Open Journal of Rheumatology and Autoimmune Diseases
Vol.3 No.4(2013), Article ID:39707,7 pages DOI:10.4236/ojra.2013.34032
Association between Premenstrual Dysphoric Disorder and Systemic Lupus Erythematosus: Exacerbation of Major Depression Symptoms?
![]()
1Medicine and Human Health Post-Graduation Program, Fundação Bahiana para o Desenvolvimento das Ciências, Escola Bahiana de Medicina e Saúde Pública, Bahia, Brazil; 2Medicine Graduation Program, Faculdade de Tecnologia e Ciências, Bahia, Brazil; 3Department of Psychiatry and Laboratório Interdisciplinar de Neurociências Clínicas (LiNC), Universidade Federal de São Paulo, São Paulo, Brazil; 4Medicine and Human Health Post-Graduation Program, Fundação Bahiana Para o Desenvolvimento das Ciências, Escola Bahiana de Medicina e Saúde Pública, Bahia, Brazil; 5Department of Neuroscience and Mental Health, Universida de Federal da Bahia, Bahia, Brazil.
Email: *silviacal@uol.com.br
Copyright © 2013 Sílvia Fernanda Lima de Moura Cal et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received August 5th, 2013; revised September 5th, 2013; accepted September 12th, 2013
Keywords: Systemic Lupus Erythematous; Depression; Anxiety; Premenstrual Dysphoric Disorder; Premenstrual Syndrome
ABSTRACT
Introduction: Systemic Lupus Erythematosus (SLE) usually presents neuropsychiatric manifestations, such as psychosis, convulsion, mood disorder and chronic headache, with mood disorder being the most prevalent. It is also known that other psychiatric disorders and menstrual cycle disorders are frequent in SLE. The aim of this study was to describe for the first time the frequency of premenstrual dysphoric disorder in patients with SLE diagnosis, and its association with depression and anxiety. Material and Methods: An evaluation was made of 62 (sixty-two) patients with diagnosis of SLE, based on the American College of Rheumatology criteria, who received follow-up care at an ambulatory reference center. The patients were submitted to a sociodemographic evaluation questionnaire, upon which the Mini International Neuropsychiatric Interview (MINI PLUS), Brazilian Version 5.0.0, was used to evaluate the diagnosis. Results: Twenty (32%) patients were found to have premenstrual dysphoric disorder, and there was a statistically significant association with major depression (p = 0.010), but no statistical significance was found with dysthymia (p = 0.063) or anxiety (p = 0.223). Conclusions: The frequency of premenstrual dysphoric disorder (PMDD) in patients with SLE was high, as well as the frequency of major depression in this group. There was an association between these two disorders.
1. Introduction
Systemic Lupus Erythematosus (SLE) is a chronic, autoimmune and systemic disease, whose frequency of neuropsychiatric manifestations varies broadly: 5% - 83% [1-4]. These include seizures, headaches, dizziness, meningitis, delusions, depression, acute organic syndrome, psychosis, anxiety and mood symptoms [3,5,6].
Menstrual cycle disorders are highly prevalent among SLE patients, reaching a rate of 40% due to oligomenorrhea, transient amenorrhea, polymenorrhea, and menorrhagia [7]. Despite this, up to now, premenstrual dysphoric disorder (PMDD) has not been studied in these patients.
In the general population, mild premenstrual mood symptoms occur in up to 80% of women [8-11], but serious cases can impair daily activities, in social, family and work functioning, and cases featuring PMDD range between 2% - 18% [9,12].
PMDD is a mood disorder, characterized by cycle recurrence during the luteal phase of the menstrual cycle, and a variety of emotional and physical symptoms, which are included in the Diagnostic Statistical Manual of Mental Disorders (DSM-IV). There must be clear evidence of complete symptom remission shortly after the onset of menses [13].
In this context, the high prevalence of major depression in SLE patients [6,14,15] and the overlap of PMDD and atypical depressive symptoms, such as hypersomnia, increased appetite, sensitivity to rejection, fatigue, and irritability, may delay the diagnosis of the comorbidity. Furthermore, the association between PMDD and depressive disorders may interfere with the person’s function, result in higher rates of hospital admissions, need of emergency care, suicidal behavior, violent crimes, accidents, prescription of antidepressants, and in the abuse of cigarettes and other drugs [16,17].
On the other hand, PMDD mood swings usually represent a disturbing and debilitating set of symptoms [11] that may be associated with psychiatric comorbidity and are distinct from the premenstrual period [18]. Additionally, studies have shown that the great harm caused by PMDD on the quality of a patient’s life is comparable to disorders like major depression and dysthymia [9].
Frequency of PMS and PMDD seems to be higher in patients with major depressive disorder, compared to groups without psychiatric history [19,20], and the affective symptoms (depression, irritability, anxiety) are the most striking concern of these menstrual cycle problems [21]. However, this interaction has not yet been studied in SLE.
Although there is consensus about the multifactorial etiology of SLE in relation to hormonal (estrogen), genetic, environmental (ultraviolet radiation, drugs), and infectious (viral) factors and psychological stress, the etiology of psychopathology in SLE has not been sufficiently clarified [3,4,22]. Aiming to add information to fill in this gap, this study evaluates the frequency of psychiatric disorders in SLE, especially PMDD, and speculates on the hormonal factors in the pathophysiology of affective disorders in these patients.
The diagnosis and treatment of these conditions could bring an improvement in the clinical condition and favorably interfere with patient recovery [19] while providing greater adherence to treatment and having a direct effect on the immune capacity of the individual [23,24].
2. Material and Methods
This study was conducted in a rheumatology clinic on female patients with SLE, according to the criteria of the American College of Rheumatology, in a cross-sectional design [25]. Patients were initially interviewed using a questionnaire to obtain sociodemographic and clinical data. The patients were assessed using the Mini International Neuropsychiatric Interview (MINI PLUS), Version 5.0.0 validated to Portuguese by Amorim [26], based on the main axis I disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV, American Psychiatric Association, 1994) and the International Statistical Classification of Diseases and Related Health Problems (ICD-10), World Health Organization, 1992). Exclusion criteria were: age under 18 or above 48 years old, being amenorrheic, pregnant, hysterectomized, in early menopause, using hormonal contraception, being unable to answer the questions of the interview due to retardation or psychosis, agitation, or any other incapacitating symptoms during the interview. The patients were evaluated between 2006 and 2008 by a research psychologist (SFC).
The study was approved by the Ethics in Research of Hospital Santa Izabel, and all patients signed an informed consent after being adequately informed about the procedure for the research.
3. Statistical Analysis
Data were analyzed using SPSS (Statistical Package for Social Sciences) version 14.0 for Windows and STATA, version 9.0. The results of continuous variables were analyzed and descriptive methods were used to estimate the mean ± standard deviation (SD), while categorical variables were expressed as proportions. The statistical test used to determine an association between menstrual disorders and each independent variable was Fisher’s Exact Test, and Robust Poisson Regression was used to obtain prevalence ratios and confidence intervals. The significance level was considered significant at p ≤ 0.10.
4. Results
We evaluated 100 women with SLE, and 62 met the criteria for inclusion in the study. In our sample, mean age was 34.53 ± 7.65, with up to 30 years (35.5%) being the most prevalent age group.
Other sociodemographic characteristics are in Table 1.
Of the 62 patients studied, 19 (30.6%) met criteria for PMDD (0.31 ± 0.465), 51 (74%) for any anxiety disorder, 22 (35.5%) for current major depression, 11 (18%) for dysthymia, and 3 (5%) reported suicide attempts (Table 2).
As to the medications used, only 5 (8%) patients were taking antidepressant medication, 12 (19%) were taking Azatioprine, 5 (8%) were on Chloroquine, and 15 (24%) on Hydroxychloroquine sulfate.
Using the Fisher’s Exact test, we found an association between PMDD and current major depression (p = 0.021). However, we did not find an association between PMDD and anxiety disorders, nor between PMDD and dysthymia. There was also no association with disease duration or with corticosteroid use. There was an association be-
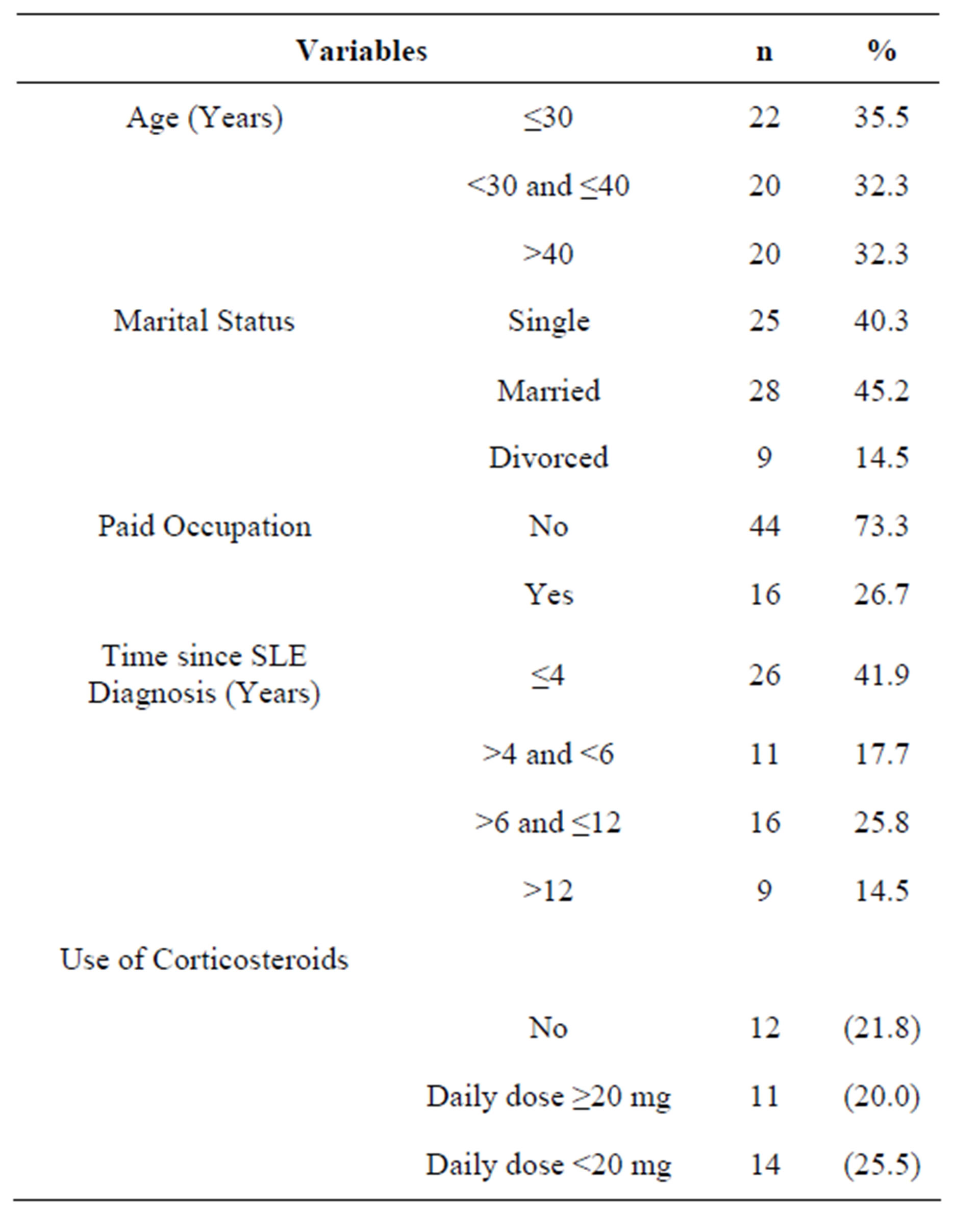
Table 1. Sociodemographic and clinical characteristics of SLE patients.
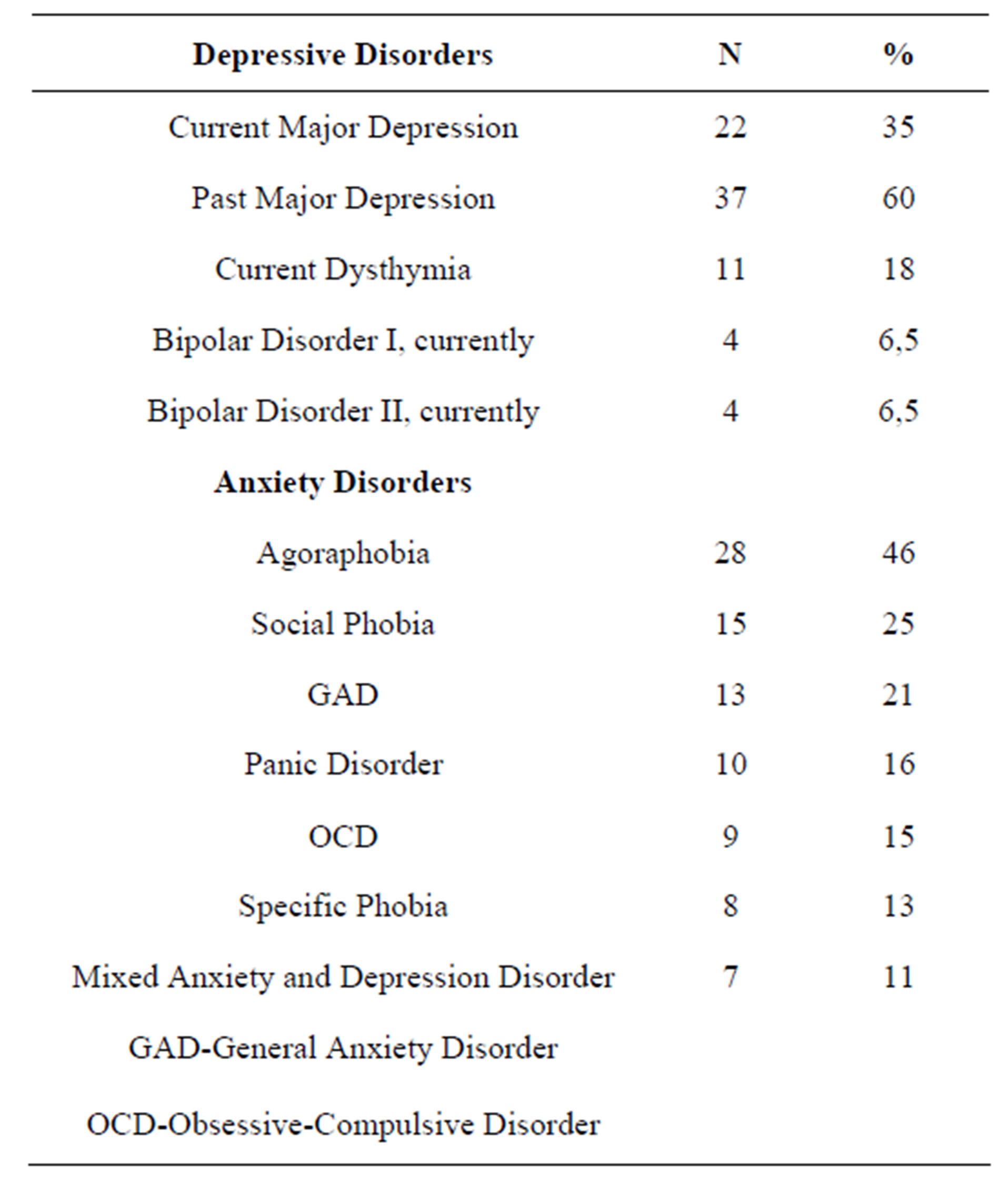
Table 2. Frequency of mood and anxiety disorders in the SLE patients.
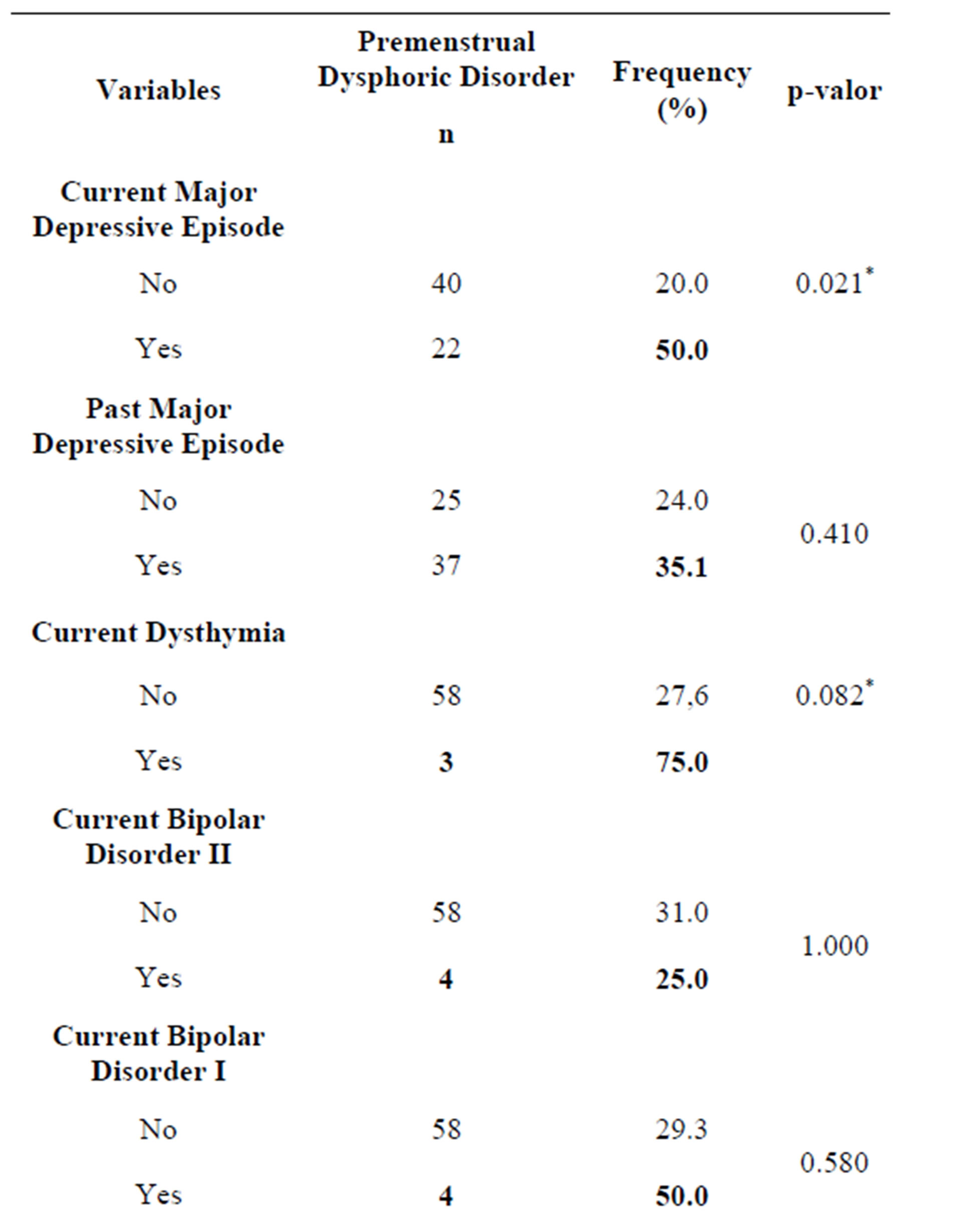
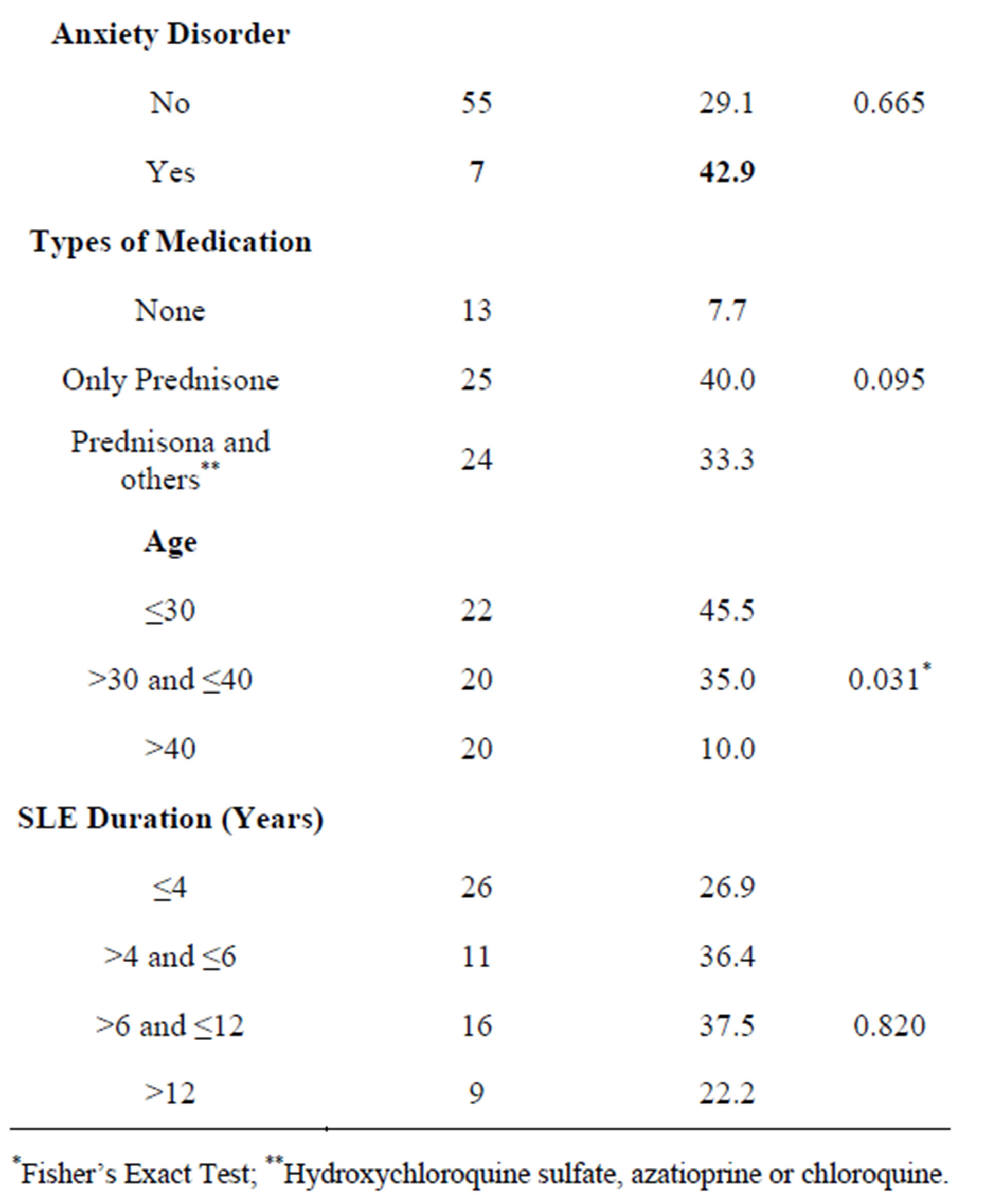
Table 3. Association between PMDD, clinical and sociodemographic variables in the SLE patients.
tween age and PMDD, and the range of up to 30 years was subject to the symptoms (Table 3).
It was observed that those who had a current major depressive episode had 2.5 times more chances of having PMDD, while the prevalence ratios for the other disorders were not statistically significant (Table 4).
5. Discussion
Although menstruation is an important event in a woman’s reproductive cycle, it may interfere with various aspects of her life, since at these periods she tends to engage in more family conflicts, place less emphasis on objective or intellectual values, and lose autonomy and innovation in her field of work [27]. Most women do not accurately report the onset of symptoms, which leads one to believe the syndrome is an insidious process [28] and mainly identify it after it has become exacerbated in situations of anxiety, fear, and stress [21,28]. Generally, women seek treatment about ten years after the onset of symptoms, when they will be more intense and have longer duration with the passing years, as well as history of more occupational damage [28]. In the case of SLE patients, who already live with the stress of having a chronic illness that is already unpredictable, this corre
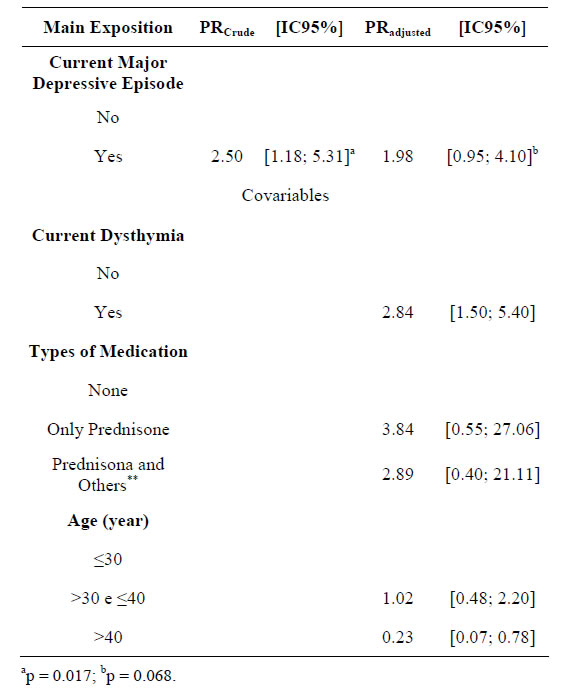
Table 4. Values of the crude and adjusted prevalence ratios, with a confidence interval, for premenstrual dysphoric disorder, calculated by Robust Poisson Regression.
sponds to an overload of loss of the patient’s quality of life, which can impair adherence to treatment and its success. Such a situation, associated with high comorbidity with depression [6,15,29], may explain the high prevalence of PMDD in SLE patients, with significant consequences in their personal, social, and economical lives; not only for the women involved but also for society, especially the state coffers [24], since the damage to quality of life as a whole often corresponds to significant losses [9].
In patients with SLE, this distinction becomes even more difficult since the prevalence of psychiatric symptoms, including depression, is high [3,23]. Women with mood disorders are prone to an exacerbation of the affective symptoms during the premenstrual period [17], and history of previous depression could influence the severity and duration of depressive symptoms in the premenstrual period, resulting in an association with PMDD [16,21,30]. The symptoms of irritability and nervousness, besides depressed mood, are recurrent in PMDD and are common characteristics in cases of atypical depression [11,27,31].
Dysphoria experienced repeatedly can lead to gradual development of an affective disorder in individuals with a genetic predisposition, thus, pre-menstrual depression could precede a case of major depression, as being the manifestation of this already-established pathology [31, 32].
Hartlage et al. (2001) found in a small-sampled study that the majority of women who experienced PMDD for a long time had a risk of developing depression later [33]. As for some authors, some mental illnesses, such as major depression, panic disorder, bulimia nervosa, schizophrenia, and other medical conditions such as asthma and epilepsy worsened in the premenstrual phase which corresponds to the [33] phenomenon of premenstrual exacerbation [17,34,35].
Exacerbation of depression prior to menstruation was present in approximately 50% of women admitted to gynecological, obstetric and psychiatric units [34,36]. The fact remains that it is a time of greater biological vulnerability [37]. This vulnerability arises from a combination of changes resulting from hormonal fluctuations and external circumstances that are not cycle changes per se, but influence the woman’s reaction in generating the occasional changes, so many areas of risk come into play. Situations were cited as the premature loss of parents, sexual abuse, disability, social support system in these children, traumatic events, stressors, interpersonal difficulties, history of previous depressive disorders or family [20, 26]. An association with a worsening of premenstrual symptoms during adverse situations or stressful experiences have been documented and is consistent with clinical experience [16,21,30].
In the present study, we found a statistically significant association between a current major depression episode and PMDD, which is in agreement with the literature [12,30]. On the other hand, no association was found between a diagnosis of past major depressive episode and PMDD, which differs from the work of Halbreich and Endicot (1985). Also, there was no association between Bipolar Disorder I and II and PMDD, although there is still no consensus in the literature regarding this association [38,39]. Despite the fact that dysthymia and anxiety disorders are mentioned as risk factors for PMDD, we could not find a statistically significant association.
The majority of the patients were being treated with corticosteroids; and its use, as well as chronic stress, can alter the hormonal ratio of androgen/estrogen and thus interfere with the menstrual cycle. However, in this study no association was found between the use of corticosteroids and PMDD [40] and not even between the presence of depression and the use of prednisone doses higher than 20 mg/day. Although there is no consensus over what the threshold is for corticosteroids to set off psychiatric alterations, there is a study that suggests that such manifestations appear with the use of doses over 40 mg/day [23].
The psychiatric comorbidity, in turn, can impair the immune capacity of patients with SLE. Several studies have shown that depressive symptoms are associated with compromised immune function and increased susceptibility to infections [41,42].
In this sample, only 12 patients (34%) reported difficulties in daily activities with reduced efficiency at work and relationship problems in the premenstrual period, which differs from other studies [5,12]. Perhaps the fact that 44 (73.3%) patients were outside the job market may have contributed to the low rate found. On the other hand, complaints such as “irritation, fights and frequent explosions”, common in patients with PMS/PMDD, were also found in only 24% of the patients [15].
This study has limitations such as the small sample size and the fact that there was no monitoring to verify whether the symptoms would persist for more than 2 or 3 months. Nor was it possible to categorize the symptoms by level of severity, due to the limitations of the instrument used. Another limitation is that there was no comparison between the phase of active PMDD and inactive SLE.
Regarding treatment, pharmacological intervention, such as the use of serotonin reuptake inhibitors (SRIs) (fluoxetine, sertraline, citalopram, paroxetine, venlafaxine and clomipramine) is the most appropriate and effective treatment for severe PMS/PMDD [12,37,43]. The response rate of patients is around 60% - 90%, improving not only the mood, but also the somatic symptoms and consequently the quality of life and social functioning; there is also the advantage of these drugs having mild side effects [8,14]. Glick et al. noted however, that a group of women did not respond to treatment with antidepressants and continued to experience premenstrual dysphoric symptoms. The authors believe that this group should have two separate conditions or comorbidities, and only one responded to antidepressants [44], most likely due to several psychiatric conditions, some of which may be comorbid with mood disorders that have been described as exacerbated during the premenstrual period [17]. In the SLE group there is high psychiatric comorbidity, which requires careful attention and individualized follow-up, associated with the work of the mental health team, reinforcing the importance of a multidisciplinary team working together in the Rheumatology outpatient clinic [6,15,29,45].
6. Conclusions
The frequency of PMDD was high in sample of SLE patients, as was the frequency of major depression. There was a significant association between these two diseases, but only in current depression, reinforcing the need for greater attention to psychiatric comorbidity in SLE.
Further studies are needed before one can know how these women experience and deal with PMDD, which symptoms are the most common in this population and their repercussions, in addition to answering questions such as: Could the vulnerability in the more acute premenstrual period interfere with SLE, leading to a worsening of the disease or triggering an outbreak of SLE? It is hoped that this initiative may serve to stimulate new research and allow for greater attention to comorbidities such as those described in the context of SLE.
7. Acknowledgements
This study was supported by a FAPESB (Research Support Foundation of Bahia) grant; #1445/2007. The authors of this paper do not have any commercial associations that might pose conflict of interest in connection with this manuscript.
REFERENCES
- J. F. Ampelas, M. J. Wattiaux and A. P. Van Amerongen, “Psychiatric Manifestations of Lupus Erythematosus Systemic and Sjogren’s Syndrome,” Encephale, Vol. 27, No. 6, 2001, pp. 588-599.
- J. G. Hanly, G. McCurdy, L. Fougere, J. A. Douglas and K. Thompson, “Neuropsychiatric Events in Systemic Lupus Erythematosus: Attribution and Clinical Significance,” Journal of Rheumatology, Vol. 31, No. 11, 2004, pp. 2156- 2162.
- E. C. Miguel, R. M. Pereira, C. A. Pereira, L. Baer, R. E. Gomes, L. C. de Sa, et al., “Psychiatric Manifestations of Systemic Lupus Erythematosus: Clinical Features, Symptoms, and Signs of Central Nervous System Activity in 43 Patients,” Medicine (Baltimore), Vol. 73, No. 4, 1994, pp. 224-232. http://dx.doi.org/10.1097/00005792-199407000-00005
- F. G. Nery, E. F. Borba, J. P. Hatch, J. C. Soares, E. Bonfa and F. L. Neto, “Major Depressive Disorder and Disease Activity in Systemic Lupus Erythematosus,” Comprehensive Psychiatry, Vol. 48, No. 1, 2007, pp. 14-19. http://dx.doi.org/10.1016/j.comppsych.2006.04.002
- ACR Ad Hoc Committee on Neuropsychiatric Lupus Nomenclature, “The American College of Rheumatology Nomenclature and Care Definitions for Neuropsychiatric Lupus Syndromes,” Arthritis & Rheumatism, Vol. 42, No. 4, 1999, pp. 599-608.
- F. G. Nery, E. F. Borba, V. S. Viana, J. P. Hatch, J. C. Soares, E. Bonfa, et al., “Prevalence of Depressive and Anxiety Disorders in Systemic Lupus Erythematosus and Their Association with Anti-Ribosomal P Antibodies,” Progress in Neuro-Psychopharmacology & Biological Psychiatry, Vol. 32, No. 3, 2008, pp. 695-700. http://dx.doi.org/10.1016/j.pnpbp.2007.11.014
- N. N. Fatnoon, S. M. Azarisman and D. Zainal, “Prevalence and Risk Factors for Menstrual Disorders among Systemic Lupus Erythematosus Patients,” Singapore Medical Journal, Vol. 49, No. 5, 2008, pp. 413-418.
- B. B. Dean, J. E. Borenstein, K. Knight and K. Yonkers, “Evaluating the Criteria Used for Identification of PMS,” Journal of Women’s Health (Larchmt), Vol. 15, No. 5, 2006, pp. 546-555. http://dx.doi.org/10.1089/jwh.2006.15.546
- U. Halbreich, J. Borenstein, T. Pearlstein and L. S. Kahn, “The Prevalence, Impairment, Impact, and Burden of Premenstrual Dysphoric Disorder (PMS/PMDD),” Psychoneuroendocrinology, Vol. 28, No. S3, 2003, pp. 1-23. http://dx.doi.org/10.1016/S0306-4530(03)00098-2
- J. F. Mortola, “Premenstrual Syndrome,” Trends in Endocrinology & Metabolism, Vol. 7, No. 5, 1996, pp. 184- 189. http://dx.doi.org/10.1016/1043-2760(96)00060-4
- G. C. Valadares, L. Ferreira, H. Correa Filho and M. Romano-Silva, “Transtorno Disfórico Pré-Menstrual Revisão: Conceito, História, Epidemiologia e Etiologia,” Revista de Psiquiatria Clínica, Vol. 33, 2006, pp. 117-123. http://dx.doi.org/10.1590/S0101-60832006000300001
- K. Yonkers, P. M. O’Brien and E. Ericksson, “Premenstrual Syndrome,” The Lancet, Vol. 371, No. 9619, 2008, pp. 1200-1210. http://dx.doi.org/10.1016/S0140-6736(08)60527-9
- S. Girdler and R. Klatzkin, “Neurosteroid in the Context of Stress: Implications for Depressive Disorders,” Pharmacology & Therapeutics, Vol. 116, No. 1, 2007, pp. 125-139. http://dx.doi.org/10.1016/j.pharmthera.2007.05.006
- H. Ainiala, J. Loukkola, J. Peltola, M. Korpela and A. Hietaharju, “The Prevalence of Neuropsychiatric Syndromes in Systemic Lupus Erythematosus,” Neurology, Vol. 57, No. 3, 2001, pp. 496-500. http://dx.doi.org/10.1212/WNL.57.3.496
- E. A. Bachen, M. A. Chesney and L. A. Criswell, “Prevalence of Mood and Anxiety Disorders in Women with Systemic Lupus Erythematosus,” Arthritis & Rheumatism, Vol. 61, No. 6, 2009, pp. 822-829. http://dx.doi.org/10.1002/art.24519
- U. Halbreich and J. Endicott, “Relationship of Dysphoric Premenstrual Changes to Depressive Disorders,” Acta Psychiatrica Scandinavica, Vol. 71, No. 4, 1985, pp. 331- 338. http://dx.doi.org/10.1111/j.1600-0447.1985.tb02532.x
- M. N. Miller and B. E. Miller, “Premenstrual Exacerbations of Mood Disorders,” Psychopharmacological Bulletin, Vol. 35, No. 3, 2001, pp. 135-149.
- L. A. Futterman and A. J. Rapkin, “Diagnosis of Premenstrual Disorders,” The Journal of Reproductive Medicine, Vol. 51, No. 4, 2006, pp. 349-358.
- J. W. Bailey and L. S. Cohen, “Prevalence of Mood and Anxiety Disorders in Women Who Seek Treatment for Premenstrual Syndrome,” Journal of Women’s Health & Gender-Based Medicine, Vol. 8, No. 9, 1999, pp. 1181- 1184. http://dx.doi.org/10.1089/jwh.1.1999.8.1181
- J. Endicott, “The Menstrual Cycle and Mood Disorders,” Journal of Affective Disorders, Vol. 29, No. 2-3, 1993, pp. 193-200. http://dx.doi.org/10.1016/0165-0327(93)90033-G
- M. Pires and H. Calil, “Associação Entre Transtorno Disfórico Pré-Menstrual e Transtornos Depressivos,” Revista Brasileira de Psiquiatria, Vol. 21, 1999, pp. 118-127. http://dx.doi.org/10.1590/S1516-44461999000200011
- D. G. Ayache and I. Costa, “Alterações da Personalidade no Lúpus Eritematoso Sistêmico,” The Brazilian Journal of Rheumatology, Vol. 45, No. 5, 2005, pp. 313-318.
- M. Alpay and E. H. Cassem, “Diagnosis and Treatment of Mood Disorders in Patients with Rheumatic Disease,” Annals of the Rheumatic Diseases, Vol. 59, No. 1, 2000, pp. 2-4. http://dx.doi.org/10.1136/ard.59.1.2
- D. P. Chapman, G. S. Perry and T. W. Strine, “The Vital Link between Chronic Disease and Depressive Disorders,” Preventing Chronic Disease, Vol. 2, No. 1, 2005, p. A14.
- E. M. Tan, A. S. Cohen, J. F. Fries, A. T. Masi, D. J. McShane, N. F. Rothfield, et al., “The 1982 Revised Criteria for the Classification of Systemic Lupus Erythematosus,” rthritis & Rheumatism, Vol. 25, No. 11, 1982, pp. 1271- 1277.
- P. Amorim, “Mini International Neuropsychiatric Interview (MINI): Validação de Entrevista Breve para Diagnóstico de Transtornos Mentais/Mini International Neuropsychiatric Interview (MINI): Validation of a Short Structured Diagnostic Psychiatric Interview,” The Revista Brasileira de Psiquiatria, Vol. 22, No. 3, 2000, pp. 106-115.
- U. Halbreich, “The Etiology, Biology, and Evolving Pathology of Premenstrual Syndromes,” Psychoneuroendocrinology, Vol. 28, No. S3, 2003, pp. 55-99. http://dx.doi.org/10.1016/S0306-4530(03)00097-0
- I. Rodrigues and E. Oliveira, “Prevalência e Convivência de Mulheres com Síndrome Pré-Menstrual,” Arquivos de Ciências da Saúde, Vol. 13, No. 3, 2006, pp. 146-152.
- S. F. Cal, A. P. Borges and M. B. Santiago, “Prevalência e classificação da Depressão em Pacientes com Lúpus Eritematoso Sistêmico Atendidos em um Serviço de Referência da Cidade de Salvador,” Jornal da LIRRNE, Vol. 2, 2006, pp. 36-43.
- J. Bancroft, D. Rennie and P. Warner, “Vulnerability to Perimenstrual Mood Change: The Relevance of a Past History of Depressive Disorder,” Psychosomatic Medicine, Vol. 56, No. 3, 1994, pp. 225-231.
- C. M. Nogueira and J. Pinto, “Prevalência dos Sintomas da Síndrome Pré-Menstrual,” Revista Brasileira de Ginecologia e Obstetricia, Vol. 22, 2000, pp. 347-351. http://dx.doi.org/10.1590/S0100-72032000000600005
- T. B. Pearlstein, “Hormones and Depression: What Are the Facts about Premenstrual Syndrome, Menopause, and Hormone Replacement Therapy?” American Journal of Obstetrics & Gynecology, Vol. 173, No. 2, 1995, pp. 646- 653. http://dx.doi.org/10.1016/0002-9378(95)90297-X
- S. A. Hartlage, K. E. Arduino and S. Gehlert, “Premenstrual Dysphoric Disorder and Risk for Major Depressive Disorder: A Preliminary Study,” Journal of Clinical Psychology, Vol. 57, No. 12, 2001, pp. 1571-1578. http://dx.doi.org/10.1002/jclp.1119
- F. Akdeniz and F. Karadag, “Does Menstrual Cycle Affect Mood Disorders?” Türk Psikiyatri Dergisi, Vol. 17, No. 4, 2006, pp. 296-304.
- P. K. Braverman, “Premenstrual Syndrome and Premenstrual Dysphoric Disorder,” Journal of Pediatric & Adolescent Gynecology, Vol. 20, No. 1, 2007, pp. 3-12. http://dx.doi.org/10.1016/j.jpag.2006.10.007
- L. Plouffe Jr., K. Stewart, K. S. Craft, M. S. Maddox and J. L. Rausch, “Diagnostic and Treatment Results from a Southeastern Academic Center-Based Premenstrual Syndrome Clinic: The First Year,” American Journal of Obstetrics Gynecology, Vol. 169, No. 2, Pt. 1, 1993, pp. 295- 303.
- T. B. Pearlstein, U. Halbreich, E. D. Batzar, C. S. Brown, J. Endicott, E. Frank, et al., “Psychosocial Functioning in Women with Premenstrual Dysphoric Disorder before and after Treatment with Sertraline or Placebo,” The Journal of Clinical Psychiatry, Vol. 61, No. 2, 2000, pp. 101-109. http://dx.doi.org/10.4088/JCP.v61n0205
- A. D’Mello, L. Pinheiro and M. Lalined-Michaud, “PreMenstrual Mania: Two Case Report,” The Journal of Nervous and Mental Disease, Vol. 181, No. 5, 1993, pp. 330-331. http://dx.doi.org/10.1097/00005053-199305000-00011
- D. Conrad and A. H. Hamilton, “Recurrent Premenstrual Declive in Serum Lithium Concentration: Clinical Correlates and Treatment Implications,” Journal of the American Academy of Child Psychiatry, Vol. 25, No. 6, 1986, 852-853. http://dx.doi.org/10.1016/S0002-7138(09)60206-5
- M. Cutolo, S. Capellino, A. Sulli, B. Serioli, M. E. Secchi, B. Villaggio and R. H. Straub, “Estrogens and autoimmune diseases,” Annals of New York Academy of Sciences, Vol. 1089, 2006, pp. 538-547.
- D. Moreira and J. Mello Filho, “Psicoimunologia Hoje,” In: Artmed Ed., Psicossomática Hoje, Porto Alegre, 1992, pp. 119-151.
- S. O. Nunes, E. M. Reich, H. K. Morimoto, E. N. Itano, E. C. Xavier, C. M. Yamoshita, et al., “Immune and Hormonal Activity in Adults Suffering from Depression,” Brazilian Journal of Medical and Biological Research, Vol. 35, No. 5, 2002, pp. 581-587. http://dx.doi.org/10.1590/S0100-879X2002000500011
- A. Rapkin, “A Review of Treatment of Premenstrual Syndrome and Premenstrual Dysphoric Disorder,” Psychoneuroendcrinology, Vol. 28, Suppl. 3, 2003, pp. 39-53.
- R. Glick, W. Harrison, J. Endicott, P. McGrath and F. M. Quitkin, “Treatment of Premenstrual Dysphoric Symptoms in Depressed Women,” Journal of American Medical Women’s Association, Vol. 46, No. 6, 1991, pp. 182- 185.
- N. Navarrete-Navarrete, M. I. Peralta-Ramírez, J. M. Sabio, I. Martínez-Egea, A. Santos-Ruiz and J. JiménezAlonso, “Quality-of-Life Predictor Factors in Patients with SLE and Their Modification after Cognitive Behavioural Therapy,” Lupus, Vol. 19, No. 14, 2010, pp. 1632-1639. http://dx.doi.org/10.1177/0961203310378413
NOTES
*Corresponding author.

