Open Journal of Nephrology
Vol.4 No.1(2014), Article ID:44089,9 pages DOI:10.4236/ojneph.2014.41005
Physician’s Awareness of Home Blood Pressure in the Treatment of Hypertensive Patients with Chronic Kidney Disease
Naoki Sugano, Satoru Kuriyama*, Yoichiro Hara, Koki Takane, Yasuhito Takahashi, Yasuko Suetsugu, Takashi Yokoo
Division of Kidney and Hypertension, Department of Internal Medicine, The Jikei University School of Medicine, Tokyo, Japan
Email: *kuriyamas218@yahoo.co.jp
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 20 December 2013; revised 19 January 2014; accepted 16 February 2014
ABSTRACT
Aim: The majority of guidelines recommended the significance of home-based blood pressure (home-BP) measurement. The present study explored that to what extent, general practitioners (GPs) were aware of the importance of home-BP in the daily clinical practice. Method: We sent out questionnaires to GPs who had been specialized in nephrology and hypertension. The questions focused on the awareness of home-BP and the selections of antihypertensive agents for refractory hypertension in chronic kidney disease (CKD) patients. Results: 1) The majority (95.9%) of the responding GPs had utilized home-BP in their clinical practice. 2) When prescribing a single agent for hypertensive CKD patients, the majority of GPs (87.3%) chose ARB for the first line drug, and Ca channel blockers (CCB) were the second. 3) As an add-on drug to the pre-treatment with an angiotensin receptor blocker (ARB), the majority preferred CCB (82.7%) to diuretics (21.8%). In addition, a fixed combination formula of antihypertensive medication consisting of ARB plus diuretic was accepted by the majority of GPs (78.7%). 4) To improve morning hypertension in patients treated with two or more drugs, 87.8% of the doctors agreed that additional night-time dosing could be useful. The choices of the agents given at night-time varied, mainly with α1- blockers (40.6%), followed by α-blockers (30.5%) and α-methyldopa (19.8%). Conclusion: The majority of GPs in Japan are aware of the importance of the home-BP-based management of CKD. They mainly chose ARB as a first line drug, and ARB plus CCB as an add-on therapy.
Keywords:Home Blood Pressure; Chronic Kidney Disease; Guideline for High Blood Pressure; Antihypertensive Agents

1. Introduction
Three different methods of BP measurement are office BP, home-BP measured at any given time of the day (home-BP) and 24-hours ambulatory BP (ABP) monitoring. The two latter methods are home-based BP, which give lots of advantages including; 1) it provides multiple measurement of BP in any occasion by days, weeks, months or years; 2) it is obtained in a usual environment for each individual which can avoid white-coat effect; 3) it can detect the white-coat, masked and morning hypertension; and 4) it is closely related to target organ damage and predicts the risk of cardiovascular events.
In cross-sectional studies, ABP values are correlated with the organ damage accompanying hypertension and diabetes mellitus more closely than office BP values [1] -[4] . Similarly, in longitudinal studies, BP values of home-based BP predict the progression of organ damage and the risk of cardiovascular disease more accurately than office BP [5] -[10] . Unquestionably, these data support the notion that home-based BP is a highly valuable tool in the management of hypertension [11] -[15] . Despite very few head-to-head comparisons between homeBP and ABP, the results constantly showed that both were equally reliable in predicting the target-organ damage in hypertensive patients [16] -[19] .
However, clinical indications for these home-based BP are substantially different. Compared with ABP, home-BP provides measurement over a much longer period of time, and is cheaper, more widely available, thus more convenient and acceptable for patients [4] [20] -[22] . Based on the European Society of Hypertension/Cardiology recommendations, ABP is advantageous if there is a considerable variability in the clinic BP of the patients’ regular visits, and if there is a marked discrepancy between home-BP and office BP. On the other hand, home-BP provides more information on the antihypertensive effect of the treatment by comparing the trough and the peak BP values [22] -[25] . Recently, after several years being exposed to the guidelines published by the Japanese Society of Hypertension, the GPs’ recognition and awareness of home-BP-based clinical practice has been surveyed in Japan [26] [27] . These studies showed a high awareness of home-BP among GPs, though they are still confused with how to apply it for patients.
On achieving adequate BP goals, lots of studies showed that more than one antihypertensive agent was needed to reach the target goal [28] . Like many other countries such as the US and Europe [29] , Japan has witnessed a substantial influx of fixed formulation tablet of combination medicines consisting of ARB plus diuretic or ARB plus CCB. As a result, in the past several years, several different analogous fixed formulations of two antihypertensive agents combined have come into use. As a result of this trend, some GPs are not sure about how to use and choose these fixed formulation tablets, and others are even perplexed about how to use them.
In this communication, we investigated that to what extent GPs are aware of the importance of home-BP in the clinical practice of CKD as well as their decisions in choosing the antihypertensive drugs. In order to pursue this objective, GPs were asked via questionnaires about the awareness of home-BP, how to prescribe multiple antihypertensive drugs for morning hypertension. The present study is the first to highlight the awareness of home-BP among GPs who are specialized in CKD practice, especially in Japan.
2. Materials and Methods
Materials: During the period between October 2009 and March 2011, we distributed and collected questionnaires to 330 doctors in Tokyo and its vicinity, All participants were general practitioners (GPs) belonging to the department of medicine of the medical universities specialized in nephrology and hypertension. Approximately 80% or more of them had taken educational programs in nephrology and hypertension while they were in the post doctoral training courses, approximately 20% of them were qualified specialists approved by the Japanese society of Nephrology and/or Hypertension. There were some GPs who had their own clinics, not always but often treating CKD patients.
Methods: They were asked about hypertension treatment on the assumption that they had encountered hypertensive CKD patients at their clinics. The questionnaires were on an anonymous basis, and the GPs were requested to answer them with reference to the High Blood Pressure Guideline either by the Japanese Society of Hypertension [30] , the 7th Report of the Joint National Committee in the U.S. [31] , or the European Society of Hypertension/Cardiology Recommendations [24] . Because of its study protocol using questionnaires in which individual patient’s information was no longer revealed, ethical consideration with respect to patient’s right was apparently not violated. The questions to the GPs mainly focused on the awareness of home-BP measurement, the expected target BP levels by home-BP (135/85 mmHg), how to select antihypertensive medications, how to prescribe antihypertensive agents, when to measure home-BP and so on. We also asked specifically about the importance of morning BP, how to choose antihypertensive agents including fixed formula of antihypertensive agents; what time is appropriate to take those agents, and then finally to what extent they were aware of the risk factors for hypertension. Questionnaires were delivered, collected and analyzed within a few months. The completion rate of the data available for analyses was 60%.
3. Results
Figure 1 shows that almost all of the GPs (95.9%) utilized home-BP in their daily clinical practice. Nearly three quarter (76.1%) of them answered that home-BP is valuable and that it should be more effectively utilized in clinical practice. In addition, morning BP (39.1%) was regarded as being more important than night time BP (0.5%), and 58.8% answered that both morning and night time home-BP were equally important in the treatment of hypertension.
Figure 2 shows the degree of recognition as to what extent the guideline-recommended definition of hypertension at home (more than 135/85mmHg) was accepted by the GPs. The majority of them approved of the home-BP goal value (86.3%). However, the majority (88.3%) believed that this criterion of home-BP had not yet been scientifically proven, and that more evidence would be needed to scientifically confirm this goal.
Figure 3 depicts the result of the recognition of the progression factors of CKD. They were asked which factors have a strong impact on CKD progression. Hypertension, hyperglycemia, high dietary protein intake, hyperlipidemia, hyperuricemia, anemia were chosen in this order as such factors.
Figure 4 depicts the choice of the antihypertensive agents for CKD when asked to carry out either monotherapy (the upper graph) or dual therapy (the lower graph). More than 80% of the GPs chose an angiotensin type 1 receptor blocker (ARB) as their first choice of medication for hypertensive CKD patients. In contrast, less than 10% chose ACE-I and/or CCB as a first line drug. As to the doctor’s preferences for their second choice of an add-on drug to ARB or ACE-I, more than 80% GPs chose CCB as a second line antihypertensive medication. In contrast, less than 20% chose diuretics as a second choice.
Figure 5 shows the responses to the questions about morning hypertension. Almost all of them (99.0%) answered that morning hypertension is a strong risk for cardiovascular diseases, and that control is crucial to achieve better outcomes. For the purpose of reducing the risk of morning hypertension, 87.8% of them agreed that the night time dosing with an additional antihypertensive agent could be effective in lowering morning events. As for the agents to ameliorate morning hypertension, 42.1% of the GPs chose 1-blocker, followed by ARB (27.0%), CCB (15.1%), β-blocker (6.9%) and ACE-I (4.4%).
Figure 6 (upper circle) depicts how to prescribe two drugs when a dual therapy was needed. The responses to this question were diverse. If the two drugs were to be given separately, 46.2% of them would prescribe either ARB or ACE-I at night and CCB or diuretics in the morning. However, 29.9% answered that both ARB/ACE-I and CCB/diuretics should be taken together in the morning.
Figure 6 (lower left circle) describes that 78.7% admitted that a fixed formulation of single tablet with ARB plus diuretic is useful and necessary for their daily clinical practice. Finally, as a third choice for refractory morning hypertension (lower right circle), the majority of the GPs chose α1-blocker (40.6%), followed by α-blocker (30.5%) and α-, plus β-blocker (19.8%).
4. Discussion
We conducted a survey on home-BP among GPs who were specialized in the treatment of CKD in Japan. The use of home-based BP has been recommended in many high blood pressure guidelines. Such guidelines suggested that home-based BP is indicative to all of the patients treated with antihypertensive medications [4] [20] -[22] . As a result of the recently-published hypertension guidelines as well as the penetration of BP measuring device at home, its use has been constantly increased all over the world, and so does in Japan. Compared with ABP which requires 24 monitoring which sometimes bothers patients, home-BP may be more suitable for daily management in the most of hypertensive patients [23] -[25] .
First, we were able to confirm a high awareness of home-BP among GPs who deal with hypertensive CKD patients (Figures 1 and 2). In addition, the notion that ARB as a first line drug and CCB as an add-on drug was approved by the majority of GPs in Japan (Figure 4). Undisputedly, a lot of evidence has confirmed the organ-protective effect of RAS inhibitors, ARB and/or ACE-I. Influenced by these evidences, the majority of GPs
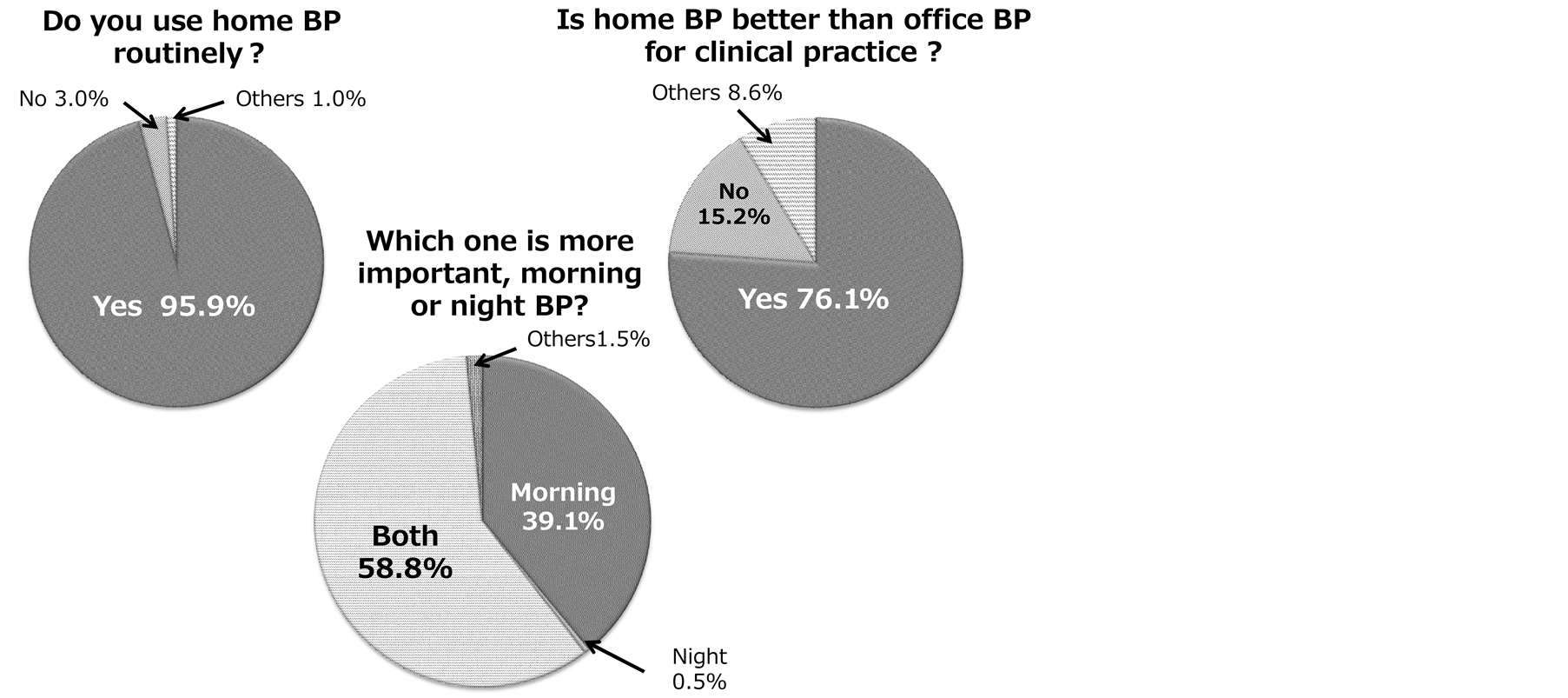
Figure 1. Awareness on the use of home-BP.
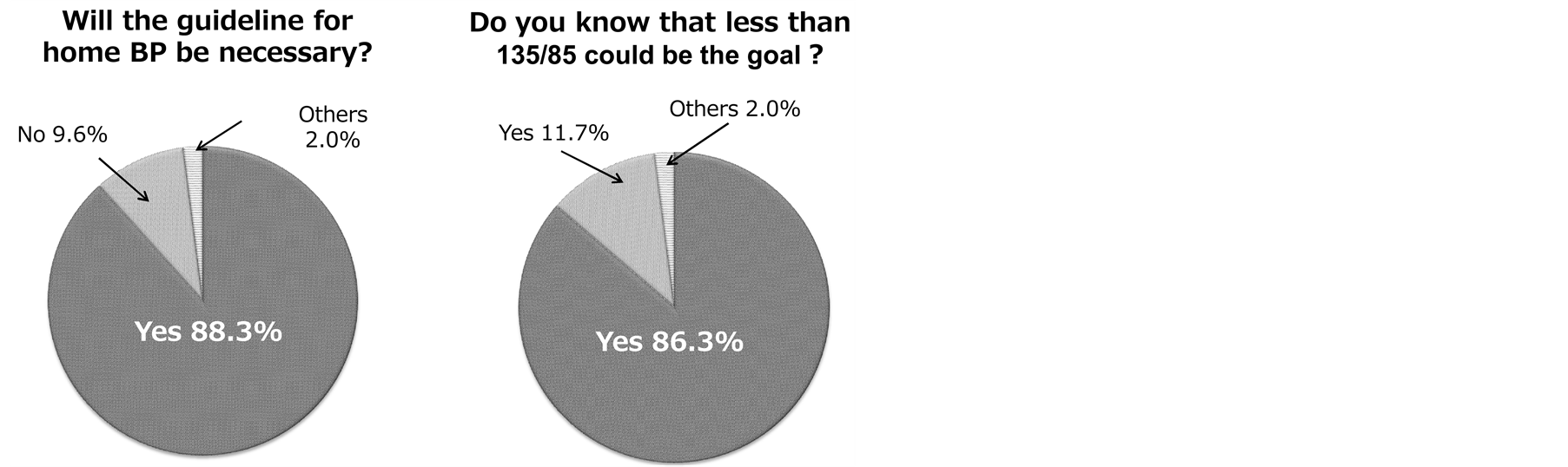
Figure 2. Treatment goal for home-BP. The Japanese Society Hypertension (JSH) guideline recommended 135/85 mmHg as the treatment goal of home-BP.
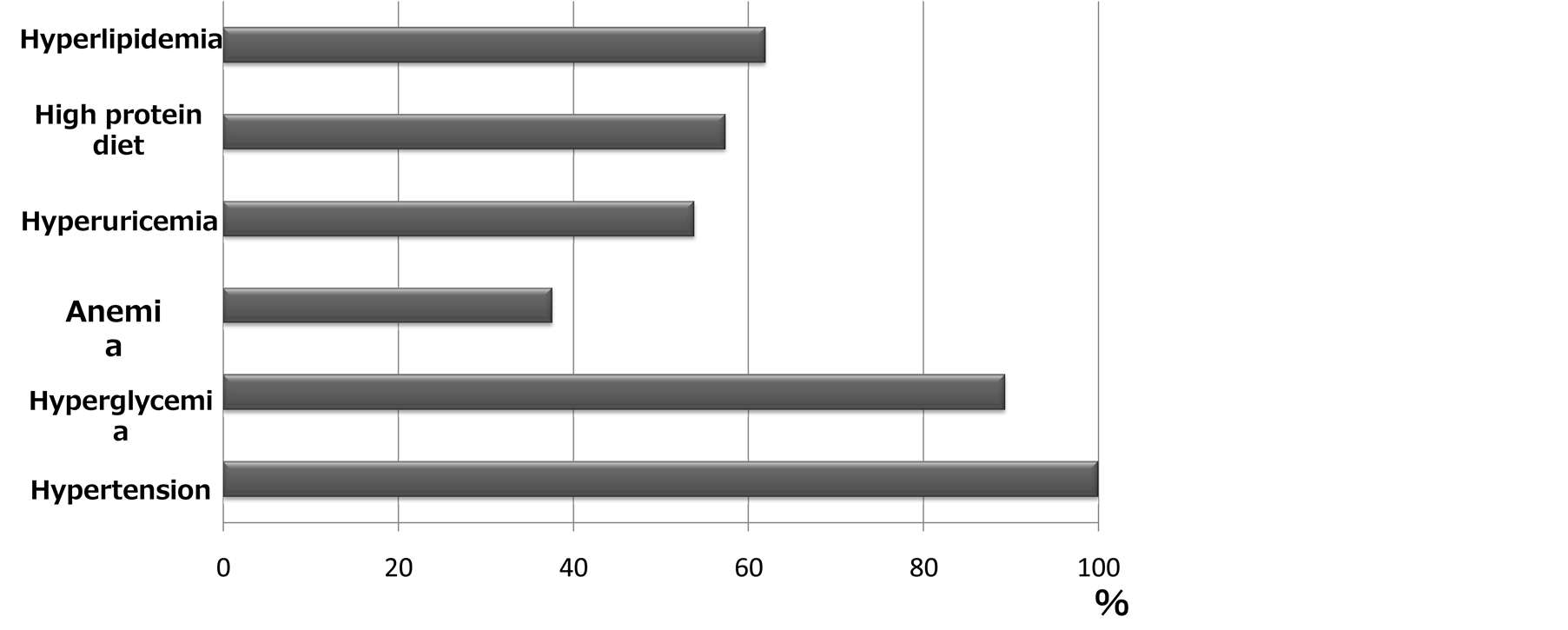
Figure 3.Questions on the progression factors for CKD.
have accepted that ARB or ACE-I must be the first-choice agent in patients with CKD.
As to the refractory hypertension which normally needs more than two antihypertensive drugs, the majority of GPs answered that the second choice should be CCB, instead of diuretic. It means that they were reluctant to se
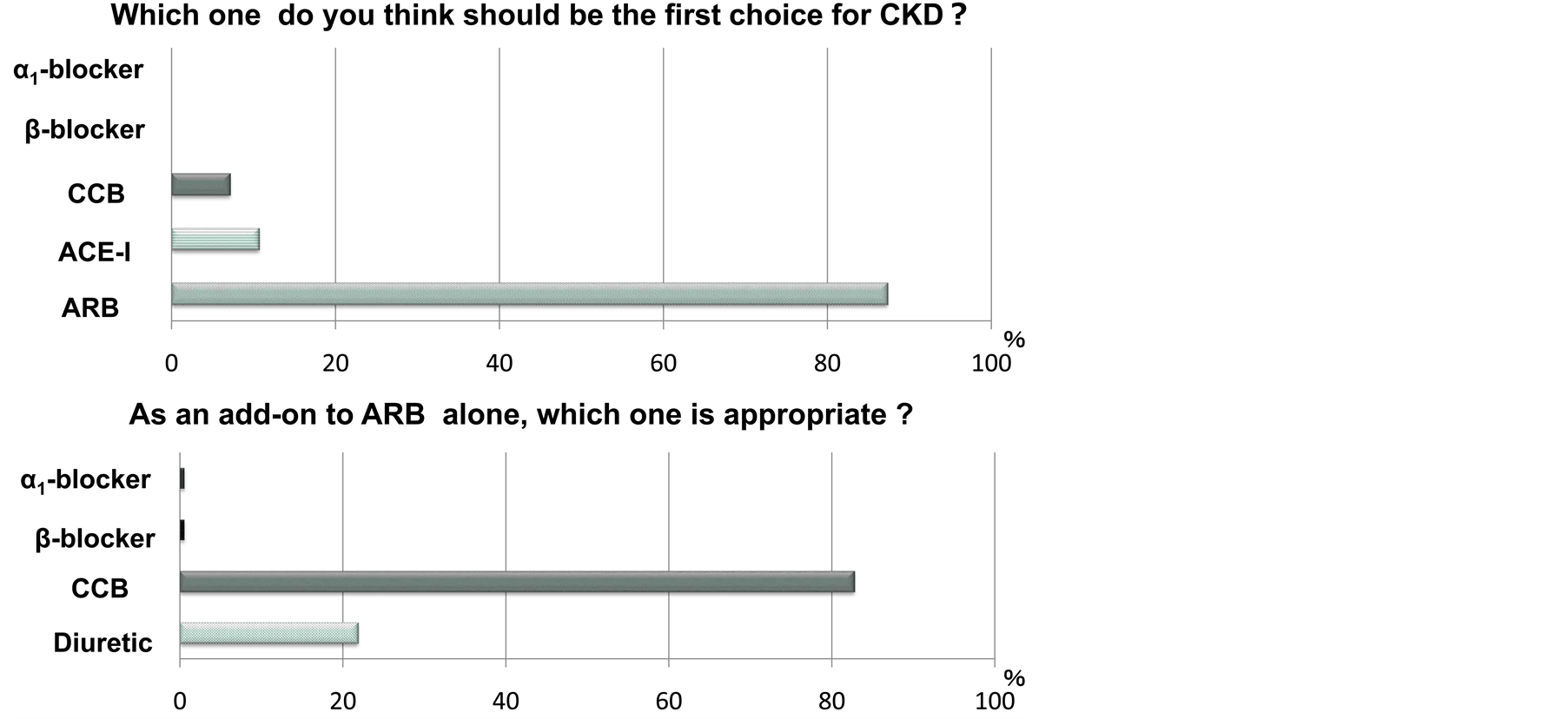
Figure 4.Choices of the antihypertensive agents for CKD.
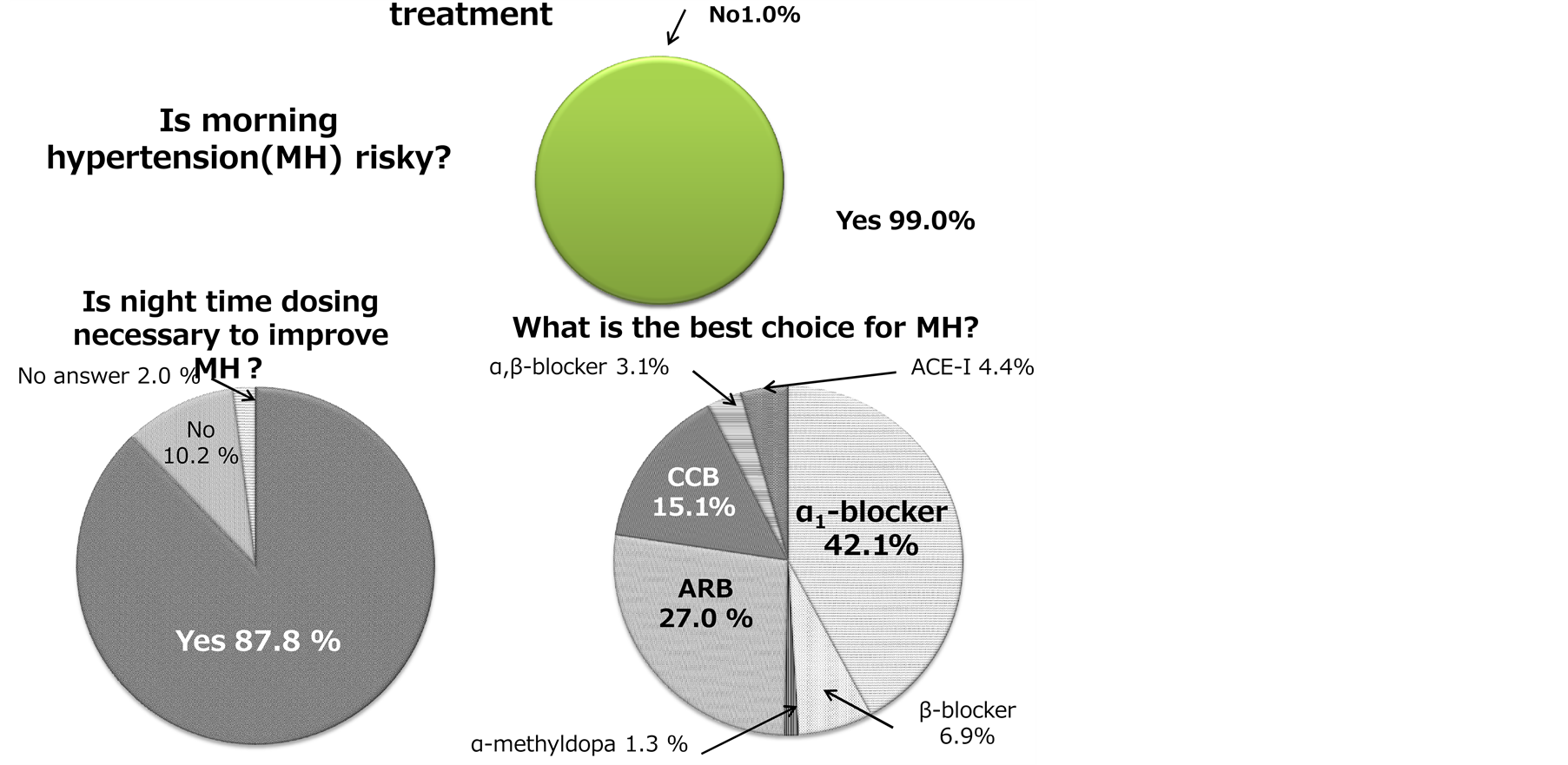
Figure 5.Morning hypertension and the treatment.
lect diuretics even as a second choice. This is surprising to us because before commencing this study, we had anticipated that the majority of GPs would choose diuretic-ridden regimen, as many fixed formulations of combined ARB with diuretics had been on the market for the past few years in Japan. Yet in reality, diuretics were thought to be inferior to CCB [32] . What’s behind this? We assume that the GPs believed that CCB is more potent to lower BP than diuretic, and safer with less metabolic adverse effects such as impaired glucose tolerance, hyperlipidemia, hypokalemia and hyperuricemia that diuretics frequently induce [31] .
Alleviating morning hypertension was accepted by nearly 90% of the GPs. As CKD progresses into more advanced stage, incidence of morning hypertension increases. In order to reduce the risk of morning hypertension, in addition to the foregoing combination therapy with ARB plus CCB or diuretic for example, night time dosing with a third choice drug could be indispensable. An appropriate chronotherapy in hypertensive patients which concerns administration-time provides a means of accomplishing this purpose. There are several possible agents to ameliorate morning hypertension. Night time dosing with the CCB, α1-blocker, β-blocker, ACE-I and ARB has been proven to be effective [33] -[37] . Among them, α1-blockers appeared to be rational as they have a substantial effect on morning hypertension. Kario et al. addressed whether the night time dosing of α1-blocker alle-
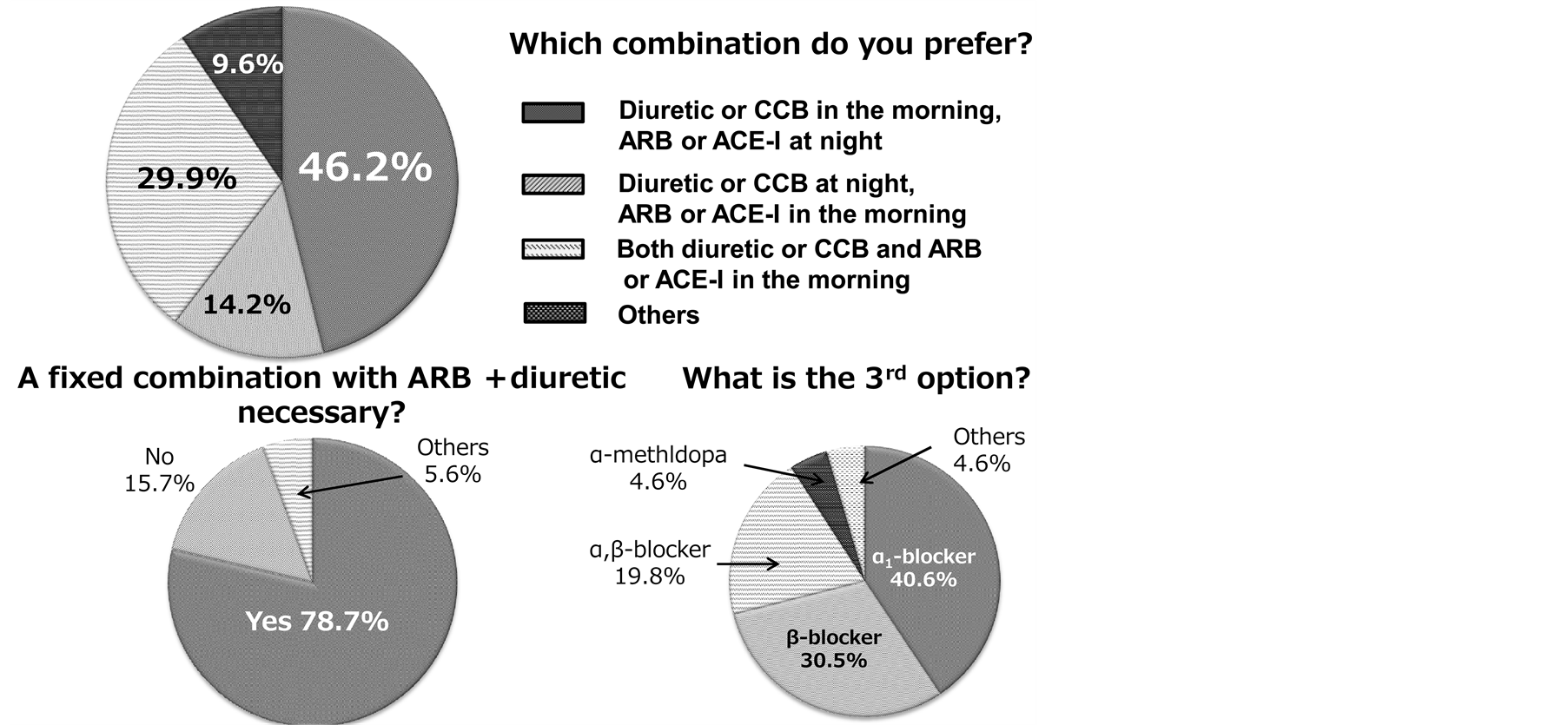
Figure 6. Combined therapies with two drugs and a need for a fixed formulation tablet.
viates morning hypertension in patients with hypertension, and found that this agent efficaciously improved morning hypertension [33] [35] .
The administration timing of the two drugs if the patients would require dual treatment was quite diverse (Figure 6). Administration of a diuretic or CCB in the morning with ARB or ACE-I at night came as the first preference (46.2%). The second preference was an administration of both diuretic or CCB and ARB or ACE-I together in the morning (29.9%). The third preference was an administration of diuretic or CCB at night and ARB or ACE-I in the morning (14.2%). When asked if there was a need to prescribe a fixed formulation with ARB plus diuretic, the majority replied in an affirmative way (78.7%). It implies that a fixed formulation tablet could be prescribed for at least 1/3 of the patients who would be treated with more than two drugs.
To summarize, this present study confirms that the majority of doctors in Japan accepted that home-BP is important. Since little is known about the diagnostic, prognostic and therapeutic values of home-BP, there is an urgent need for clinical studies on how to use home-BP in terms of improving long-term patients’ prognostic outcomes.
5. Conclusion
The doctors in clinical practice of CKD in Japan have a high awareness of the importance of home-BP, though choices of antihypertensive agents remain diverse. Since little has been established regarding how to integrate home-BP into clinical practices, it appears imperatively to proceed with further clinical investigations in this field.
Conflict of Interest
No conflict of interest is declared.
References
- Jula, A., Puukka, P. and Karanko, H. (1999) Multiple Clinic and Home Blood Pressure Measurements versus Ambulatory Blood Pressure Monitoring. Hypertension, 34, 261-266. http://dx.doi.org/10.1161/01.HYP.34.2.261
- Mancia, G., Parati, G., Hennig, M., Flatau, B., Omboni, S., Glavina, F., Costa, B., Scherz, R., Bond, G. and Zanchetti, A. (2001) For the ELSA Investigators. Relationship between Blood Pressure Variability and Carotid Artery Damage in Hypertension: Baseline Data from the European Lacidipine Study on Atherosclerosis (ELSA). Journal of Hypertension, 19, 1981-1989. http://dx.doi.org/10.1097/00004872-200111000-00008
- Mancia, G. and Parati, G. (2000) Ambulatory Blood Pressure Monitoring and Organ Damage. Hypertension, 36, 894- 900. http://dx.doi.org/10.1161/01.HYP.36.5.894
- Mancia, G., Zanchetti, A., Agabiti-Rosei, E., Benemio, G., De Cesaris, R., Fogari, R., Pessina, A., Porcellati, C., Rappelli, A., Salvetti, A. and Trimarco, B. (1997) Ambulatory Blood Pressure Is Superior to Clinic Blood Pressure in Predicting Treatment Reduced Regression of Left Ventricular Hypertrophy. Circulation, 95, 1464-1470. http://dx.doi.org/10.1161/01.CIR.95.6.1464
- Khattar, R.S., Swales, J.D., Banfield, A., Dore, C., Senior, R. and Lahiri, A. (1999) Prediction of Coronary and Cerebrovascular Morbidity Blood Pressure Monitoring in Essential Hypertension. Circulation, 100, 1071-1076. http://dx.doi.org/10.1161/01.CIR.100.10.1071
- Lurbe, E., Redon, J., Kesani, A., Pascual, J.M., Tacons, J., Alvarez, V. and Batlle, D. (2002) Increase in Nocturnal Blood Pressure and Progression to Microalbuminuria in Type I Diabetes. The New England Journal of Medicine, 347, 797-805. http://dx.doi.org/10.1056/NEJMoa013410
- Perloff, D., Sokolow, M. and Cowan, R. (1983) The Prognostic Value of Ambulatory Bloodpressures. JAMA, 249, 2793-2798. http://dx.doi.org/10.1001/jama.1983.03330440030027
- Redon, J., Campos, C., Narciso, M.L., Rodicio, J.L., Pascual, J.M. and Ruilope, L.M. (1998) Prognostic Value of Ambulatory Blood Pressure Monitoring in Refractory Hypertension: A Prospective Study. Hypertension, 31, 712-718. http://dx.doi.org/10.1161/01.HYP.31.2.712
- Robinson, T.G., Dawson, S.L., Ahmed, U., Manktelow, B., Fotherby, M.D. and Potter, J.F. (2001) Twenty-Four Hour Systolic Blood Pressure Predicts Long-Term Mortality Following Acute Stroke. Journal of Hypertension, 19, 2127- 2134. http://dx.doi.org/10.1097/00004872-200112000-00003
- Staessen, J.A., Thijs, L., Fagard, R., O’Brien, E.T., Clement, D., de Leeuw, P.W., Mancia, G., Nachev, C., Palatini, P., Parati, G., Tuomilehto, J. and Webster, J. (1999) Predicting Cardiovascular Risk Using Conventional vs Ambulatory Blood Pressure in Older Patients with Systolic Hypertension: Systolic Hypertension in Europe Trial Investigators. JAMA, 282, 539-546. http://dx.doi.org/10.1001/jama.282.6.539
- Bjorklund, K., Lind, L., Zethelius, B., Andren, B. and Lithell, H. (2003) Isolated Ambulatory hypertension Predicts Cardiovascular Morbidity in Elderly Men. Circulation, 107, 1297-1302. http://dx.doi.org/10.1161/01.CIR.0000054622.45012.12
- Clement, D.L., De Buyzere, M.L., De Bacquer, D.A., de Leeuw, P.W., Duprez, D.A., Fagard, R.H., Gheeraert, P.J., Missault, L.H., Braun, J.J., Six, R.O., Van Der Niepen, P. and O’Brien, E. (2003) For the Office Versus Ambulatory Pressure Study Investigators. Prognostic Value of Ambulatory Blood Pressure in Patients with Treated Hypertension. The New England Journal of Medicine, 348, 2407-2415. http://dx.doi.org/10.1056/NEJMoa022273
- Verdecchia, P., Reboldi, G., Porcellati, C., Schillaci, G., Pede, S., Bentivoglio, M., Angeli, F., Norgiolini, S. and Ambrosio, G. (2002) Risk of Cardiovascular Disease in Relation to Achieved Office and Ambulatory Blood Pressure Control in Treated Hypertensive Subjects. Journal of the American College of Cardiology, 39, 878-885. http://dx.doi.org/10.1016/S0735-1097(01)01827-7
- Yamamoto, Y., Akiguchi, I., Oiwa, K., Hayashi, M. and Kimura, J. (1998) Adverse Effect of Nighttime Blood Pressure on the Outcome of Lacunar Infarct Patients. Stroke, 29, 570-576. http://dx.doi.org/10.1161/01.STR.29.3.570
- Zweiker, R., Eber, B., Schumacher, M., Toplak, H. and Klein, W. (1994) “Non-Dipping” Related to Cardiovascular Events in Essential Hypertensive Patients. Acta Medica Austriaca, 21, 86-89.
- Bobrie, G., Chatellier, G., Genes, N., Clerson, P., Vaur, L., Vaisse, B., Menard, J. and Mallion, J.M. (2004) Cardiovascular Prognosis of “Masked Hypertension” Detected by Blood Pressure Self-Measurement in Elderly Treated Hypertensive Patients. JAMA, 291, 1342-1349. http://dx.doi.org/10.1001/jama.291.11.1342
- Kario, K., Pickering, T.G., Matsuo, T., Hoshide, S., Schwartz, J.E. and Shimada, K. (2001) Stroke Prognosis and Abnormal Nocturnal Blood Pressure Falls in Older Hypertensives. Hypertension, 38, 852-857. http://dx.doi.org/10.1161/hy1001.092640
- Sega, R., Facchetti, R., Bombelli, M., Cesana, G., Corrao, G., Grassi, G. and Mancia, G. (2005) Prognostic Value of Ambulatory and Home Blood Pressures Compared with Office Blood Pressure in General Population. Circulation, 111, 1777-1783. http://dx.doi.org/10.1161/01.CIR.0000160923.04524.5B
- Verdecchia, P., Porcellati, C., Schillaci, G., Borgioni, C., Ciucci, A., Battistelli, M., Guerrieri, M., Gatteschi, C., Zampi, I. and Santucci, A. (1994) Ambulatory Blood Pressure: An Independent Predictor of Prognosis in Essential Hypertension. Hypertension, 24, 793-801. http://dx.doi.org/10.1161/01.HYP.24.6.793
- Martinez, M.A., Sancho, T., Garcia, P., Moreno, P., Rubio, J.M., Palau, F.J., Anton, J.L., Cirujano, F.J., Sanz, J., Puig, J.G. and MAPA Working Group (2006) Home Blood Pressure in Poorly Controlled Hypertension: Relationship with Ambulatory Blood Pressure and Organ Damage. Blood Pressure Monitoring, 11, 207-213. http://dx.doi.org/10.1097/01.mbp.0000209073.30708.e1
- Mule, G., Caimi, G., Cottone, S., Nardi, E., Andronico, G., Piazza, G., Volpe, V., Federico, M.R. and Cerasola, G. (2002) Value of Home Blood Pressures as Predictor of Target Organ Damage in Mild Arterial Hypertension. Journal of Cardiovascular Risk, 9, 123-129. http://dx.doi.org/10.1097/00043798-200204000-00008
- Stergiou, G.S., Argyraki, K.K., Moyssakis, I., Mastorantonakis, S.E., Achimastos, A.D., Karamanos, V.G. and Roussias, L.G. (2007) Home Blood Pressure Is as Reliable as Ambulatory Blood Pressure in Predicting Target-Organ Damage in Hypertension. American Journal of Hypertension, 20, 616-621. http://dx.doi.org/10.1016/j.amjhyper.2006.12.013
- Mancia, G., De Backer, G., Dominiczak, A., Cifkova, R., Fagard, R., Germano, G., Grassi, G., Heagerty, A.M., Kjeldsen, S.E., Laurent, S., Narkiewicz, K., Ruilope, L., Rynkiewicz, A., Schmieder, R.E., Boudier, H.A. and Zanchetti, A. (2007) Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Journal of Hypertension, 25, 1105-1187. http://dx.doi.org/10.1097/HJH.0b013e3281fc975a
- Parati, G., Stergiou, G.S., Asmar, R., Bilo G, de Leeuw, P., Imai, Y., Kario, K., Lurbe, E., Manolis, A., Mengden, T., O’Brien, E., Ohkubo, T., Padfield, P., Palatini, P., Pickering, T.G., Redon, J., Revera, M., Ruilope, L.M., Shennan, A., Staessen, J.A., Tisler, A., Waeber, B., Zanchetti, A., Mancia, G. and On Behalf of ESH Working Group on Blood Pressure Monitoring (2010) European Society of Hypertension Practice Guidelines for Home Blood Pressure Monitoring. Journal of Human Hypertension, 24, 779-785. http://dx.doi.org/10.1038/jhh.2010.54
- Verdecchia, P., Angeli, F., Mazzatta, G., Gentile, G. and Reboldi, G. (2009) Home Blood Pressure Measurement Will Not Replace 24-Hour Ambulatory Blood Pressure Monitoring. Hypertension, 54, 188-195. http://dx.doi.org/10.1161/HYPERTENSIONAHA.108.122861
- Kobayashi, M., Obara, T., Ohkubo, T., Fukunaga, H., Satoh, M., Metoki, H., Asayama, K., Inoue, R., Kikuya, M., Mano, N., Miyakawa, M. and Imai, Y. (2010) Practice and Awareness of Physicians Regarding Casual-Clinic Blood Pressure Measurement in Japan. Hypertension Research, 33, 960-964. http://dx.doi.org/10.1038/hr.2010.89
- Obara, T., Ohkubo, T., Fukunaga, H., Kobayashi, M., Satoh, M., Metoki, H., Asayama, K., Inoue, R., Kikuya, M., Mano, N., Miyakawa, M. and Imai, Y. (2010) Practice and Awareness of Physicians Regarding Home Blood Pressure Measurement in Japan. Hypertension Research, 33, 428-434. http://dx.doi.org/10.1038/hr.2010.10
- Elliot, W.J. (2002) Is Fixed Combination Therapy Appropriate for Initial Hypertension Treatment? Current Hypertension Reports, 4, 278-285. http://dx.doi.org/10.1007/s11906-996-0005-z
- Black, H.R. (2009) Triple Fixed-Dose Combination Therapy. Hypertension, 54, 19-22. http://dx.doi.org/10.1161/HYPERTENSIONAHA.109.132688
- Ogihara, T., Kikuchi, K., Matsuoka, H., Fujita, T., Higaki, J., Horiuchi, M., Imai, Y., Imaizumi, T., Ito, S., Iwao, H., Kario, K., Kawano, Y., Kim-Mitsuyama, S., Kimura, G., Matsubara, H., Matsuura, H., Naruse, M., Saito, I., Shimada, K., Shimamoto, K., Suzuki, H., Takishita, S., Tanahashi, N., Tsuchihashi, T., Uchiyama, M., Ueda, S., Ueshima, H., Umemura, S., Ishimitsu, T., Rakugi, H. and Japanese Society of Hypertension Committee. (2009) The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertension Research, 32, 103-107.
- Chobanian, A.V., Bakris, G.L., Black, H.R., Cushman, W.C., Green, L.A., Izzo Jr., J.L., Jones, D.W., Materson, B.J., Oparil, S., Wright Jr., J.T., Roccella, E.J. and Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (2003) National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension, 42, 1206-1252. http://dx.doi.org/10.1161/01.HYP.0000107251.49515.c2
- Kohro, T., Yamazaki, T., Sato, H., Ohe, K. and Nagai, R. (2013) The Impact of a Change in Hypertension Management Guidelines on Diuretic Use in Japan: Trend in Antihypertensive Drug Prescriptions from 2005 to 2011. Hypertension Research, 36, 559-563. http://dx.doi.org/10.1038/hr.2012.216
- Kario, K., Pickering, T.G., Hoshide, S., Eguchi, K., Ishikawa, J., Morinari, M., Hoshide, Y. and Shimada, K. (2004) Morning Blood Pressure Surge and Hypertensive Cerebrovascular Disease. American Journal of Hypertension, 17, 668-675. http://dx.doi.org/10.1016/j.amjhyper.2004.04.001
- Kario, K., Schwartz, J.E. and Pickering, T.G. (2000) Changes of Nocturnal Blood Pressure Dipping Status in Hypertensives by Nighttime Dosing of α-Adrenergic Blocker, Doxazosin. Result from HALT Study. Hypertension, 35, 787- 794. http://dx.doi.org/10.1161/01.HYP.35.3.787
- Hermida, R.C., Ayala, D.E., Fernamdez, J.R. and Calvo, C. (2007) Comparison of the Efficacy of Morning versus Evening Administration of Telmisartan in Essential Hypertension. Hypertension, 50, 715-722. http://dx.doi.org/10.1161/HYPERTENSIONAHA.107.094235
- Hermida, R.C., Ayala, D.E., Smolensky, M.H. and Portaluppi, F. (2007) Chronotherapy in Hypertensive Patients: Administration Time Dependent Effects of Treatment on Blood Pressure Regulation. Expert Review of Cardiovascular Therapy, 5, 463-475. http://dx.doi.org/10.1586/14779072.5.3.463
- Hermida, R.C. and Ayala, D.E. (2009) Chronotherapy with the Angiotensin-Converting Enzyme Inhibitor Ramipril in Essential Hypertension: Improved Blood Pressure Control with Bedtime Dosing. Hypertension, 54, 40-46. http://dx.doi.org/10.1161/HYPERTENSIONAHA.109.130203
NOTES

*Corresponding author.

