Open Journal of Urology
Vol.2 No.4(2012), Article ID:24499,6 pages DOI:10.4236/oju.2012.24043
Predictors of Outcome after Transvaginal Mesh for Pelvic Organ Prolapse
Brady Urological Institute, Johns Hopkins Medical Institution, Baltimore, USA
Email: *imegwal1@jhmi.edu
Received August 1, 2012; revised August 31, 2012; accepted September 12, 2012
Keywords: Prolapse; Mesh; Vagina; Outcome; Complication
ABSTRACT
Introduction: We aim to report outcomes and predictors of outcome of transvaginal mesh (TVM) for pelvic organ prolapse (POP). We also report frequency, severity, risk factors, and management of mesh-related complications after TVM. Materials and Methods: We performed retrospective chart review of TVM performed from 2005 to 2010. There were 67 patients followed for a mean duration of eighteen months. Complications were reported using the International Continence Society and International Urogynecological Association classification system for prosthesis/graft complication. Results: Success rate was 88% (97% for anterior repair, 100% for posterior repair and 71% for combined repair) and complications occurred in 13 patients (19%), including vaginal hematoma, pelvic pain, urinary retention, dyspareunia and vaginal mesh exposure (in 9 patients). On multivariable logistic regression, recurrence was significantly higher with combined repair (p = 0.021), overall complication was significantly associated with younger age (p = 0.019), and mesh exposure was significantly associated with age and combined repair. All mesh-related complications were vaginal exposures occurring at median of 6 months postoperatively. Two patients were managed conservatively with vaginal estrogen cream, while seven patients elected surgical excision of exposed mesh with primary re-approximation of the vaginal epithelium. There were no excision-related complications, and in no case was the defect large enough to require closure with graft or secondary material. Conclusion: Combined anterior and posterior repair using TVM is associated with failure, younger age is associated with higher rate of complication, and combined repair and younger age are associated with mesh-related complication specifically.
1. Introduction
Pelvic organ prolapse (POP) is a common condition affecting the aging female population. The lifetime risk of undergoing a single operation for prolapse or incontinence is 11.1, with 29.2% requiring reoperation [1]. The effectiveness and durability of traditional vaginal repair techniques are highly variable. Use of biomaterials in pelvic reconstructive surgery has increased markedly in recent years. Use of absorbable grafts have shown limited effectiveness, with some authors reporting that addition of absorbable mesh did not improve cure rate of anterior colporrhaphy [2].
The transvaginal mesh repair (TVM) was introduced as an approach that could provide greater durability than traditional vaginal repairs with less morbidity than abdominal approaches. Indeed, one large study found no difference in apical success rate after transvaginal mesh repair, uterosacral ligament suspension and abdominal sacral colpopexy, but transvaginal mesh repair compared to abdominal sacral colpopexy and uterosacral ligament suspension was associated with less frequent pelvic organ injury, operating room time, estimated blood loss, and intraoperative hemorrhage greater than 500 mL [3] . Awareness of mesh-related complications has recently increased, causing some regulatory agencies to issue advisory statements regarding use of TVM [4]. There have been several studies reporting short and medium term outcomes after TVM [3,5,6] . However, there is limited data on the predictors of outcome after TVM.
The purpose of this study is not only to report our experience with TVM, including complications and efficacy, but also to determine the predictors of anatomic success and complications. We also report specifically the rate and nature of mesh-related complications in our series.
2. Materials and Methods
After obtaining institutional review board approval, we retrospectively reviewed the medical records of all patients who underwent TVM using Prolift® (Gynecare Prolift, Ethicon, Inc., Piscataway, NJ, USA) device by a single surgeon between May 2005 and July 2010. After excluding participants with missing follow-up data (n = 16), the final study population consisted of 67 consecutive patients.
Before surgery, all patients underwent physical examination in lithotomy and standing positions. Pelvic organ prolapse quantification system (POP-Q) was used for prolapse staging, and the methods and definitions conformed to the standards recommended by the International Continence Society [7]. Complications were reported using the International Continence Society (ICS) and International Urogynecological Association (IUGA) classification system for prosthesis/graft complication [8].
The Prolift® technique for vaginal mesh repair was performed according to the instructions of the manufacturer on the product insert [9]. Patients who demonstrated stress incontinence on preoperative urodynamic evaluation underwent simultaneous midurethral sling placement. Cystoscopy and digital rectal exam were performed intraoperatively at the conclusion of mesh repair to evaluate for pelvic organ injury. A urethral catheter and vaginal packing were typically left in place overnight and removed on the first postoperative day prior to discharge from the hospital. Postoperative vaginal speculum exam and interview were conducted by the primary surgeon at six weeks and then every six months.
Recurrence was defined as postoperative POP-Q stage II or greater in an operated compartment. New onset prolapse in a non-operated compartment during follow-up was also reported. For univariate analysis, rank sum test was used for continuous variables (age) and chi-square test was used for categorical variables (preoperative stage, type of surgical repair, sexual activity, year of surgery). Logistic regression was used for multivariable analysis to examine factors associated with recurrence, overall complication, and mesh-related complication. All analyses were performed using Stata 11.0 software. The vaginal mesh manufacturing company had no influence on the study design, execution, analysis or interpretation of data.
3. Results
The study population consisted of 67 patients with mean age 64 years (range, 40 - 89). Overall, 28 (42%) were stage II, 32 (48%) were stage III, five (7%) were stage IV and two (3%) did not have a preoperative POP-Q assignment (Table 1). Anterior repair was performed in 35 (52%) patients, posterior repair in seven (11%) patients and combined anterior and posterior repair in 25 (37%) patients. Twenty-four women (36%) underwent concurrent midurethral sling placement.
Mean follow up was 18.0 months (range 1 - 71). There were eight (12%) recurrences.
The anatomic cure rate was 97% (34/35 patients) after anterior repair, 100% (7/7 patients) after posterior repair, and 71% (18/25 patients) after combined repair. There were four apical descents, two anterior descents and one enterocele recurrence after combined repair. One patient had anterior and apical descent after anterior repair. Six patients (9%) developed prolapse of an unsupported compartment; two patients developed new onset apical prolapse after anterior repair, three patients developed new onset posterior prolapse after anterior repair, and one patient developed new onset anterior prolapse after posterior repair.
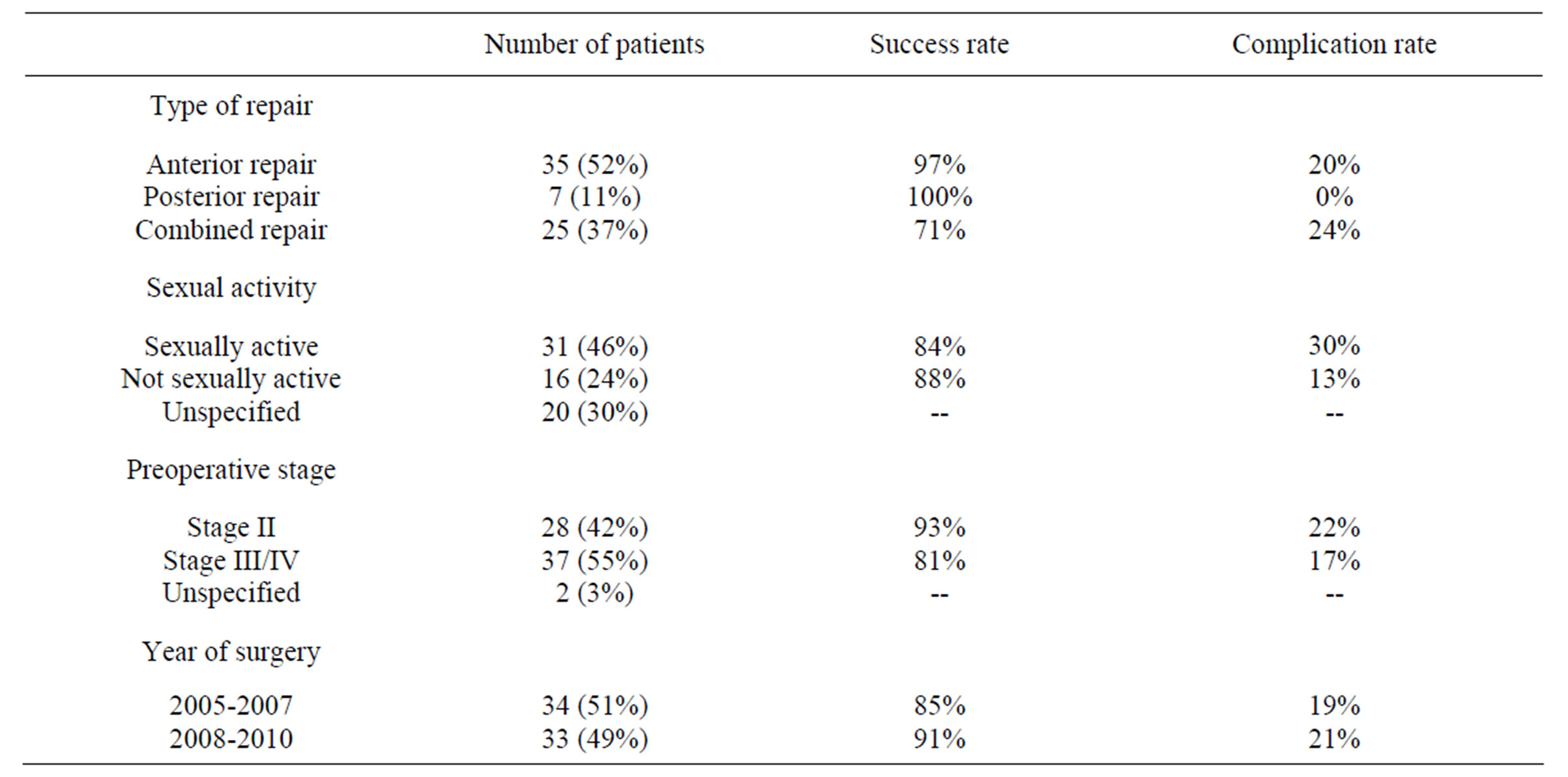
Table 1. Patient characteristics by success rate and complication rate.
Table 2(a) shows univariate and multivariable analysis predicting recurrence. Only combined repair (p = 0.021) was significantly associated with recurrence. Table 2(b) shows univariate and multivariable analysis predicting overall complication. Only age (p = 0.019) was significantly associated with complication. When evaluating the specific complication of mesh exposure (Table 2(c)), younger age (p = 0.018) and combined repair (p = 0.048) were found to be significantly associated with mesh exposure.
Median postoperative hospitalization was one day (range one to three days). Table 3 shows the main postoperative complications stratified by surgical approach. Complications occurred in 13 patients (one hematoma, nine mesh exposures, one dyspareunia, one pelvic pain and one urinary retention in a patient who had a concurrent midurethral sling placement). There were no mesh erosions into adjacent organs. The age, ICS/IUGA classification for prosthesis/graft complication, management and outcome for the patients with mesh-related complications are shown in table 4. Two patients were managed conservatively with vaginal estrogen crème and brief abstinence from intercourse, while the other seven patients underwent transvaginal excision of the exposed mesh with re-approximation of the vaginal epithelium. There were no excision-related complications. In no patient was the defect large enough to require closure with secondary material such as alloderm® or surgisis®.
4. Discussion
Vaginal mesh repair is frequently marketed as an effective and durable alternative to traditional colporrhaphy with an acceptable complication profile. We found an anatomic success rate of 88% (97% for anterior repair,
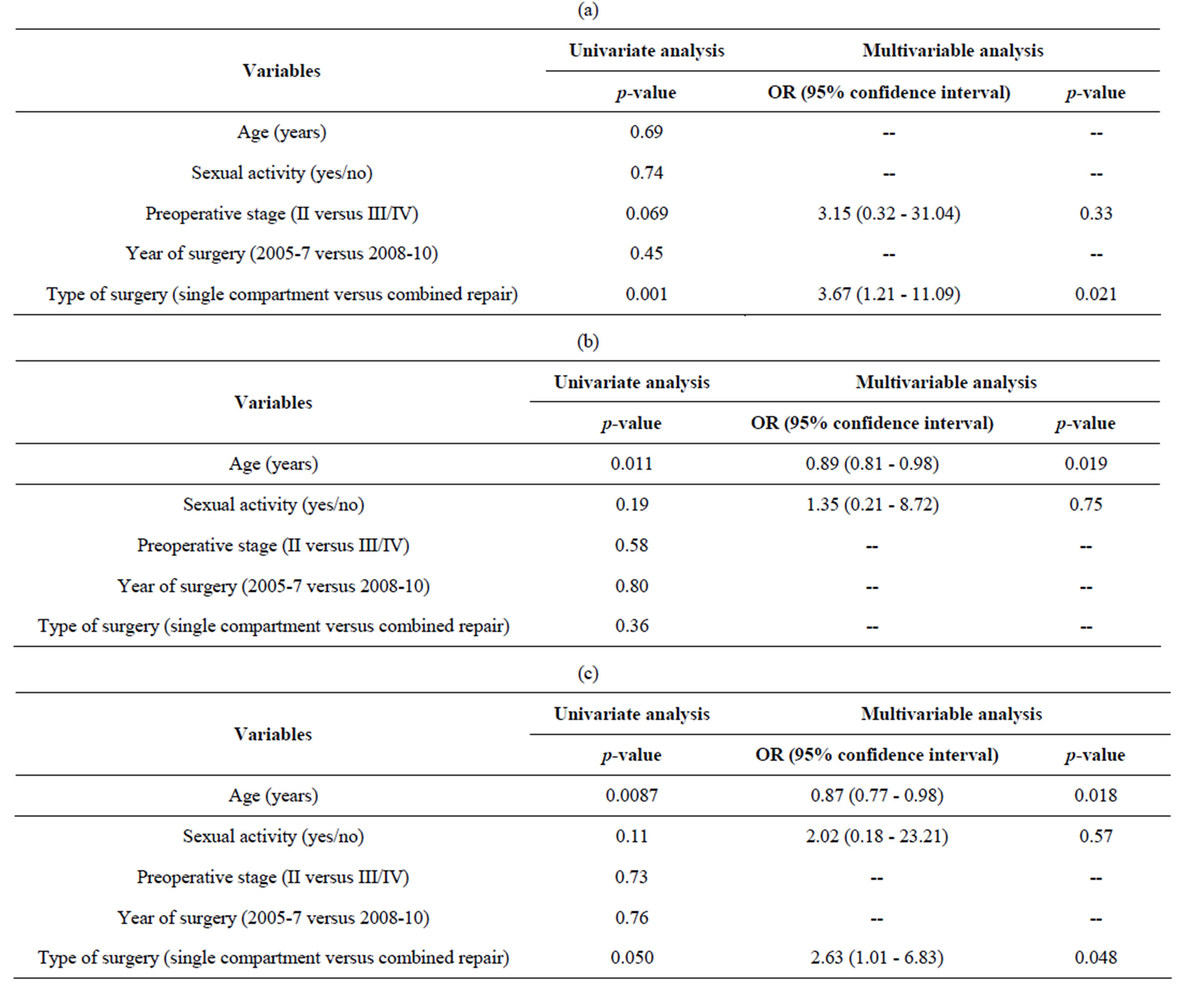
Table 2. Univariate and multivariable models predicting: (a) Recurrence; (b) Overall complication; and (c) Mesh exposure.
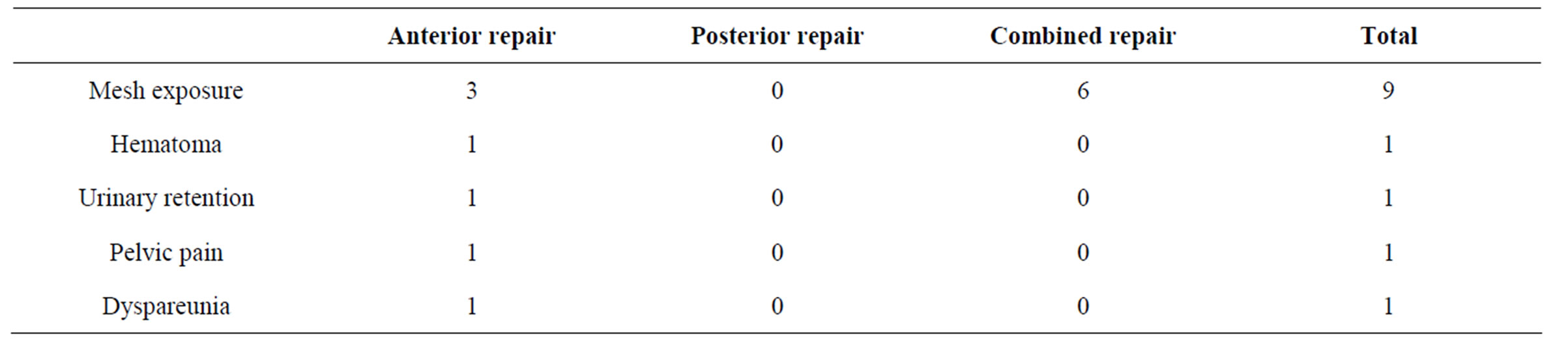
Table 3. Complications stratified by surgical approached.
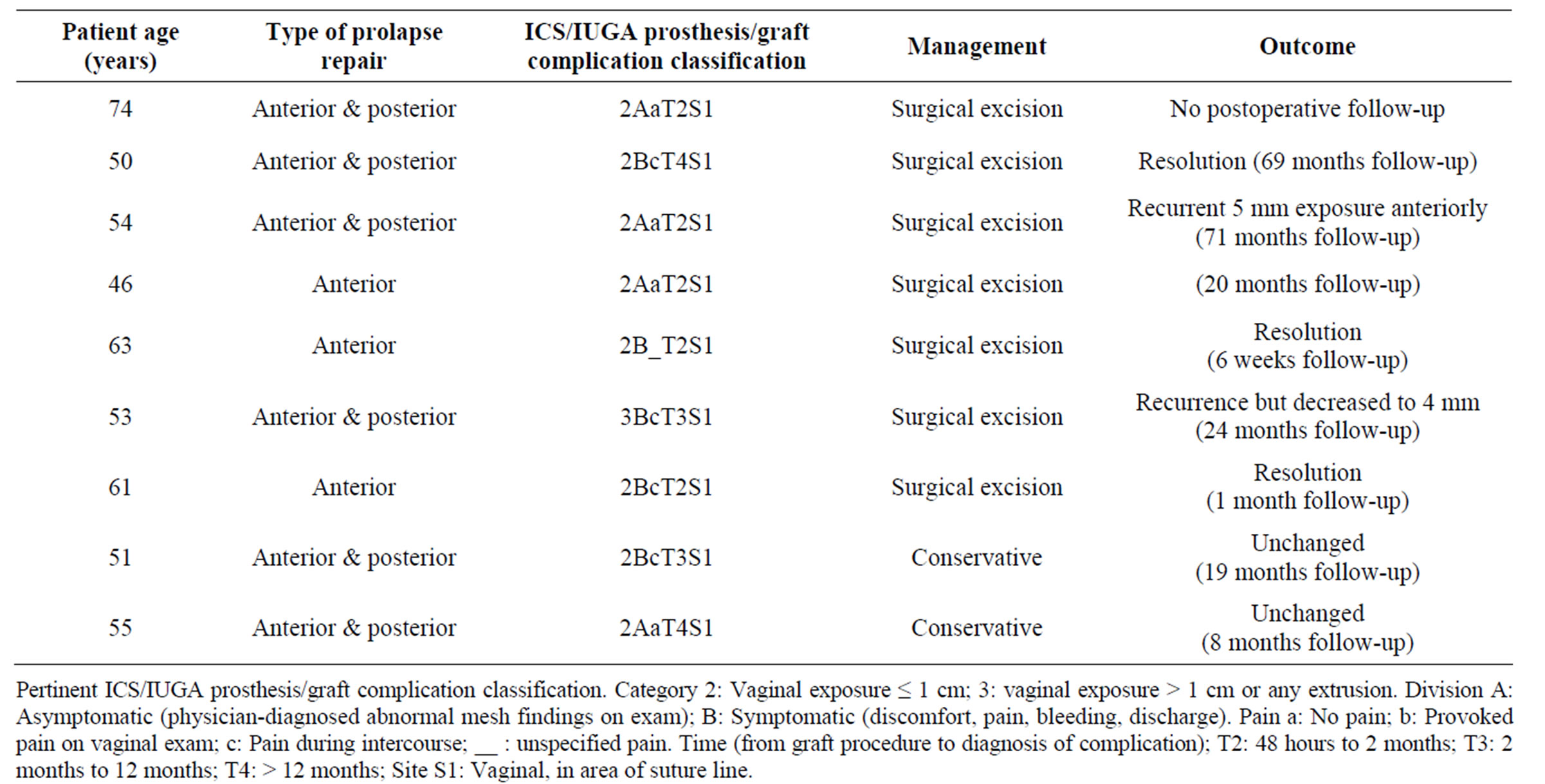
Table 4. Demographic features and clinical findings.
100% for posterior repair and 71% for combined repair) with combined repair being associated with risk of recurrence. Complications occurred in 19% of our population (13 of 67 patients), and were more likely in younger patients. There were nine (13%) mesh exposures and no mesh erosion or perforation into adjacent organ.
Altman and colleagues [10] recently performed a randomized control trial comparing traditional anterior colporrhaphy to TVM for management of anterior vaginal wall prolapse. Their primary outcome measure was a composite of anatomical and subjective endpoints, and they reported superior success with TVM (60.8%) compared to traditional colporrhaphy (34.5%) at 1 year. However, they did find higher rates of complication with TVM, including a 3.5% rate of bladder perforation. Sanses and colleagues in comparing short-term outcomes of vaginal mesh repair to abdominal sacral colpopexy for management of apical prolapse reported an anatomic cure rate of 98.8% for vaginal mesh repair and 99.3% with abdominal sacral colpopexy at three to six months follow-up [3] . A retrospective study of 56 patients who underwent Prolift® vaginal mesh procedures reported a cure rate of 91% at 21 months follow-up [11], and another series of 60 patients with median follow-up of 29 months reported success rate of 85% with 15% rate of mesh exposure [6]. Others have reported rates of mesh exposure between 1% and 25% [12-14] . Van Raalte and colleagues studied 97 patients who underwent anterior, posterior, and total vaginal mesh repair and reported that 94.2% of subjects were cured in the treated compartment [15] . Altman and colleagues in a multicenter trial reported short-term (two months postoperatively) outcomes after vaginal mesh repair and had an 87% anatomic cure rate for anterior repair, 91% cure rate for posterior repair and 88% cure rate for total repair [5]. Thus, our findings of 71% to 100% success rate in the different compartments with best results in posterior repair, as well as our mesh exposure rate of 13% are all consistent with the reported literature.
We noted a higher rate of mesh exposure with combined repair compared to anterior only or posterior only repair. All mesh exposures in our series were at the sites of a suture line. Hence, the higher rate of mesh exposure with combined repair is likely due to a larger suture line with combined repair.
Prior authors [5] have reported a 3.2% rate of pelvic organ perforation and 1.6% rate of vaginal mesh exposures. Likewise other authors reported 2% to 3.5% rate of pelvic organ erosions/injuries and 4.4% rate of vaginal exposures [3,10] . In the current series, there were no instances of mesh erosion or perforation of pelvic organs. We operated on 78% (7 of 9 patients) of our patients with vaginal mesh exposure. Likewise, Carey [16] and colleagues reported operating in 75% of their patients with vaginal mesh exposure. On the contrary, Khong and colleagues [17] managed all of their patients with excision of exposed mesh and closure of the vaginal epithelium with surgisis®; perhaps this is because their patients had exposures of significant size (1 - 4 cm).
Other interesting findings from the current study include the lack of association between year of surgery and all evaluated outcome measures. This may suggest that the learning curve over a six-year period is not a major contributor to outcome in this procedure.
Surprisingly, there was an association between younger age and higher risk for complication. Other authors [18] have found that younger age and sexual activity were significantly associated with mesh exposure in patients who underwent TVM for POP. Interestingly, we did not find an association between sexual activity and complication; our analysis may be limited by the modest sample size. Perhaps lifestyle differences between different age groups may contribute to outcome after TVM.
A concern regarding TVM is that repair of one compartment can predispose to prolapse in an untreated compartment. In our series, six (9%) patients developed prolapse in an unsupported compartment. Since our study design does not allow for comparison with a control group, we cannot determine whether this is a higher rate than is seen after other types of prolapse repair. Another limitation of our study is that we did not assess the subjective success of the procedure. Additionally, our sample size was modest and the study population constitutes a single-surgeon series using the Prolift® device; thus, results may not be generalizable to other settings or vaginal mesh devices. Our study not only adds to a growing body of literature on the risks and efficacy of TVM, but also reports the predictors of outcome after this procedure. Given the rising concern regarding safety of TVM, this information may be useful in selection of appropriate patients to minimize complication and maximize success. The use of the recently developed ICS/ IUGA classification system for prosthesis/graft complication allows standardized reporting of mesh-related complications and could facilitate future compilation of several institutional series into a meta-analysis.
5. Conclusion
TVM has an overall success rate of 88% and complication rate of 19% in the management of POP. Combined repair is associated with risk of failure while younger age is associated with risk of complication. The association between younger age and complication needs to be further elucidated by future studies.
6. Acknowledgements
This project was supported by Award Number T32DK 007552 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
REFERENCES
- A. L. Olsen, V. J. Smith, J. O. Bergstrom, J. C. Colling and A. L. Clark, “Epidemiology of Surgically Managed Pelvic Organ Prolapse and Urinary Incontinence,” Obstetrics & Gynecology, Vol. 89, No. 4, 1997, pp. 501-506. doi:10.1016/S0029-7844(97)00058-6
- A. M. Weber, M. D. Walters, M. R. Piedmonte and L. A. Ballard, “Anterior Colporrhaphy: A Randomized Trial of Three Surgical Techniques,” American Journal of Obstetrics & Gynecology, Vol. 185, No. 6, 2001, pp. 1299-1304. doi:10.1067/mob.2001.119081
- T. V. Sanses, A. Shahryarinejad, S. Molden, et al., “Anatomic Outcomes of Vaginal Mesh Procedure (Prolift) Compared with Uterosacral Ligament Suspension and Abdominal Sacrocolpopexy for Pelvic Organ Prolapse: A Fellow’s Pelvic Research Network Study,” American Journal of Obstetrics & Gynecology, Vol. 201, No. 5, 2009, pp. 1-8.
- “FDA Safety Communication: UPDATE on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse,” 2011. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm262435.htm
- D. Altman, T. Vayrynen, M. E. Engh, S. Axelsen and C. Falconer, “Short-Term Outcome after Transvaginal Mesh Repair of Pelvic Organ Prolapse,” International Urogynecol Journal of Pelvic Floor Dysfunction, Vol. 19, No. 6, 2008, pp. 787-793. doi:10.1007/s00192-007-0526-2
- R. Nair, A. Nnochiri, C. Barnick and C. Roberts, “Transvaginal Mesh (ProliftTM) Repair: 2-Year Anatomic Outcomes,” European Journal of Obstetrics, and Gynecology Reproductive Biology, Vol. 158, No. 2, 2011, pp. 358- 360.
- R. C. Bump, A. Mattiasson, K. Bo, et al., “The Standardization of Terminology of Female Pelvic Organ Prolapse and Pelvic Floor Dysfunction,” American Journal of Obstetrics Gynecology, Vol. 175, No. 1, 1996, pp. 10- 17. doi:10.1016/S0002-9378(96)70243-0
- B. T. Haylen, R. M. Freeman, S. E. Swift, et al., International Urogynecological Association, International Continence Society and Joint IUGA/ICS Working Group on Complications Terminology, “An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Terminology and Classification of the Complications Related Directly to the Insertion of Prostheses (Meshes, Implants, Tapes) and Grafts in Female Pelvic Floor Surgery,” Neurourology Urodynamics, Vol. 30, No. 1, 2011, pp. 2-12.
- “Prolift Website,” 2012. http://www.ethicon360.com/sites/default/files/products/PRO-294-11_PROLIFT_IFU.pdf
- D. Altman, T. Vayrynen, M. E. Engh, S. Axelsen and C. Falconer, “Anterior Colporrhaphy Versus Transvaginal Mesh for Pelvic-Organ Prolapse,” New England Journal of Medicine, Vol. 364, No. 19, 2011, pp. 1826-1836.
- L. O. Gagnon and L. M. Tu, “Mid-Term Results of Pelvic Organ Prolapse Repair Using a Transvaginal Mesh: The Experience in Sherbooke, Quebec,” Canadian Urological Association Journal, Vol. 4, No. 3, 2010, pp. 188-191.
- Committee on Gynecologic Practice, “Committee Opinion No. 513: Vaginal Placement of Synthetic Mesh for Pelvic Organ Prolapse,” The American College of Obstetricians and Gynecologists, Vol. 118, No. 6, 2011.
- C. Birch, “The Use of Prosthetics in Pelvic Reconstructive Surgery,” Best Practice & Research Clinical Obstetrics & Gynaecology, Vol. 19, No. 6, 2005, pp. 979-991. doi:10.1016/j.bpobgyn.2005.08.013
- T. M. Julian, “The Efficacy of Marlex Mesh in the Repair of Severe, Recurrent Vaginal Prolapse of the Anterior Midvaginal Wall,” American Journal of Obstetrics & Gynecology, Vol. 175, No. 6, 1996, pp. 1472-1475. doi:10.1016/S0002-9378(96)70092-3
- H. M. van Raalte, V. R. Lucente, S. M. Molden, R. Haff and M. Murphy, “One-Year Anatomic and Qualityof-Life Outcomes after the Prolift Procedure for Treatment of Posthysterectomy Prolapse,” American Journal of Obstetrics & Gynecology, Vol. 199, No. 6, 2008, pp. 1-6.
- M. Carey, P. Higgs, J. Goh, et al., “Vaginal Repair with Mesh versus Colporrhaphy for Prolapse: A Randomised Controlled Trial,” BJOG: An International Journal of Obstetrics & Gynaecology, Vol. 116, No. 10, 2009, pp. 1380-1386. doi:10.1111/j.1471-0528.2009.02254.x
- S. Y. Khong and A. Lam, “Use of Surgisis Mesh in the Management of Polypropylene Mesh Erosion into the Vagina,” International Urogynecological Journal, Vol. 22, No. 1, 2011, pp. 41-46.
- Y. Kaufman, S. S. Singh, H. Alturki and A. Lam, “Age and Sexual Activity Are Risk Factors for Mesh Exposure Following Transvaginal Mesh Repair,” International Urogynecol Journal of Pelvic Floor Dysfunction, Vol. 22, No. 3, 2011, pp. 307-313.
NOTES
*Corresponding author.

