis in 02 patients (18.18%). Three patients died during surgery (27.27%), 03 during the first 24 hours after surgery (27.27%), 02 between 2 and 7 days after surgery (18.18%), 01 between 10 and 15 days after surgery (9.09%) and 01 patient died more than 25 days after surgery (9.09%) (Table 9). It was not possible to apply statistical tests to these data because of the low incidence of death in this series.
Among patients that died, 02 had isolated arterial injuries (18.18%), 05 had isolated venous traumas (45.45%) and 04 presented combined arterial and venous injuries (36.36%). It was not possible to apply statistical tests to these data because of the low incidence of death in this series (Table 10).
5. Discussion
As the incidence of trauma is rising all over the world, it is crucial that surgeons be prepared to deal with vascular injuries [2] . These injuries are associated to high mortality and morbidity in civilian populations of urban areas and militaries on the battlefield [6] [27] -[30] .
Vascular injuries are more frequent among young and economically productive patients and represent asurgical challenge because of aggressive trauma mechanisms and increasing severity of associated lesions [31] [32] , especially when combined to hemorrhagic shock, which, according to experimental researches, diminishes the probability of limb functional recovery if blood flow restoration is delayed for more than 3 hours [33] . Rigid
Table 6. Arterial injuries treatment in patients treated for vascular trauma.
Statistical Test: Chi-square; n: Number of cases; * = p-value < 0.05; %: Percentage of cases; **Intraoperative death without arterial treatment. ***175 arterial injuries detected in 173 patients. ANIVI: Amputation for Not Identified Vascular Injuries.
Table 7. Venous injuries treatment in patients treated for vascular trauma.
Statistical Test: Chi-square; n: Number of cases; * = p-value < 0.05; %: Percentage of cases; **Intraoperative death without venous treatment. ***80 venous injuries detected in 173 patients.
Table 8. Postoperative complications in patients treated for vascular trauma.
Statistical Test: Chi-square; n: Number of cases; * = p-value < 0.05; %: Percentage of cases; **Common iliac artery and inferior vena cava injuries during lysis of Intestinal adhesions in one patient.
Table 9. Death etiology and period of death in patients treated for vascular trauma.
Statistical Test: Chi-squared; n: Number of cases; * = p-value < 0.05; %: Percentage of cases; PO: Postoperative; **Low death rate prevented statistical test application.
criteria must be followed in order to obtain early diagnosis of vascular injury and prevent function limitation, amputation and death [34] .
In consonance with other papers, male gender accounted for the majority (95.95%) of this casuistry. This is probably justified by the fact that men are more exposed to violence and traffic accidents risky situations [6] [14] [16] [31] [35] -[39] . The mean age of 28.92 years old, found on this study, matches the literature [6] [17] [21] [22] [31] [34] [39] [40] . Most patients sustained penetrating traumas (88.44%), mainly firearm’s projectile wounds (FPW) (47.40%), a data supported by many other studies [22] [31] [34] [35] [41] . Nevertheless, other
Table 10. Injured blood vessels in patients treated for lethal vascular trauma.
n: Number of cases; %: Percentage of cases; *Low death rate prevented statistical test application.
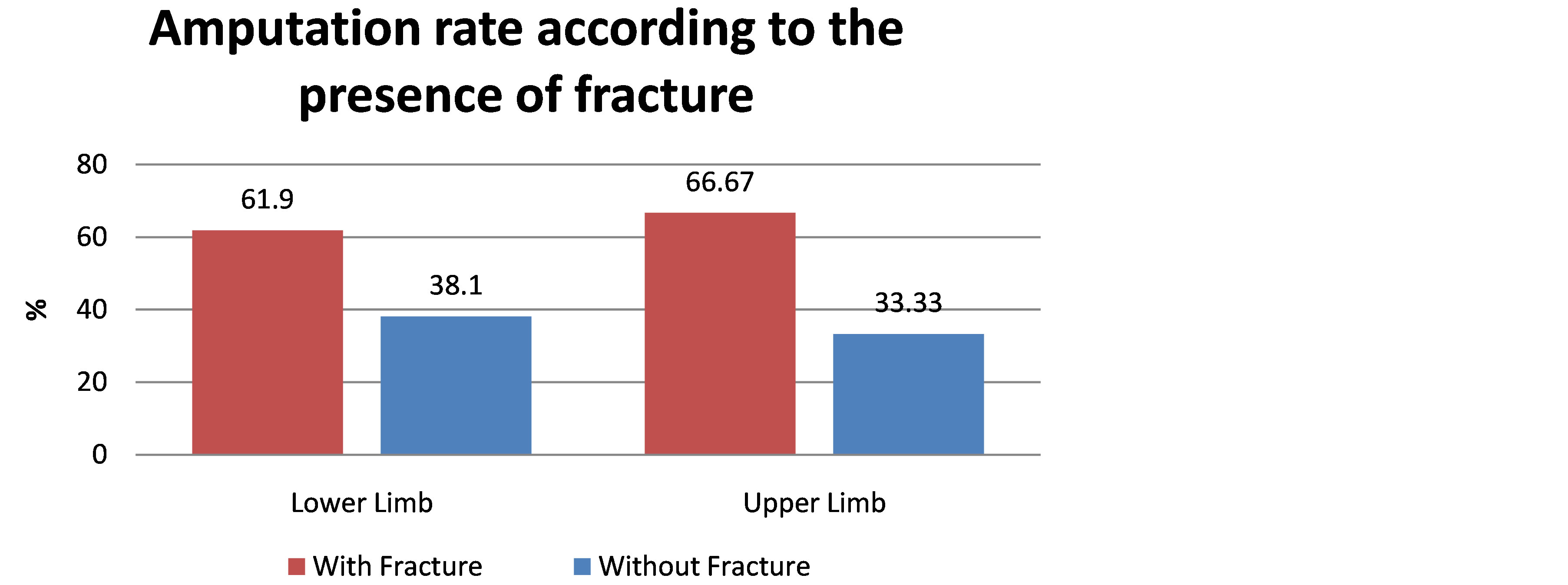
Figure 4. Lower limb and upper limb amputations rate according to the presence of associated fracture.
authors found an equal incidence of FPW and blunt trauma [9] ; cutting wounds (CW) were the most frequent trauma mechanism detected by others [14] .
As previously found by other authors [6] [16] [42] , extremities sustained most of vascular traumas (83.24%), especially lower limbs (45.66%).
The most frequently associated non-vascular injuries were bone fractures, which were found in 25.43% of patients, similar to results exposed by Murad and cols, who found a 27.08% rate association of vascular trauma and fractures [34] . This rate was much lower than that reported by Nitecki and cols, who detected a 80.00% rate among military casualties in Israel [21] , but this difference is probably due to the fact that combat injuries are frequently caused by high speed firearm’s projectiles and explosives, which increases the probability of nonvascular associated injuries.
Pseudoaneurysms, a vascular trauma late complication due to both blunt and penetrating mechanisms [43] [44] was found in 10.86% of patients, a similar incidence than those found by Murad and cols (10.41%) in an Egyptian series [34] and by Yavuz and cols (8.30%) who analyzed a 10 year Turkish casuistry of femoral artery injuries [45] . All pseudoaneurysms detected in the present study were the consequence of a miss diagnosed arterial injury during patient’s initial evaluation; a fact that is widely described on literature [21] [22] [46] [47] .
The isolated arterial injuries predominance over isolated venous ones, here presented, was similar to other reports [8] [31] [34] .
Although this study have analyzed only civilian patients, the incidences of CVI for both arterial (86.67%) and venous (70.00%) were similar to the ones reported by Markov, when describing data from middle east military conflicts [48] .
As previously reported by many authors, peripheral arteries were the most injured ones. The superficial femoral artery was the most commonly traumatized (15.75%), in agreement with most authors [6] [9] [21] [24] [31] [34] [35] [49] [50] . However, diverging from previous papers, the frequency of ulnar artery injury was as high as the superficial femoral artery (15.75%); this is related to the high incidence of cutting wounds (41.04%) in this casuistry, a mechanism frequently associated to upper limb’s trauma [14] [50] [51] and is probably justified by the high incidence of aggression with machete in the Amazon region and the fact that victims usually use the ulnar forearm border to defend themselves.
Venous injuries were also more frequent on lower limbs, as reported by many authors [9] [16] [20] [49] [52] . In this study the superficial femoral vein was the most injured (17.77%) and the popliteal vein, the second most injured (14.44%), similarly to many reports [16] [20] [49] ; nevertheless, other researchers pointed the popliteal vein as the most injured one [9] [52] .
Popliteal arteries traumas are described as the most related to limbs amputations due to vascular injuries [9] [21] [53] . In this study, among lower limb’s arterial injuries, it presented the higher rate of limb amputation (33.33%), which is corroborated by others [54] .
Most of arterial injuries were managed by autologous vein graft interposition, mainly using the great saphenous vein; most studies have also found this the most adopted surgical technique for arterial lesions [16] [21] [31] [35] . On the other hand, according to fewer authors, most arterial injuries were treated by end-to-end anastomosis [23] [34] .
Autologous vein graft interposition is considered the most durable and effective technique for vascular repair, especially when the injury produced arterial tissue loss, diminishing the probability of a tension free end-to-end anastomosis. Synthetic grafts are not frequently used for traumatic injuries due to higher thrombosis and infection rates, which leads to limb’s amputation [20] . Synthetic grafts were not used in this casuistry.
For the 90 detected venous injuries, ligature was the most performed technique (85%); other studies also support that ligature is the most frequent surgical technique for venous trauma [16] [49] . Jawas and cols published that 13 from a total of 17 venous injuries were treated by venorrhaphy and only 4 were ligated [9] , but the author himself considered as a specific characteristic of his surgical team the avoidance of venous ligature. The best surgical strategy for venous injuries management remains uncertain, but for hemodynamically unstable patients, ligature is still considered the best choice [52] .
Operative site infection is the most frequent post-operative complication [55] . In this study, operative site infection (19.07%) and arterial thrombosis (10.40%) were the most common complications.
Most of the times reoperations are necessary due to infectious and ischemic complications [21] . In this casuistry reoperations were necessary in 25.43% of patients, mainly for amputations (39.13%) and debridements (31.88%), which is in agreement with other reports [20] [23] .
From the total amount of patients, 27 (15.60%) were submitted to limb’s amputation. Literature reports amputation rates as low as 9.56% [35] and as high as 25% [9] .
The overall mortality was 6.36%, which is similar to many reports on the literature [16] [31] [35] [48] . Aspreviously described [16] [31] [53] , the hypovolemic and septic shocks were the most common causes of death. Agreeing with previous data [16] , isolated arterial injuries or it’s association to venous injuries were found in nearly half of lethal cases; and among these patients NCVI were the most frequent ones, also in consonance with higher mortality rates previously reported [48] .
Isolated non-compressible venous injuries happened in 45.45% of deaths, mainly the inferior vena cava trauma, which accounted for 60% of these cases. The lethality of this specific injury corroborates previously published data [48] [56] .
This study presents some limitations as the fact that the casuistry had a bias selection, as patients constituted a convenience sample, hence the MEH is the only regional specialized center for vascular trauma cases and patients sometimes arrive with a delay that can lead to unfavorable clinical outcomes. Others limitations include the fact that the 2 year period that was studied didn’t allow a more significant amount of cases (before 2011 medical charts were not electronically archive at the hospital in case) and the issue that patients were not followed after hospital discharge, which would allow late post-operative evaluation.
Nevertheless, databases research (Pubmed, Scielo, Bireme and Lilacs) didn’t provide studies which have analyzed in similar way the demographic and anatomical data, the surgical management and clinical outcome of vascular trauma victims in the Amazon region.
6. Conclusions
1) Vascular injuries occurred predominantly in men from 24 to 49 years old.
2) The majority of vascular injuries were caused by penetrating mechanisms, mainly by firearms projectiles.
3) Lower limb was the most affected topography.
4) The most frequently injured vessels were the ulnar and superficial femoral arteries and the superficial femoral vein.
5) Compressible vascular injuries were more frequent and the complete vessel transection was the most common injury pattern.
6) Arterial trauma was most frequently treated with autologous venous graft interposition.
7) Venous injuries were most frequently managed by ligature.
8) Fractures were the most common associated non-vascular lesions.
9) The majority of patients recovered uneventfully and ischemic and infectious complications were the most frequent ones.
10) Reoperation was performed in approximately 25.00% of vascular trauma cases.
11) Limb’s amputation was performed in approximately 16.00% of vascular trauma cases, most of the times it was related to lower limb’s vascular injuries.
12) The overall mortality for vascular trauma was 6.36% and deaths were caused by hypovolemic and septic shocks.
References
- World Health Organization (WHO) (2010) Injuries and Violence: The Facts. World Health Organization, Geneva.
- Fatimi, S.H., et al. (2012) Major Thoracic Vessels and Cardiac Trauma: Case Series from a Centre in a Developing Country. Ulus Travma Acil Cerrahi Derg, 18, 490-494. http://dx.doi.org/10.5505/tjtes.2012.39225
- Brasil. Secretaria de Políticas de Saúde—Ministério da Saúde (2000) PolíticaNacional de Redução da MorbimortalidadeporAcidentes e Violência. Revista de Saúde Pública, 34, 427-430. http://dx.doi.org/10.1590/S0034-89102000000400020
- Brasil. Ministério da Saúde. Departamento de Informáticado SUS (2013) Morbidade Hospitalar do SUS por Causas Externas—Por Local de Internação—Brasil. Datasus. Disponívelem. http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sih/cnv/fiuf.def
- Moreira, R.C.R. (2008) Trauma Vascular. Jornal Vascular Brasileiro, 7, 185-186. http://dx.doi.org/10.1590/S1677-54492008000200018
- Bilgen, S., et al. (2009) Peripheral Vascular Injury-Related Deaths. Ulusal Travma ve Acil Cerrahi Dergisi, 15, 357- 361.
- Salas, C.D. (2011) Trauma Vascular, Visión del Cirujano Vascular. Revista médica Clínica Las Condes, 22, 686-696.
- Silva, M.A.M., et al. (2012) Trauma Vascular Napopulaçãopediátrica. Jornal Vascular Brasileiro, 11, 199-205. http://dx.doi.org/10.1590/S1677-54492012000300006
- Jawas, A., et al. (2013) Management of War-Related Vascular Injuries: Experience from the Second Gulf War. World Journal of Emergency Surgery, 8, 22. http://dx.doi.org/10.1186/1749-7922-8-22
- Westphal, F.L., De Lima, L.C., Netto, J.C.L., Da Silva, De Souza da Silva, J., Dos Santos Jr., V.L. and Westphal, D.C. (2009) Thoracic Trauma: Analysis of 124 Patients Who Underwent Thoracotomy. Revista do Colégio Brasileiro de Cirurgiões, 36, 482-486. http://dx.doi.org/10.1590/S0100-69912009000600004
- Casey, E., et al. (2009) Vascular Injuries in the Lower Limb of Athletes. Nerve and Vascular Injuries in Sports Medicine, 183-198.
- Fernandes, R.F., et al. (2011) Tratamento Endovascular de Lesõesarteriaistraumáticas. Angiologia e Cirurgia Vascular, 7, 21-28.
- Antunes, L.F., et al. (2011) Traumatismosvascularesrevisão de 5 Anos. Angiologia e Cirurgia Vascular, 7, 86-93.
- Jaha, L., et al. (2012) A Decade of Civilian Vascular Trauma in Kosovo. World Journal of Emergency Surgery, 7, 24. http://dx.doi.org/10.1186/1749-7922-7-24
- Staeheli, G.R., Fraser Jr., M.R. and Morgan, S.J. (2012) The Dangers of Damage Control Orthopedics: A Case Report of Vascular Injury after Femoral Fracture External Fixation. Patient Safety in Surgery, 6, 7. http://dx.doi.org/10.1186/1754-9493-6-7
- Costa-Val, R., et al. (2008) Reflexões sobre o trauma cardiovascular civil a partir de um estudo prospectivo de 1000 casos atendidos em um centro de trauma de nível I. Revista do Colégio Brasileiro de Cirurgiões, 35, 162-167.
- Rasouli, M.R., Moini, M. and Khaji, A. (2009) Civilian Traumatic Vascular Injuries of the Upper Extremity: Report of the Iranian National Trauma Project. Annals of Thoraacic and Cardiovascular Surgery, 15, 389-393.
- Jong-Woo, K.I.M., et al. (2010) Vascular Injury Associated with Blunt Trauma without Dislocation of the Knee. Yonsei Medical Journal, 51, 790-792. http://dx.doi.org/10.3349/ymj.2010.51.5.790
- Medeiros, C.A.F., et al. (2008) Tratamento Endovascular do Trauma Arterial dos Membros. Jornal Vascular Brasileiro, 7, 56-61. http://dx.doi.org/10.1590/S1677-54492008000100010
- Fox, C.J., et al. (2005) Contemporary Management of Wartime Vascular Trauma. Journal of Vascular Surgery, 41, 638-644. http://dx.doi.org/10.1016/j.jvs.2005.01.010
- Nitecki, S.S., et al. (2013) Management of Combat Vascular Injuries Using Modern Imaging: Are We Getting Better? Emergency Medicine International, 2013, Article ID: 689473.
- Van Waes, O.J.F., et al. (2013) Treatment of Penetrating Trauma of the Extremities: Ten Years Experience at a Dutch Level 1 Trauma Center. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 21, 2. http://dx.doi.org/10.1186/1757-7241-21-2
- Kshirsagar, A.Y., et al. (2013) Management of Vascular Injury in Rural Setup. International Journal of Health Sciences & Research, 3, 12-16.
- Ganie, F.A., et al. (2012) The Increasing Rate of Secondary Amputation in Popliteal Arterial Injury Associated with Multi-Organ Injuries and Hypotension. International Cardiovascular Research Journal, 6, 124-127.
- Brasil, InstitutoBrasileiro de Geografia e Estatística (IBGE) (2010) Censo Demográfico. http://www.ibge.gov.br/
- Brasil, Governo do Estado do Pará, Secretaria de Estado de Saúde, Hospital Metropolitano de Urgência e Emergência, Departamento de Ensino e Pesquisa, 2013. http://www.saude.pa.gov.br/
- Caixeta, C.R., et al. (2010) Morbidadeporacidentes de Transporte Entre Jovens de Goiânia, Goiás. Ciência & Saúde Coletiva, 15, 2075-2084. http://dx.doi.org/10.1590/S1413-81232010000400021
- EUA, Centers for Disease Control and Prevention (2011) Violence-Related Firearm Deaths among Residents of Metropolitan Areas and Cities—United States, 2006-2007. Morbidity and Mortality Weekly Report, 60, 573-578.
- Miller, T.E. (2013) New Evidence in Trauma Resuscitation—Is 1:1:1 the Answer? Perioperative Medicine, 2, 13. http://dx.doi.org/10.1186/2047-0525-2-13
- Gonsaga, R.A.T., et al. (2013) Characteristics of Care Provided by the Emergency Mobile Care Service in the Municipality of Catanduva, São Paulo state, Brazil, 2006-2012. Epidemiologia e Serviços de Saúde, 22, 317-324.
- González, A.H.R., Molina, J.L.C. and Martínez, M.R.L. (2013) Trauma Vascular. Experiencia de 30 años en el Estado de Michoacán. Revista Mexicana de Angiología, 41, 55-61.
- Palu, L.A. (2013) O Custo Social dos Acidentescommotocicletas e Suacorrelação com Osíndices de Trauma. 92f. Dissertação (MestradoemClínicaCirúrgica), Faculdade de Medicina, Universidade Federal do Paraná, Curitiba.
- Hancock, H.M., et al. (2011) Hemorrhagic Shock Worsens Neuromuscular Recovery in a Porcine Model of Hind Limb Vascular Injury and Ischemia-Reperfusion. Journal of Vascular Surgery, 53, 1052-1062. http://dx.doi.org/10.1016/j.jvs.2010.10.104
- Murad, M.K., et al. (2012) Prehospital Trauma Care Reduces Mortality. Ten-Year Results from a Time-Cohort and Trauma Audit Study in Iraq. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 20, 13.
- Topal, A.E., Eren, M.N. and Celik, Y. (2010) Lower Extremity Arterial Injuries over a Six-Year Period: Outcomes, Risk Factors, and Management. Vascular Health and Risk Management, 6, 1103-1110. http://dx.doi.org/10.2147/VHRM.S15316
- Ranney, M.L., Whiteside, L., Walton, M.A., Chermack, S.T., Zimmerman, M.A. and Cunningham, R.M. (2011) Gender Differences in Characteristics of Adolescents Presenting to the Emergency Department with Acute Assault-Related Injury. Academic Emergency Medicine, 18, 1027-1035. http://dx.doi.org/10.1111/j.1553-2712.2011.01165.x
- Malta, D.C., Mascarenhas, M.D.M., Bernal, R.T.I., De Araújo Andrade, S.S.C., Das Neves, A.C.M., De Melo, E.M. and Da Silva Jr., J.B. (2012) Causas Externas em Adolescentes: Atendimentos em Services Sentinelas de Urgência e Emergência nas Capitais Brasileiras-2009. Ciência & Saúde Coletiva, 17, 2291-2304. http://dx.doi.org/10.1590/S1413-81232012000900011
- Ascari, R.A., Chapieski, C.M., Da Silva, O.M. and Frigo, J. (2013) Perfil Epidemiológico de Vítimas de Acidente de Trânsito. Revista Enfermagem Da UFSM, 3, 112-121. http://dx.doi.org/10.5902/217976927711
- Zabeu, J.L.A., Zovico, J.R.R., Júnior, W.N.P. and Neto, P.F.T. (2013) Perfil de Vítima de Acidente Motociclístico na Emergência de um Hospital Universitário. Revista Brasileira de Ortopedia, 48, 242-245. http://dx.doi.org/10.1016/j.rbo.2012.09.006
- Copuroglu, C., Heybeli, N., Ozcan, M., Yilmaz, B., Ciftdemir, M. and Copuroglu, E. (2012) Major Extremity Injuries Associated with Farmyard Accidents. The Scientific World Journal, 2012, Article ID: 314038.
- Nafissi, N., Saghafinia, M. and Balochi, K. (2008) Improving Trauma Care in Rural Iran by Training Existing Treatment Chains. Rural and Remote Health, 8, 881.
- Mishwani, A.H., Ghaffar, A. and Janjua, S. (2012) Combat Related Vascular Trauma. Journal of the College of Physicians and Surgeons-Pakistan, 22, 213-217.
- Aslanturk, O., Ertem, K., Karakaplan, M. and Korkmaz, M.F. (2013) Pseudoaneurysm Discovered during Reverse Radial Forearm Flap after a Gunshot Injury: A Case Report. Medicine Science, 2, 414-422.
- Kaczynski, J., Wilczynska, M. and Fligelstone, L. (2013) Flail Upper Limb Due to Delayed Presentation of a Traumatic Brachial Artery Pseudoaneurysm. BMJ Case Reports, 1-3. http://dx.doi.org/10.1136/bcr-2012-007706
- Yavuz, C., Demirtas, S., Caliskan, A., Ertas, F., Kaya, H., Aydin, M., Benli, E.D., Celik, Y. and Eren, M.N. (2013) The Predictors of Poor Outcomes in Patients with Femoral Artery Injuries. European Review for Medical and Pharmacological Sciences, 17, 1901-1908.
- Küçükarslan, N., Oz, B.S., Ozal, E., Yildirim, V. and Tatar, H. (2007) Factors Affecting the Morbidity and Mortality of Surgical Management of Vascular Gunshot Injuries: Missed Arterial Injury and Disregarded Vein Repair. Ulusal Travma ve Acil Cerrahi Dergis, 13, 43-48.
- Dobson, P.F., Purushothaman, B., Michla, Y., England, S., Krishnan, M.K. and Tourret, L. (2013) Delayed Ulnar Nerve Palsy Secondary to Ulnar Artery Pseudoaneurysm Distal to Guyon’s Canal Following Penetrating Trauma to the Hand. Annals of the Royal College of Surgeons of England, 95, 75-76. http://dx.doi.org/10.1308/003588413X13511609955850
- Markov, N.P., DuBose, J.J., Scott, D., Propper, B.W., Clouse, W.D., Thompson, B., Blackbourne, L.H. and Rasmussen, T.E. (2012) Anatomic Distribution and Mortality of Arterial Injury in the Wars in Afghanistan and Iraq with Comparison to a Civilian Benchmark. Journal of Vascular Surgery, 56, 728-736. http://dx.doi.org/10.1016/j.jvs.2012.02.048
- Sohn, V.Y., Arthurs, Z.M., Herbert, G.S., Beekley, A.C. and Sebesta, J.A. (2008) Demographics, Treatment, and Early Outcomes in Penetrating Vascular Combat Trauma. JAMA Surgery, 143, 783-787. http://dx.doi.org/10.1001/archsurg.143.8.783
- Santana, J.C.B., Dutra, B.S., Viana, J.A., Vieira, L.S. and Cardoso, C.M.L. (2012) Vítimas de Agressões Por Arma Branca: O Que Retrata a Demanda de um Serviço de Urgência. Cogitare Enferm, 17, 78-84.
- Zandomenighi, R.C., Mouro, D.L. and Martins, E.A.P. (2011) Ferimento Por Arma Branca: Perfil Epidemiológico Dos Atendimentos em um Pronto Socorro. Revista da Rede de Enfermagem do Nordeste, 12, 669-677.
- Nitecki, S.S., Karram, T., Hoffman, A. and Bass, A. (2007) Venous Trauma in the Lebanon War 2006. Interactive CardioVascular and Thoracic Surgery, 6, 647-650. http://dx.doi.org/10.1510/icvts.2007.158014
- Pourzand, A., Fakhri, B.A., Azhough, R., Ali Hassanzadeh, M., Hashemzadeh, S. and Bayat, A.M. (2010) Management of High-Risk Popliteal Vascular Blunt Trauma: Clinical Experience with 62 Cases. Vascular Health and Risk Management, 6, 613-618.
- Kauvar, D.S., Sarfati, M.R. and Kraiss, L.W. (2011) National Trauma Databank Analysis of Mortality and Limb Loss in Isolated Lower Extremity Vascular Trauma. Journal of Vascular Surgery, 53, 1598-1603. http://dx.doi.org/10.1016/j.jvs.2011.01.056
- Brown, K.V., Ramasamy, A., Tai, N., MacLeod, J., Midwinter, M. and Clasper, J.C. (2009) Complications of Extremity Vascular Injuries in Conflict. Journal of Trauma, 66, S145-S149. http://dx.doi.org/10.1097/TA.0b013e31819cdd82
NOTES

*Institutions: University Center of Pará (CESUPA) and Metropolitan Emergency Hospital.
#Corresponding author.


