Surgical Science
Vol. 3 No. 12 (2012) , Article ID: 25326 , 4 pages DOI:10.4236/ss.2012.312114
Colonoscopy in Elderly Patients with Hemorrhoidal Disease and Average-Risk for Colorectal Cancer, a Qatari Community Hospital Experience
1Department of General Surgery, Al Khor Hospital, Hamad Medical Corporation, Doha, Qatar
2Department of Medicine, Al Khor Hospital, Hamad Medical Corporation, Doha, Qatar
3Department of Geriatric Medicine, Al Amal Hospital, Hamad Medical Corporation, Doha, Qatar
Email: hennawyhany@hotmail.com
Received September 22, 2012; revised October 24, 2012; accepted November 4, 2012
Keywords: Colonoscopy; Elderly; Hemorrhoidal Disease; Colorectal Cancer
ABSTRACT
Introduction: Hemorrhoids are a frequent and familiar concern of patients in the general practice and surgery settings. Colonoscopy is both diagnostic and therapeutic. In Qatar, There are little data available about coincidental pathology in elderly patients with hemorrhoids. Objective: To assess the outcome of colonoscopy in management patients with hemorrhoidal disease and average-risk for colorectal cancer and its clinical significance. Method: A retrospective study of 200 patients with hemorrhoids with average risk colorectal cancer (anal bleeding and anal symptoms) and subjected to colonoscopic examination at Al Khor hospital’s endoscopy unit during the period from May 2005 till August 2012. Patients below 50 years and high risk patients for colorectal cancer; with the following alarm signs: Positive personal history of colorectal neoplasms or Inflammatory Bowel Disease (IBD), positive first degree family history of colorectal neoplasms, history of altered bowel habits, recent significant weight loss, presence of iron deficiency anemia, and history of previous colonoscopy were excluded. All significant endoscopic co-findings (diverticuli, polyps, cancer, angiodysplasia and varices, or colitis) were recorded. Results: There were 200 patients; 134 male, 66 female; Mean patient age was 56.3 years (range, 50 to 82 years), who met the eligibility criteria. 200 colonoscopies were performed. Evaluation of these patients revealed Polyps in 16 patients (13 benign and 3 malignant), seven malignant lesions(one annular lesion and 6 fungating masses), Ulcerative colitis in 5 patients, no crohn’s disease, diverticular disease in 4 patients, no Vascular malformations, bleeding piles in 3 patients controlled by injection, and 65.5% of patients were free from any additional pathology. Colonoscopy changed the treatment plan in 58 patients (29%). No complications were encountered. Conclusion: Coincidental abnormalities in colon and rectum in elderly patients with hemorrhoids are common. Benign polyps, followed by diverticular diseases, anal fissures then colorectal cancer were the commonest findings. Endoscopic evaluation of elderly patients with hemorrhoids and average risk for colorectal cancer is advocated. Omitting endoscopy in these patients can lead to major doctors’ delay.
1. Introduction
Hemorrhoids are a common surgical problem and affect about 4 percent of population [1] Symptomatic hemorrhoids affect at least 50% of the American population at some time during their lives, with around 5% of the population suffering at any given time, and both sexes experiencing the same incidence of the condition [2]. The aetiopathogenesis remains unclear. Progressive degeneration of the fibromuscular structure of the internal hemorrhoidal plexus may be the reason [3]. Many other abnormalities in the rectum and colon can be responsible for rectal bleeding [4]. The relationship between rectal bleeding and colorectal cancer has been studied. However, the relationship between rectal bleeding, hemorrhoids and other pathology is not clear. Rectal bleeding is one of the commonest symptoms of colorectal cancer, but more often, it is because of benign pathology. It is generally regarded as a symptom of early colorectal cancer. Rectal bleeding of any nature in primary care is considered a “mandatory referral symptom”, requiring investigation in secondary care [5]. Rectal bleeding in patients with hemorrhoids requires exact diagnosis because it may be not simply a hemorrhoidal bleeding and can be an early sign of severe bowel diseases, such as colon carcinoma, or inflammatory bowel diseases that could be discovered by colonoscopy [6]. Age is the number one risk factor for colorectal cancer. More than 90% of people diagnosed with the disease are 50 or older and the average age of diagnosis is 64.
2. Methods
A retrospective study of 200 patients with hemorrhoids clinically diagnosed in anorectal clinic with average risk colorectal cancer (anal bleeding and anal symptoms) and referred to Al Khor hospital’s endoscopy unit for Colonoscopy, during the period from May 2005 till August 2012. Patients below 50 years and patients with the following alarm signs were excluded: Positive personal history of colorectal neoplasms or Inflammatory Bowel Disease (IBD), positive first degree family history of colorectal neoplasms, history of previous colonoscopy, history of altered bowel habits, recent significant weight loss, and presence of iron deficiency anemia. All patients were interviewed and examined by a gastroenterologist. Informed written consent was obtained from each patient before interview according to the guidelines of the institute. After clinical evaluation, all patients underwent anal inspection and digital rectal examination. Regardless of any anal pathologies detected, all patients underwent colonoscopy. Endoscopy was performed, by expert endoscopists, after ingestion of Dulcolax tablets (Bisacodyl) 5 mg (6 tablets) starting the day before the procedure and for colonoscopy ingestion of 4 to 6 liters of polyethylene glycol solution starting the day before the procedure. Colonoscopies were performed as outpatient procedures, with patients under conscious sedation using intravenous midazolam and fentanyl. All significant endoscopic cofindings (diverticuli, polyps, cancer, angiodysplasia and varices, or colitis); location and size were recorded, analyzed, and discussed and the polyps were removed if technically possible. Any abnormal lesion was biopsied and sent for histology. IBD was diagnosed based on colonoscopy features and histopathological findings. A complete examination was defined as the endoscope reaching the cecum, as documented in a photograph of the cecal pole. Procedure-related complications and hospitalizations were documented for 30 days following each colonoscopy. Patients with poor bowel preparation were scheduled for repeat colonoscopy and the results of a satisfactory examination are reported. Only the first endoscopy, done in a patient was included. The results of endoscopy were noted in a standardized endoscopy report; from May 2005 till mid 2008 handwritten and from 2008 using the EndosoftTM computerized system. Data collected from all patients are summarized in Tables 1 and 2. The study was approved by the hospital ethical research committee.
3. Statistical Analysis
Data entry and analysis were performed using the Statistical Packages for Social Sciences version 15 (SPSSChicago, Illinois, USA). Descriptive statistics were calculated for continuous variable such as age. Mean ± SD were computed. For categorical variables such as sex and type of lesion, the frequencies and percentages were calculated.
4. Results
There were 200 patients; 134 male, 66 female; Mean patient age was 56.3 years (range, 50 to 82 years) who met the eligibility criteria. Commonest presenting complaints were nonspecific to hemorrhoidal disease; anal pain 62%, bleeding per rectum 42.5%, itching 14.5%, then prolapsed piles 10%. Second degree piles in 92 patients (46%), third degree piles in 88 patients (44%) and fourth degree piles in 20 patients (10%). Associated anal fissures were found in 4% of patients while perianal fistulas were found in 3%of patients. 16.5% of patients had history of previous anal surgeries [hemorrhoidectomy (n 21); Conventional hemorrhoidectomy in 18 patients while Stapled hemorrhoidectomy (Procedure for Prolapse and Hemorrhoids [PPH] was done in 3 patients, and lateral internal sphincterotomy (n12)]. 200 colonoscopies were performed. Evaluation of these patients revealed Polyps in 16 patients (13 benign and 3 malignant), seven malignant lesions (one annular lesion and 6 fungating masses), all of which were located in the distal colon. A concomitant proximal significant lesion was found in 2 patients (1%); in both patients there were proximal and distal benign polyps. Ulcerative colitis in five patients, no crohn’s disease, diverticular disease in 12 patients (6%), no vascular malformations, bleeding piles in three patients controlled by injection, and 74.5% of patients were free from any additional pathology. No deflation, stenting, or mucosal resections were performed. 147 patients were scheduled for regular outpatient clinic follow up; while 77 patients received antihemorrhoidal medication, five patients received anti-inflammatory medications for inflammatory bowel disease. Colonoscopy changed the treatment plan in 58 patients (29%). 10 patients were referred to oncologic consultations. 65 patients were subjected to hemorrhoidectomy and 10 patients (5%) diagnosed with cancer subjected to conventional open low anterior resection. No procedure-related deaths occurred. No complications such as perforation and hemorrhage were encountered. Incomplete procedures (failed cecal intubation) in 17 patients; five patients did not tolerate the procedure, eleven patients had bad preparations and one had a stenotic lesion.
5. Discussion
Rectal bleeding is a common symptom, with a prevalence of 14% to 19% in adults. Most patients bleed from
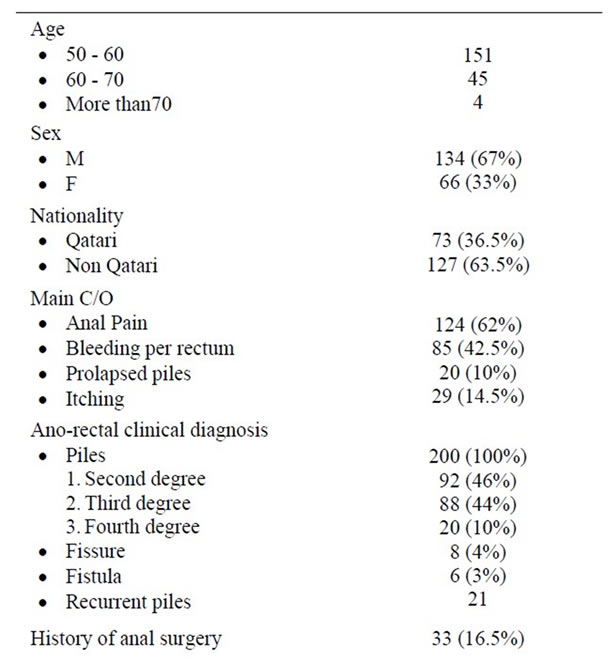
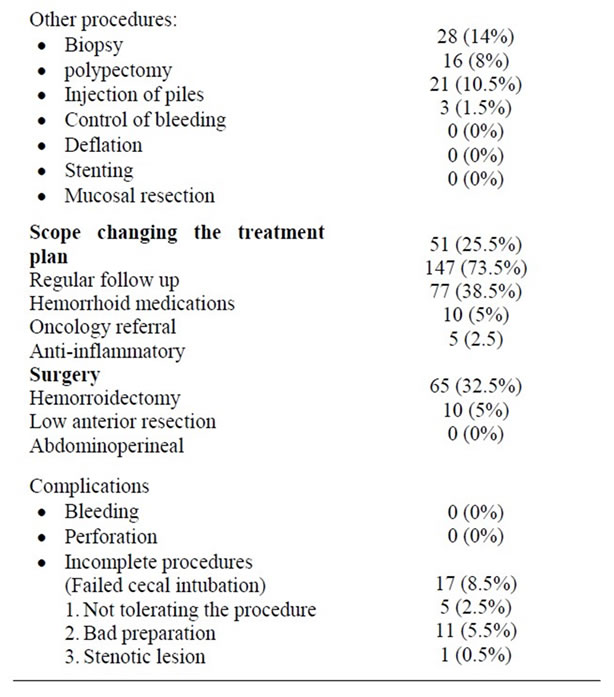
Table 1. Results.
benign sources such as hemorrhoids and diverticula, but others have serious colorectal disease including colon cancer, adenomatous polyps, and inflammatory bowel disease. The optimal evaluation strategy for rectal bleeding is unknown. Neither historical information nor the presence or absence of hemorrhoids has been shown to reliably differentiate benign from serious disease [7]. Patients complaining of rectal bleeding with anal symptoms; local cause such as hemorrhoids, or an anal fissure
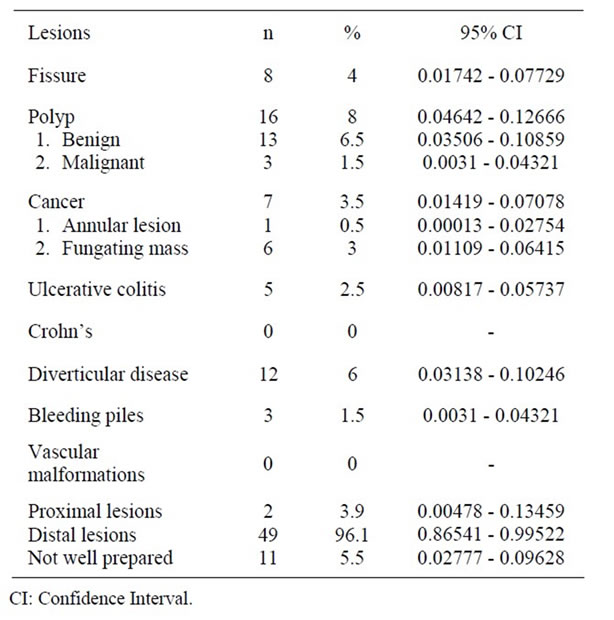
Table 2. Endoscopic findings.
are considered low risk group. Rectal bleeding is reported less in older age groups [8]. Previous studies of colonoscopy in symptomatic and asymptomatic elderly patients have consistently shown a high prevalence of colorectal neoplasia [9]. In patients with hemorrhoids other abnormalities can be present. In recent guidelines on rectal bleeding, age is an important discriminant in diagnostic tactics [10]. Especially in older patients the clinician must be cautious to attribute complaints solely to hemorrhoids. Furthermore, endoscopic co-findings were found with increasing age [11]. With regard to the patients with known hemorrhoids, the guideline are based on an expert’s opinion because there are few data on when to suspect other pathology in a patient with hemorrhoids [10].
However, opinions still differ on the subject whether or not to do colonoscopy in cases of complaints possibly due to hemorrhoids. It is stated that a full colonoscopy is necessary in all patients, regardless the age [12]. Some authors have recommended colonoscopy in all patients with rectal bleeding, while others prefer colonoscopy for patients over 50 years of age and recommend sigmoidoscopy only if a potential source of bleeding is not identified on physical examination or anoscopy/proctoscopy [13]. In common practice, the age of 50 years holds the threshold for colonoscopy since the incidence of colorectal cancer, diverticulosis and polyps increases as people are getting older [14]. Our study is a confirmation of previous results on coincidental abnormalities in colon and rectum in elderly patients with hemorrhoids. Endoscopic lesions are found mostly in the distal colon (94%) and hence flexible sigmoidoscopy seems to be a reasonable evaluation tool in elderly patients with no other alarm symptoms. benign polyps, followed by diverticular diseases, anal fissures then colorectal cancer were the commonest findings. Colonoscopy changed the patients’ management plans in 25.5% of patients so we do strongly recommend endoscopic evaluation of elderly patients with hemorrhoids and low risk for colorectal cancer.
6. Limitations of the Study
This was a single-center study in a community hospital. There may be a referral bias as not all patients with hemorrhoids are referred for endoscopy. More randomized prospective clinical trials in elderly patients with a large sample size are needed from this region before making any firm recommendations regarding the most appropriate modality for the evaluation of patients with hemorrhoids and low risk colorectal cancer. Nevertheless, this is one of the initial studies of its kind from north Qatar.
7. Conclusion
In our study, the most frequent diagnoses were benign polyps, followed by diverticular diseases, anal fissures then colorectal cancer. Colonoscopies were safe and no complications were recorded. Majority of endoscopic lesions were found mostly in the distal colon hence flexible sigmoidoscopy seems to be a reasonable evaluation tool in elderly patients with hemorrhoids and average risk for colorectal cancer. A move towards a lower threshold for referral and increased use of diagnostics might be a more reliable option for early diagnosis.
REFERENCES
- J. F. Johanson and A. Sonnenberg, “The Prevalence of Hemorrhoids and Chronic Constipation. An Epidemiologic Study,” Gastroenterology, Vol. 98, No. 2, 1990, pp. 380- 386.
- S. Lorenzo-Rivero, “Hemorrhoids: Diagnosis and Current Management,” The American Surgeon, Vol. 75, No. 8, 2009, pp. 635-642.
- R. Vanheuverzwyn, J. F. Colin, T. van Wymersch, A. Kartheuser and P. Hoang, “Hemorrhoids Review,” Acta Gastro-Enterologica Belgica, Vol. 58, No. 5-6, 1995, pp. 452- 464.
- J. L. Pfenninger and G. G. Zainea, “Common Anorectal Conditions: Part I. Symptoms and Complaints,” American Family Physician, Vol. 63, No. 12, 2001, pp. 2391-2398.
- R. Lawrenson, J. Logie and C. Marks, “Risk of Colorectal Cancer in General Practice Patients Presenting with Rectal Bleeding, Change in Bowel Habit or Anaemia,” European Journal of Cancer Care, Vol. 15, No. 3, 2006, pp. 267-271. doi:10.1111/j.1365-2354.2005.00637.x
- F. Pigot, “Haemorrhoidal Disease,” Revue du Praticien, Vol. 58, No. 16, 2008, pp. 1763-1768.
- M. D. Elizabeth-Allen, M. D. Christina-Nicolaidis, Mark and M. D. Helfand, “The Evaluation of Rectal Bleeding in Adults a Cost-Effectiveness Analysis Comparing Four Diagnostic Strategies,” Journal of General Internal Medicine, Vol. 20, No. 1, 2005, pp. 81-90. doi:10.1111/j.1525-1497.2005.40077.x
- W. Hamilton and D. Sharp, “Diagnosis of Colorectal Cancer in Primary Care: The Evidence Base for Guidelines,” Family Practice, Vol. 21, No. 1, 2004, pp. 99-106. doi:10.1093/fampra/cmh121
- O. S. Lin, R. A. Kozarek, D. B. Schembre, K. Ayub, M. Gluck, F. Drennan, M.-S. Soon and L. Rabeneck, “Screening Colonoscopy in Very Elderly Patients Prevalence of Neoplasia and Estimated Impact on Life Expectancy,” The Journal of the American Medical Association, Vol. 295, No. 20, 2006, pp. 2357-2365.
- M. V. Koning and R. J. L. F. Loffeld, “Rectal Bleeding in Patients with Haemorrhoids, Coincidental Findings in Colon and Rectum,” Family Practice, Vol. 27, No. 3, 2010 pp. 260-262. doi:10.1093/fampra/cmq008
- M. V. Koning and R. J. L. F. Loffeld, “A Survey of Abnormalities in the Colon and Rectum in Patients with Haemorrhoids,” BMC Gastroenterology, Vol. 10, No. 74, 2010, p. 74. doi:10.1186/1471-230X-10-74
- R. F. Wong, R. Khosla, J. H. Moore and S. K. Kuwada, “Consider Colonoscopy for Young Patients with Hematochezia,” The Journal of Family Practice, Vol. 53, No. 11, 2004, pp. 879-884.
- S. Nikpour and A. Asgari, “Colonoscopic Evaluation of Minimal Rectal Bleeding in Average-Risk Patients for Colorectal Cancer,” World Journal of Gastroenterology, Vol. 14, No. 42, 2008, pp. 6536-6540. doi:10.3748/wjg.14.6536
- A. Jemal, R. Siegel, E. Ward, et al., “Cancer Statistics,” CA: A Cancer Journal for Clinicians, Vol. 58, No. 2, 2008, pp. 71-96. doi:10.3322/CA.2007.0010

