Open Journal of Medical Imaging
Vol.4 No.2(2014), Article
ID:46876,6
pages
DOI:10.4236/ojmi.2014.42011
Clinical and Radiological Localization of Language Dysfunctions in Acute Ischemic Stroke
Amira Ahmed Zaki Dwidar, Taha Kamel Alloush, Mahmoud Youssef Abou El-Ella, Nahed Salah El-Din Ahmed, Karima Moustafa Maher, Maha Ali Mohamed Nada, Mohamed Hamdy Ibrahim
Faculty of Medicine, Ain Shams University, Cairo, Egypt
Email: mohamedhamdy_neuro2007@yahoo.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 13 April 2014; revised 23 May 2014; accepted 30 May 2014
ABSTRACT
Objective: To study the effect of cerebral ischemic vascular insult on the localization of language areas as regard to automatic speech, initiation, and mutism. Materials and Methods: Seventy ischemic stroke patients were selected within the first 48 h of the onset of stroke with left hemispheric stroke with aphasia. Inclusion criteria: any age above seven years, both sexes, first ever clinical stroke, admitted within the first 2 days of stroke insult. Patients underwent careful history taking, neurological examination, routine laboratory investigations, echo cardiography, and carotid duplex and language assessments. Results: Automatic speech disorders were mainly seen along left insular, left supramarginal and left frontal inferior orbital lesions. Initiation difficulty is seen mainly along as left insular, left temporal superior and left periventricular lesions. Mutism is seen along left external capsule, left internal capsule, left pallidum, left frontal inferior orbital and left inferior trigone lesions. Conclusions: Deep periventricular white matter and insular area in the dominant hemisphere play an important role in many language tasks. Thus aphasia is not a mere cortical function.
Keywords:Clinicoradiological Localization, Aphasia, Stroke, White Matter, Perventricular

1. Introduction
Aphasia is an acquired disorder of language due to brain damage. It can affect either speech production or speech comprehension or both, it also can affect other aspects of language, such as reading and writing. The patient with aphasia might lose partially or completely his ability to communicate verbally or via written words [1] . Stroke is likely the most common cause of aphasia and about 20% of acute stroke patients develop some type of aphasia; language processes are lateralized to the dominant, usually left, hemisphere. This has been determined through anatomoclinical correlation in patients with language disturbances and associated brain pathology. In addition to the known left hemisphere cortical functions in language processing, other structures, including the insula, striatum, thalamus, and subcortical white matter, are involved in language function. The striatum is involved in speech output and prosody; the thalamus is important for cortical arousal and language comprehension. The subcortical white matter interconnects language areas [2] . Aphasic syndromes have been studied since the last century, they include: Broca’s aphasia or expressive aphasia, Wernicke’s or receptive aphasia, Global aphasia, Transcortical aphasias (motor, sensory & mixed), subcortical aphasias and specific syndromes: include alexia (with and without agraphia), pure word deafness and pure word blindness. In 1980s three developments revolutionized thinking about aphasia. First PET, second the functional MRI and third the magnetoencephalography showed that areas in both hemispheres of the brain are activated specifically during language tasks, although the left hemisphere reliably shows more activation in the majority of neurologically normal adults. Furthermore, these functional imaging studies have revealed not only coordinated activations in the previously described language centers, but also activation of more distant areas of cortex [3] .
2. Materials and Methods
A total of 70 ischemic stroke patients selected from Stroke Unit, Ain Shams University Specialized Hospital & Neurology Department, Ain Shams University Hospitals within the first 48h of the onset of stroke. Ethical committee of Ain Shams University Specialized Hospital, Cairo, Egypt had approved the clinical study. The patient, patient family and party were informed orally about objectives, risk factor and benefit of the study. And verbal approvals, consent were obtained and taken. They all have had left hemispheric stroke with aphasia. All were recruited to this study between August 2006 and July 2008. Any age above seven years (complete language development), both sexes were included. Patients with first ever clinical stroke, admitted within the first 2 days from the onset of stroke, with ischemic brain attack. Patients with persistent disturbed conscious level, with aphasia due to pure right cerebral hemisphere damage and past history of previous mental deterioration or dementia were excluded. All patients were subjected to the following: Careful history taking stressing on any past history suggestive of memory impairments or dementia, also stressing on patient’s education level whether illiterate, moderate or high education level. Neurological examination including (NIHSS) National Institute of Health Stroke Scale, Routine laboratory investigations for risk factors of stroke especially in young patients (e.g. collagen profile). Echo cardiography and carotid duplex were done. Language assessments were done two to four weeks from the onset of stroke. Magnetic Resonance Imaging (MRI) was conducted at 1.5 tesla on a General Electric Superconducting Magnet System.MRI brain containing the following studies (T1, T2, Flair, Diffusion & MRA) was performed within the first 48 hours of stroke onset. In each language function we determined the number of affected patients, and then in those patients we determined the different areas in which MRI lesion is present (as described before).
3. Results
The study included 70 acute ischemic stroke patients, presenting with dysphasia. The mean age was 57.93 years old. The study included 37 (53%) female and 33 (47%) male patients. we made Distribution of language functions affection in relation to different MRI lesional areas. As regard Automatic speech disorders were seen in 53 patients (76%) and in the affected group the MRI lesions distribution showed in the following Table1
Careful analysis of the table showed that automatic speech disorder were significantly related to 4 main areas which are Deep Periventricular, Temporal superior, Supramarginal and Frontal inferior orbital.
As regard patients with initiation difficulty the distribution of MRI lesions is as in Table2
Careful analysis of the table showed that initiation difficulty was significantly related to 3 main areas as Periventricular, Insula and Temporal superior.
As regard mute patients the distribution of MRI lesional areas shows the following distribution in Table3
Careful analysis of this table found that mutism is related to many brain areas lesions. However we had almost 10 brain areas lesions showed statistical significance from total 24 areas in the brain, this shows how mutism could be assign in many brain vascular ischemic insults.
Table 1. The distribution of automatic speech disorders over different brain areas in the left hemisphere.
* = statistically significant while ** = highly significant. The p value is of significance when < 0.05, p value > 0.05 non-significant, p value < 0.01 highly significant (Pearson Chi-square test).
* = statistically significant while ** = highly significant. The p value is of significance when < 0.05, p value > 0.05 non-significant, p value < 0.01 highly significant (Pearson Chi-square test).
Case Presentation: A 25 years old female patient married with 2 off springs youngest one year old. The patient was moderately educated and was right handed. She had past history of rheumatic fever and mitral valve disease. The patient presented to ER with acute right sided weakness, upper limb > lower limb and she was unable to walk unsupported, together with difficulty to express herself in words or understand spoken words, her NIHSS was 7. Her CT scan revealed no hemorrhage, so she received antiplatelet and anticoagulants. Two days from onset the patient had an MRI study in our Ain Shams Specialized Hospital revealed a hyperintense left hemispheric lesion in the diffusion & flair studies (see Figure 1). Using the MRI brain, these lesions were located in the following areas: Insula, Rolandic operculum, Precentral, Post central, Supramarginal, Angular, Temporal superior, Temporal pole superior, Parietal inferior, Occipital mid.
This figure shows a hyper intense lesion in the distribution of left MCA territory.
In the 3rd week from illness, the patient came for phoniatric assessment, her dysphasia test revealed the following: She had fluent aphasia.
§ Automatic speech: Normal
§ Speech initiation: Normal
§ Mutism: Absent
§ Repetition: Normal
§ Paraphasias: Present (Semantic)
§ Gargon and neologism: Absent
§ Perseveration: Absent
§ Syntax: Affected
§ Naming: Normal
§ Reading: Affected
§ Reading comprehension: Intact
§ Visual comprehension: Intact
* = statistically significant while ** = highly significant. The p value is of significance when < 0.05, p value > 0.05 non-significant, p value < 0.01 highly significant (Pearson Chi-square test).
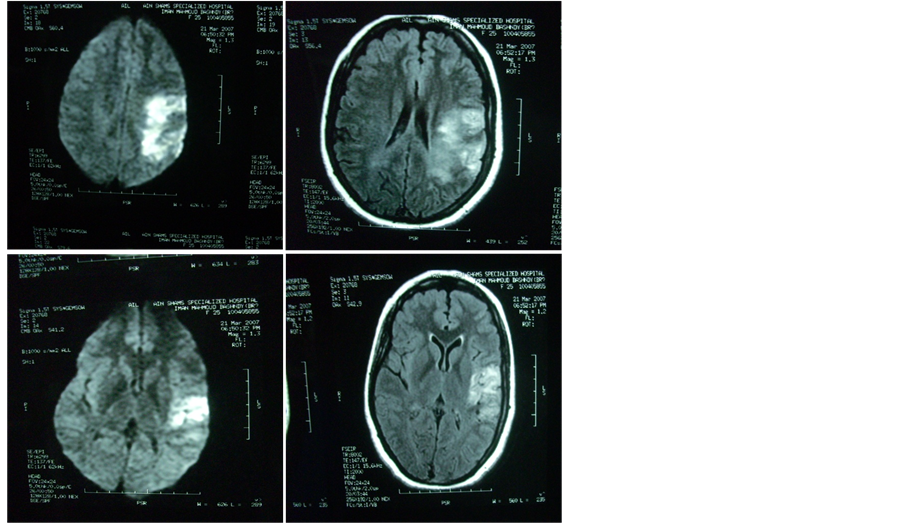
Figure 1. MRI diffusion & flair of this patient.
§ Auditory comprehension affected
§ Color and form perception: Intact
§ Matching: Impaired
§ Writing: Affected
§ Prosody: Affected
§ Calculation: Affected In her follow up one month later, the patient showed marvelous improvement regarding weakness and language problem. The weakness regressed to be only mild upper limb weakness, with no clinically detectable weakness in right lower limb. The family could not notice any language abnormality in the patient except for mild comprehension defect.
4. Discussion
Aphasia is a common complication of stroke that adds more disability to the patients and produces more deterioration to patients’ and relatives’ quality of life. Language functions have been studied many years ago usually in patients with post stroke aphasia. Aphasia can complicate ischemic as well as hemorrhagic stroke. While ischemic stroke lesions respect vascular anatomy, cerebral hematoma behaves by its nature as a space occupying lesion. Aphasic syndromes have been studied since the last century, they include: Broca’s aphasia or expressive aphasia, Wernicke’s or receptive aphasia, Global aphasia, Transcortical aphasias (motor, sensory & mixed), Subcortical aphasias and specific syndromes: include alexia (with and without agraphia), pure word deafness and pure word blindness.
In our study automatic speech disorders were mainly associated with lesions in the deep periventricular white matter and anterior perisylvian regions as insula, temporal superior, rolandic operculum, temporal mid, frontal inferior operculum, and supramarginal area. This results matches to some degree with those results of a study done by Emam (2003) [4] , who found only significant correlation between disorders of automatic speech and insular-external capsule regions. Kreisler et al. (2000) [5] found correlation with lesions in the inferior frontal gyrus and putamenal lesions in left hemisphere. In our study 51% of affected patients had putamenal lesions but also with no significant statistical correlation.
From our results we can suggest that the affection of propositional speech production occurs with lesions to the, left frontal operculum and rostral left temporal cortex. Blank et al. (2002) [6] has reached the same conclusion.
In this study we found that initiation difficulty was significantly correlated with lesions in the following areas: deep periventricular white matter, insula and temporal superior area. Although Kirzinger & Jurgens (1982) [7] stated that the cingulate and the supplementary motor area connect the limbic motivational system and motor initiation system to operate as a starter mechanism for speech and language; we could not find significant correlation with either the cingulate gyrus or the supplementary motor gyrus, however the deep periventricular white matter may play a role in connecting the previously mentioned areas.
Early mutism or difficulty in speech initiation may be over diagnosed as having global aphasia. We found that mutism is significantly correlated with lesions in the following areas: temporal mid area, external capsule, caudate nucleus, internal capsule, supramarginalgyrus, heschgyrus, precentral area, frontal inferior operculum, frontal inferior orbital and pallidum. Our findings (especially the high significant correlation with caudate lesions) may be explained by what is mentioned by Jurgens (1984) [8] that there are two pathways that bring motor activation to language output regions. One originates in the anterior cingulate and supplementary motor areas bilaterally and projects to the region of the frontal operculum. The second pathway originates in the cingulate and projects into the subcallosal fasiculus to the caudate. Anatomical proximity may explain our finding of highly significant correlation with lesions in the temporal mid area, as it lies close to limbic structures. Also Rohrer et al. (2008) [9] stated that lesions affecting the upper brain stem or the frontal cingulate/supplementary area bilaterally can interfere with the initiation of both behavior and verbal output. When it is severe, this state is called akinetic mutism. Suggested that a decrease in speech output can occur in many patients with frontal or subcortical deficits who exhibit a generalized inertia of thought; these results also can explain our findings of significant correlation with many subcortical structures.
5. Conclusion
The classification of aphasias as “expressive” or “receptive” and “motor” or “sensory” is both overly simplistic and inaccurate. The deep periventricular white matter and insular area in the dominant hemisphere play an important role in many language tasks, such as automatic speech production. Thus aphasia is not a mere cortical function.
References
- Kirshner, H.S. and Jacobs, D. (2008) eMedicine Specialties. http://emedicine.medscape.com/article/1135944-overview
- Spreen, O. and Risser, A.H. (2003) Assessment of Aphasia. Oxford University Press, New York, 45-49.
- Hillis, A.E. (2007) Aphasia: Progress in the Last Quarter of a Century. John Hopkins University School of Medicine, Baltimore. (Supported by NIH (NIDCD) from AAN Enterprises, Inc.)
- Emam, A. (2003) The Diagnostic role of Neuroradiology in Dysphasic Patients. Ain Shams University, Cairo.
- Kreisler, A., Godefroy, O., Delmaire, C., et al. (2000) The Anatomy of Aphasia Revisited. Neurology, 54, 1117-1123.
- Blank, S.C., Scott, S.K., Warburton, E., et al. (2002) Speech Production: Wernicke, Broca and Beyond. Brain, 125, 1829-1838. (Quoted from Rohrer et al., 2008)
- Kirzinger, A. and Jurgens, U. (1982) Cortical Lesion Effects and Vocalization in the Squirrel Monkey. Brain Research, 223, 299-315.
- Jurgens, V. (1984) The Efferent and Afferent Connections of the Supplementary Motor Area. Brain Research, 300, 63-81.
- Rohrer, J.D., Knight, W.D., Warren, J.E., et al. (2008) Word Finding Difficulty: A Clinical Analysis of the Progressive Aphasias. Brain, 131, 8-38. http://dx.doi.org/10.1093/brain/awm251


