International Journal of Clinical Medicine
Vol.3 No.3(2012), Article ID:19385,6 pages DOI:10.4236/ijcm.2012.33037
A Study on Stroke in Young and Elderly in Rajiv Gandhi Government General Hospital, Chennai
![]()
1Institute of Internal Medicine, Rajiv Gandhi Government General Hospital (RGGGH), Chennai, India; 2Madras Medical College, Chennai, India.
Email: iim.rgggh@gmail.com
Received March 12th, 2012; revised April 20th, 2012; accepted May 10th, 2012
Keywords: Cardiac Disease; Cerebral Infarction; Intracerebral Hemorrhage; Recurrent Pregnancy Loss; Recurrent Stroke; Stroke; Young Stroke
ABSTRACT
Stroke is a devastating and disabling cerebrovascular disease with some amount of residual deficit leading onto economic loss. Recent Indian studies have shown a stroke prevalence rate of 471.58/100,000 population. This study was undertaken to analyse the clinical profile and to arrive at important factors contributing to stroke in <45 years group and >45 years group. This is a descriptive, retrospective cross—sectional study carried out on acute CVA patients, admitted to the I.I.M., RGGGH, Chennai. 150 patients were studied over a period of 3 months in the 2011. 20% of <45 years (young stroke) and 80% >/= 45 years constituted our study population. 18.4% and 22.2% of males and females respectively were young stroke patients. Only 33.3% of patients were brought to the hospital within 6 hours. 90% patients had mild GCS score (>/=13/15) and presented with hemiplegia 76% and 18% had infarct and intracerebral hemorrhage(ICH) respectively. Risk factors: Type A personality (70.7%), Tobacco (60.7%) and Alcohol (44.7%) abuse, Systemic Hypertension (60.7%), Diabetes Mellitus (33.3%), Cardiac disorders (14%). Stroke was seen to be more common in >45 years but still young stroke carries paramount importance due to loss of productive years in these patients. Female predominance was seen in young stroke, with particular reference to puerperal period. Among the comorbid illness systemic hypertension followed by cardiac disorders had important contributing role in young strokes. Most of the patients with infarct and ICH were tobacco and alcohol abusers respectively. A holistic approach encompassing further research in factors involved in young stroke, public awareness, behavioural modification and comorbid medical illness management is the need for the hour.
1. Introduction
Stroke is a devastating and disabling cerebrovascular disease with significant amount of residual deficit leading on to economic loss. It has been defined as a rapidly developing signs of focal (or global) disturbance of cerebral function with symptoms lasting for ≥24 hours, or leading to death with no apparent cause other than vascular origin [1]. It is a collection of clinical syndromes resulting from cerebral ischemia to intracranial hemorrhage. In the west, it is the 3rd most common cause of morbidity and mortality [2]. Though India was ranked among countries lacking sufficient stroke research data [3], some of the recent studies have elucidated the stroke pattern to considerable extent in our country with a prevalence rate of 471.58/100,000 population [4]. Despite many studies prevail regarding stroke, still this major illness remain widely prevalent. Hence this study was undertaken to delineate the various aspects of stroke in our setup which shall be of immense use to the physicians who are required to manage the patients disabled by stroke. This study was conducted on acute cerebrovascular accidents (CVA) patients admitted to the Institute of Internal Medicine, Rajiv Gandhi Government General Hospital, Chennai, to assess and analyse the epidemiological, clinical and risk factor profile of these stroke victims with particular reference to <45 years (young stroke) and >45 years age groups.
2. Material & Methods
This is a descriptive, retrospective, cross sectional study carried out on Acute CVA Patients admitted to the Institute of Internal Medicine, Rajiv Gandhi Government General Hospital, Chennai. Patients admitted for hemiparesis other than CVA were excluded from the study. Sample size was 150 CVA patients. This study was conducted over a period of 3 months during the year 2011. Patient data collection forms were used to collect data on age, sex, educational status, occupation, Glascow Coma Scale (GCS) score, time of occurrence, time lapse, clinical profile and risk factors—Chronic Medical Illness—Systemic Hypertension (HT): Diagnosed and/or under treatment, Diabetes Mellitus (DM): Diagnosed and/or under treatment, Cardiac disorders (Ischemic heart disease, valvular heart disease, atrial fibrillation, cardiomyopathy, congenital heart diseases): Diagnosed and/or under treatment.
Adverse Personal Habits—Tobacco Abuse (Smoking, Chewing, Snuff), Alcohol abuse.
Personality Types—Type A: Ambitious, Aggressive, highly competitive; Type B: Apathetic, Patient, relaxed. Type A may be associated with cardiovascular diseases.
Statistical analysis was done by Pearson chi square test using SPSS 17.0 version software.
3. Results
Our study population consisted of 150 CVA patients of which 20% (n = 30) were <45 years (young stroke) and 80% (n = 120) were >45 years. Under the young stroke category 53.3% (n = 16) were males and 46.7 (n = 14) were females. >45 years group consisted 59.2% (n = 71) of males and 40.8% (n = 49) of females. Among the males and females, young stroke constituted 18.4% (n = 16) and 22.2% (n = 14) respectively. 52% (n = 78) of our study population were illiterates and 48% (n = 72) were literates. 50% (n = 15) of <45 years and 52.5% (n = 64) of >45 years were illiterates. Of the 41.3% (n = 62) unemployed. 33.3% (n = 10) and 43.3% (n = 52), among males and females were unemployed respectively. With respect to the golden period of 6 hours, 33.3% (n = 50) were brought to the medical attention within this period. 33.3% (n = 10) of <45 years and 33.3% (n = 40) of >45 years were brought within this “Golden Period” (Table 1).
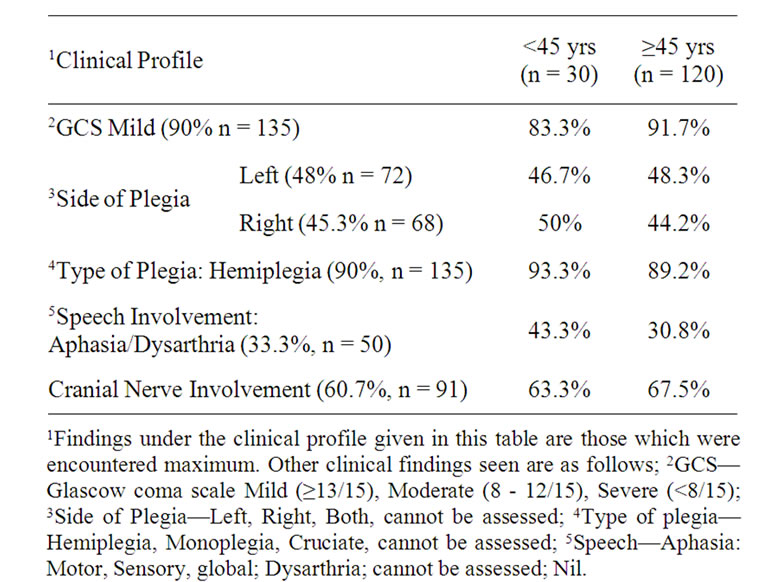
Table 1. Clinical profile in <45 years and ≥45 years.
The pathology encountered in plain Computed Tomography (CT) brain was infarct in 76% (n = 14) and intracerebral hemorrhage (ICH) in 18% (n = 27). However no subarachnoid hemorrhage was encountered in the study. 73.6% (n = 22) of <45 years and 76.7% (n = 92) of ≥45 years had infarct. 16.7% (n = 5) of <45 years and 18.3% (n = 22) of ≥45 years had ICH. 72% (n = 108) of our patients had CVA during work of which 92.6% (n = 100) had identifiable pathology in plain CT brain. Under this 85% (n = 85) had infarct and 15% (n = 15) had ICH. 28% (n = 42) developed stroke during sleep/as soon as waking up, of which of whom 71.4% (n = 30) had infarct and 28.6% (n = 12) had ICH. 73.9% (n = 85) of infarcts and 55.6% (n = 15) of ICH occurred during work. 26.1% (n = 30) of infarct and 44.4% (n = 12) of ICH occurred during sleep/as soon as waking up.
Considering the site of involvement of stroke in the brain, subcortex accounted for 52.7% (n = 79). 43.3% (n = 13) of <45 years and 55% (n = 66) of >45 years had subcortical involvement. Other sites involved were subcortex + cortex in 18.7% (n = 28), only cortex in 15.3% (n = 23) etc.
Of the female young stroke patients, 21.4% (n = 3) were in puerperal period and 28.6% (n = 4) had a positive history of recurrent pregnancy loss. 60.9% (n = 70) of patients with infarct and 59.3% (n = 16) of patients with ICH were tobacco abusers. 43.5% (n = 50) of patients with infarct and 55.6% (n = 15) of patients with ICH were alcohol abusers. 6% (n = 9) of cases had history of recurrent CVA. 10% (n = 3) of <45 years and 5% (n = 6) of ≥45 years had recurrent CVA.
4. Discussion
As with prior articles [5], in this study also the peak incidence of stroke is in ≥45 years age group. Though majority of case (80%) were seen in the elderly, stroke in the young carries special importance as they form the most productive age group. Young stroke has increased in the recent times with changing lifestyles and better diagnostic modalities. In accordance with prior Indian studies, our study population had 20% young strokes [6]. Considering the sex ratio, female predominance is seen in young stroke victims [7]. It is evident from this study as 22.2% of female young stroke patients in contrast to males –18.4%. Assessment of educational and occupational status revealed that ≥45 years age group had more number of Illiterates and unemployed. Stroke is a quintessential medical emergency. CVA patients who receive neurological care within 6 hours of onset of symptoms have a 4 fold greater chance of good outcome than those treated after this acute period [8]. In this study the proportion of <45 years and ≥45 years who were brought within 6 hours were found to be equal.
In this study majority of them were right handed individuals, with only 3 left handed patients. So this data did not have significant impact on the study outcome.
Non contrast computed tomography brain is the first imaging modality adopted in CVA patients as it reliably distinguishes acute ICH from ischemia [9]. In this study also pathological process involved in the causation of stroke was evaluated using plain CT brain. In accordance to prior studies conducted in India, cerebral infarction was major pathology encountered (76%) [10]. Recent Indian Stroke studies have shown ratio between infarction: ICH is 2.21:1 (Western countries—5:1) [11,12]. However in this study the ratio is 4.2:1. In both the age groups, infarction was the predominant pathology. Also infarction was the major pathology in both who had CVA during work and during sleep/as soon as waking up. 52.7% of the patients had only subcortical involvement which was the most common site seen in this study. ≥45 years exceeded <45 years in subcortical involvement by 11.7%.
Identification of risk factors for stroke [13] as well as an awareness of the relative importance of each and their interaction carries prime importance in the pathological outcome in both these age groups. Though innumerable risk factors exist for the occurrence of stroke, the most salient and common ones encountered in our setup and those risk factors whose modification has a great positive impact on the occurrence and outcome of stroke has been considered in this study [14]. DM, HT, Cardiac disorders, Smoking and long term Alcohol consumption are major risk factors in young adults as in elder population [15].
They are—Chronic Medical Illness such as—Hypertension [16], Diabetes Mellitus [17], Cardiac Disorders [18]; Adverse Personal Habits such as—Tobacco Abuse [19, 19], Alcohol Abuse [21]; Personality Types such as— Type A, Type B [22]. As far as the chronic medical illness is considered, the most common encountered is the HT seen in 60.7% of patients, followed by DM (33.3%) and cardiac disorders (14.1%) [20,23] (Figure 1).
Study of pattern of past medical illness in patients with infarct, showed that large number of patients were hypertensives (29.8%) followed by the combination of HT + DM and DM + HT + cardiac disorders (6.1%) (Figure 2).Whereas in patients with ICH, 33.3% had DM + HT followed by only HT (18.5%) (Figure 3). Among the adverse habits, tobacco abuse was seen in the majority of patients (60.7%). Most of the patients with infarct were tobacco abusers (6.9%) and in those with ICH were alcohol abusers (55.6%) (in accordance to prior studies) [24] (Table 2). Interestingly 70.1% of our study population had Type A personality, of whom males predominated.
In assessing the combination and their effects of risk factors, tobacco abuse and hypertension appear to act synergistically as stroke risk factors [25] which was evident in this study also by the following data—hypertensive tobacco abusers were 60.43% in contrast to only hypertensives without tobacco abuse were only 39.57%. Similar relation of tobacco abuse with DM [26] and cardiac disorders was seen.
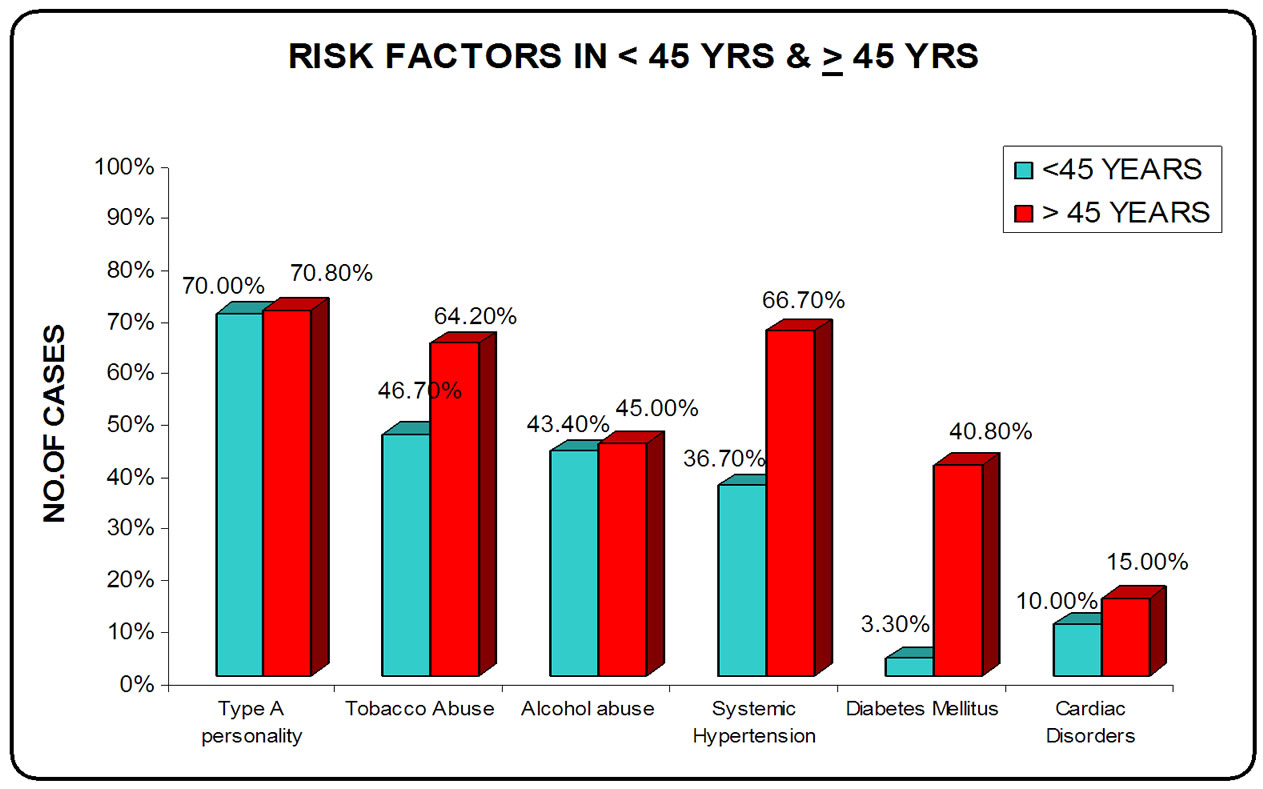
Figure 1. Risk Factors in <45 years and ≥45 years.
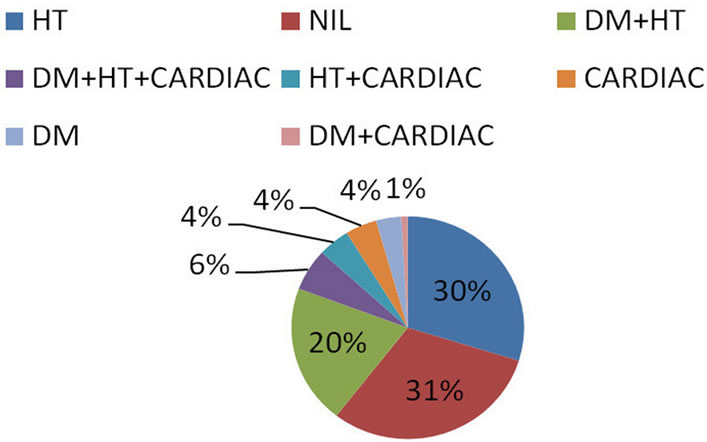
Figure 2. Cerebral infarction and comorbid medical illness.
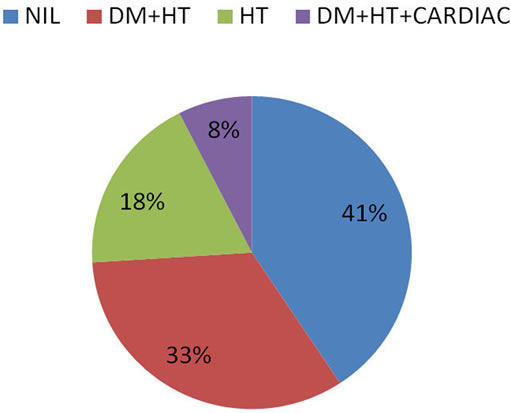
Figure 3. ICH and comorbid medical illness.
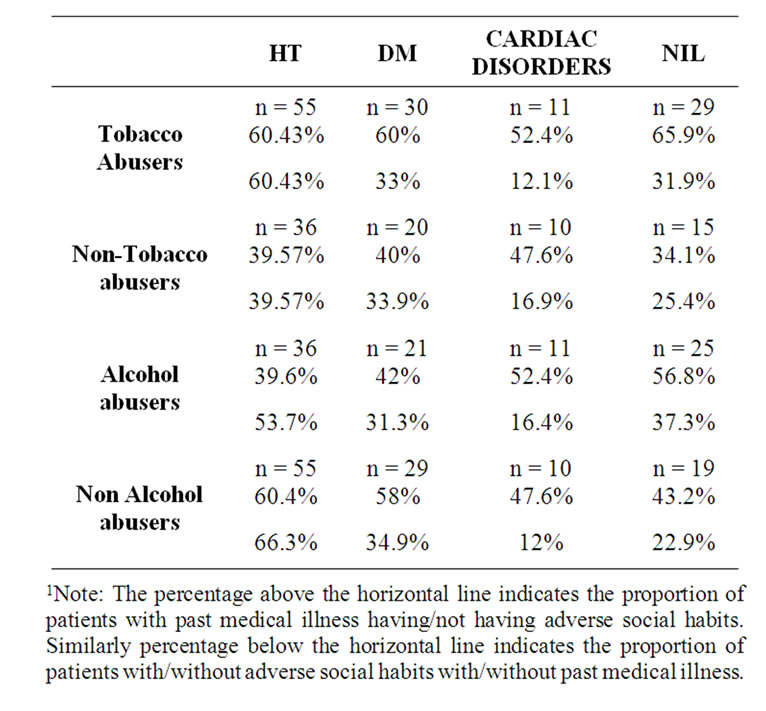
Table 2. Adverse social habits and comorbid medical illness.1
According to quadrantic model of risk of stroke, there appears to be a “J” shaped relation between alcohol intake and risk. Moderate and heavy drinking reduces and increases the risk respectively [27]. The percentage of hypertensives who were alcohol abusers (39.6%) was less than those who were not alcohol abusers (60.4%). Similar pattern was observed in diabetics. However, in cardiac patients who were alcohol abusers were more than those who were not.
As an individual risk factor, tobacco abuse increased the risk of CVA as it was seen that tobacco abusers without past medical illness were 65.9%. Similar pattern was also observed in alcohol abusers.
On exploring the risk factors, it was seen that the percentage of tobacco abusers among ≥45 years was much greater than <45 years (by 17.5%), whereas no significant difference was noted in the percentage of alcohol abusers in the two groups. The proportion of patients ≥45 years with comorbid medical illness was found to be more than the patients <45 years.
On considering the medical risk factors in young stroke patient, prior studies have revealed important contribution by cardiac disorders [28]. In this study also, following systemic hypertension, cardiac disorders was the major factor involved in the causation of stroke. Recurrent CVA was most commonly seen in <45 years (10%) [29].
To conclude, stroke in our country is very much on the rise and has accelerated the morbidity and mortality which has been evident by the data accumulated by prior studies. The occurrence of stroke steeply rises with age with its peak between 55 - 65 years. It was seen in this study also that patients ≥45 years were 80% of the stroke patients. Though stroke in the young was seen to be less common (20%) it is much more devastating, particularly with respect to productive years lost. Hence it is of paramount importance to consider it with much more greater vigour. This study showed a sex ratio with female predominance in young stroke victims with particular reference to the puerperal period. Though cerebral infarction outnumbered ICH, hemorrhage still was seen in 18% of patients. However the occurrence of ICH and cerebral infarction was equal in both age groups. Interestingly most of the patients with ICH were alcohol abusers in contrast to patient with infarcts, who were mainly tobacco abusers. This opens new avenues to explore the association between prediction of probable CVA pathology and adverse personal habits. As expected, systemic hypertension was the most common factor with significant contribution from Diabetes Mellitus. Risk factor analysis showed greater influence in ≥45 years than young strokes. On exploration of factors in young stroke victims, next to systemic hypertension, cardiac disorders proved a significant contribution. There is a need for further research in young strokes, particularly population based studies to elucidate much more intricate factors involved in its causation.
Thus a holistic approach encompassing stroke awareness, further research studies and dispensing timely management of these victims in the need of the hour to contain the tough challenge of stroke in our country which is now poised to become a giant threat in near future.
5. Acknowledgements
We acknowledge the statistical assistance given by Mr. K. Boopathi, Biostatistician, National Institute of Epidemiology, Indian Council of Medical Research, Chennai.
REFERENCES
- S. Hartona, “Experiences from a Multicenter Stroke Register: A Preliminary Report,” Bulletin of the World Health Organization, Vol. 54, No. 5, 1976, pp. 541-553.
- P. Bath, “Acute Stroke,” In: D. Machin, S. Day and S. Green, Eds., Textbook of Clinical Trials, Wiley, Hoboken, 2006, p.179-180. doi:10.1002/9780470010167.ch13
- Asian Acute Stroke Advisory Panel, “Stroke Epidemiological Data of Nine Asian Countries,” Journal of the Medical Association of Thailand, Vol. 83, 2000, pp. 1-7.
- S. K. Das, T. K. Banerjee, A. Biswas, D. K. Raut, C. S. Mukherjee, A. Chaudhari, et al., “A Prospective Community Based Study of Stroke in Kolkata, India,” Stroke, Vol. 38, No. 3, 2007, pp. 906-910. doi:10.1161/01.STR.0000258111.00319.58
- P. M. Dalal, “Burden of Stroke—Indian Perspective,” Journal of the Association of Physicians of India, Vol. 52, 2004, pp. 695-696.
- J. Abraham, P. S. S. Rao, S. G. Inbaraj, G. Shetty and C. J. Jose, “An Epidemiological Study of Hemiplegia Due to Stroke in South India,” Stroke, Vol. 1, No. 6, 1970, pp. 477-481. doi:10.1161/01.STR.1.6.477
- H. Bevan, K. Sharma and W. Bradley, “Stroke in Young Adults,” Stroke, Vol. 21, No. 3, 1990, p. 382. doi:10.1161/01.STR.21.3.382
- A. Davalos, J. Castillo, E. Martinez-Vila, et al., “Delay in Neurological Attention and Stroke Outcome,” Stroke, Vol. 26, No. 12, 1995, p. 2233.
- R. Von Kummer, P. N. Nolte, H. Schnittger, et al., “Detectability of Cerebral Hemispheric Ischemic Infarcts by CT within 6 h of Stroke,” Neuroradiology, Vol. 38, No. 1, 1996, pp. 31-33. doi:10.1007/s002340050188
- P. M. Dalal, “Burden of Stroke: Indian Perspective,” International Journal of Stroke, Vol. 1, No. 3, 2006, pp. 164- 166. doi:10.1111/j.1747-4949.2006.00051.x
- T. K. Banerjee, C. S. Mukherjee and A. Sarkhel, “Stroke in the Urban Population of Calcutta: An Epidemiological Study,” Neuroepidemiology, Vol. 20, No. 3, 2001, pp. 201- 207. doi:10.1159/000054788
- E. H. Lo, T. Dalkara and M. A. Moskowitz, “Mechanisms, Challenges and Opportunities in Stroke,” Nature Reviews Neuroscience, Vol. 4, No. 5, 2003, pp. 399-412. doi:10.1038/nrn1106
- G. Boysen, J. Nyboe, M. Appleyord, et al., “Stroke Incidence and Risk Factors for Stroke in Copenhagen, Denmark,” Stroke, Vol. 19, No. 11, 1988, p. 1345. doi:10.1161/01.STR.19.11.1345
- B. Herman, P. I. M. Schmintz, A. C. M. Leyten, et al., “Multivariate Logistic Analysis of Risk Factors for Stroke in Tilburg, Netherlands,” American Journal of Epidemiology, Vol. 118, No. 4, 1983, pp. 514-525.
- R. X. You, J. J. McNei, H. M. O’Malley, S. M. Davis, A. G. Thrift and G. A. Donan, “Risk Factors for Stroke Due to Cerebral Infarction in Young Adults,” Stroke, Vol. 28, No. 10, 1997, pp. 1913-1918. doi:10.1161/01.STR.28.10.1913
- JNC 7 Express, “The Seventh Part of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure,” US Department of Health and Human Services, National Institute of Health, Vol. 3, 2003, p. 5233.
- Expert Committee on Diagnosis and Classification of Diabetes Mellitus, “Follow-Up Report on the Diagnosis of Diabetes Mellitus,” Diabetes Care, Vol. 26, 2003, pp. 3160-3167. http://care.diabetesjournals.org/content/27suppl-1/S5.full
- P. H. Davis, J. M. Dambrosia, B. S. Shoenberg, et al., “Risk Factors for Ischemic Stroke—A Prospective Study in Rochester, Minnesota,” Annals of Neurology, Vol. 22, No. 3, 1987, pp. 319-327. doi:10.1002/ana.410220307
- R. D. Abott, B. L. Rodriguez, C. M. Burchfiel and J. D. Curb, “Physical Activity in Older Middle Aged Men and Reduced Risk of Stroke: The Honolulu Heart Program,” American Journal of Epidemiology, Vol. 139, No. 9, 1994, pp. 881-893.
- P. A. Wolf and R. B. D. Agostino, “Epidemiology of Stroke,” In: H. J. M. Barnett, J. P. Mohr, B. M. Stein and F. M. Yatsu, Eds., Stroke Pathophysiology, Diagnosis and Management, 3rd Edition, Churchill Livingstone, Edinburgh, 1988, pp. 3-28.
- P. B. Gorlick, M. B. Rodin, P. Langenberg, et al., “Weekly Alcohol Consumption, Cigarette Smoking and the Risk of Ischemic Stroke: Results of Case Control Study at Three Urban Medical Centres in Chicago, Illinosis,” Neurology, Vol. 39, No. 3, 1989, p. 339.
- R. B. Williams, “Hostility: Effect on Health and the Potential for Successful Behavioural Approaches to Prevention and Treatment,” In: A. Baum, T. A. Revenson and J. E. Singer, Eds., Handbook of health psychology, Elbraum, Mahwah, 2001.
- C. M. Burchfiel, J. D. Curb, B. L. Rodriguez, et al., “Glucose Intolerance and 22 Year Stroke Incidence—The Honolulu Heart Program,” Stroke, Vol. 25, No. 5, 1994, pp. 951-957. doi:10.1161/01.STR.25.5.951
- M. R. Goldman, E. L. Rogers and M. C. Rogers, “Subarachnoid Hemorrhage Associated with Unusual Electrocardiographic Changes,” Journal of the American Medical Association, Vol. 234, No. 9, 1975, pp. 957-958. doi:10.1001/jama.1975.03260220061023
- M. R. Pandey, “Tobacco Smoking and Hypertension,” The Journal of the Indian Medical Association, Vol. 97, No. 9, 1999, pp. 367-369.
- U. Keil, A. Liese, B. Filipiak, et al., “Alcohol, Blood Pressure and Hypertension,” Novartis Foundation Symposium, Vol. 216, 1998, p. 125.
- R. L. Sacco, M. El Kind, B. Boden-Albala, et al., “The Protective Effect of Moderate Alcohol Consumption on Ischemic Stroke,” Journal of the American Medical Association, Vol. 281, No. 1, 1999, pp. 53-60. doi:10.1001/jama.281.1.53
- A. Caroli, C. Marini, E. Ferranti, et al., “A Prospective Study of Cerebral Ischemia in the Young. Analysis of Pathogenic Determinants,” Stroke, Vol. 24, No. 3, 1993, pp. 362-367. doi:10.1161/01.STR.24.3.362
- “Copenhagen Stroke Study: Stroke Recurrence, Predictors, Severity and Prognosis, Neurology,” 1997. http/www.neurology.org/content/48/4/891.short

