Open Journal of Orthopedics
Vol.06 No.07(2016), Article ID:68505,10 pages
10.4236/ojo.2016.67028
The Outcome of Minimally Invasive Discectomy in Single Level Lumbar Disc Prolapse
Hamid A. Jaff, Bakhtyar Rasul M. Amin, Rebar M. Noori Fatah, Hosam H. Husein
Department of Orthopedic, College of Medicine, University of Sulaimani, Kurdistan, Iraq

Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 20 May 2016; accepted 15 July 2016; published 18 July 2016
ABSTRACT
Lumbar disc surgery in carefully selected patients who have failed conservative treatments can significantly improve quality of life. Minimally invasive treatment of lumbar disc herniation has been popularized in recent years. The aim of the study was to assess the outcome of minimal invasive (loupe) discectomy among lumbar disc prolapse patients in Sulaimani. A prospective study carried out in Shar and Sulaimani Teaching hospitals in Sulaimani city for period from 1st of February, 2013 to end of June, 2014 on sample of 30 patients with single level lumbar disc pro- lapse admitted to orthopedic units. The data were collected by the researcher through direct inter- view and filling a prepared questionnaire. The outcome of surgery was evaluated by comparing the symptoms (back pain, leg pain, and leg parathesia) and the muscle power grading (EHL & FHL) of the patients pre- and post-operatively. Mean age of studied patients was 39.1 ± 9.3 years. Males were more than females. Disc prolapse level was L4-L5 among 17 and L5-S1 among 13 patients. Studying the symptoms pre- and post-operatively, revealed significant decrease in leg pain, leg parathesia and back pain post-operatively (p < 0.001). Studying EHL & FHL power grading pre- and post-operatively, revealed significant increase in muscle power grades 4 and grade 5 postoperatively (p < 0.001). We concluded that minimal invasive discectomy is good and safe treatment option for lumbar disc prolapse.
Keywords:
Disc Prolapse, Diskectomy

1. Introduction
Lumbar disc herniation is a prevalent condition and symptomatic patients present a significant socioeconomic and health burden [1] . Spinal surgery in carefully selected patients who have failed conservative treatments can significantly improve quality of life [1] [2] . Sciatica, better defined as sciatic neuralgia or lumbosacral radicular syndrome (LSRS), is a frequently diagnosed debilitating spine disorder with an estimated yearly incidence of 5 - 10 per 1000 persons [3] . The impact of low back-related disorders is quite high, as they remain the number one cause of work disability in most Western countries. Sciatica manifests itself as radiating dermatome pain regularly accompanied by diminished jerk reflexes, sensory and motor deficits [4] .
Minimally invasive treatment of lumbar disc herniation has been popularized in recent years. The concept of minimally invasive spine surgery comprises reduced muscle injury while achieving good clinical outcome comparable to conventional open surgery. Patients are expected to have less low-back pain, shorter hospitalization, faster mobilization and recovery, and quicker resumption of work and daily activities. In addition, cost-effec- tiveness is expected to favor minimally invasive surgery [5] .
The standard surgical treatment of lumbar disc herniation has been open discectomy [6] but there has been a trend towards minimally invasive procedures. The minimal invasive discectomy is traditionally done by mobilizing the muscles laterally off the spinous process and lamina using a unilateral retractor. A minimally invasive discectomy is thought to decreases surgical morbidity [7] [8] . The purported benefit of the minimally invasive approach is that it would allow patients to recover more quickly because of less tissue trauma [9] . The success rate of lumbar discectomy is about 70% to 90%. Micro discectomy and minimally invasive discectomy decrease surgical exposure and trauma and have success rates of approximately 90% [10] . The surgical treatment of prolapsed lumbar intervertebral disc has evolved since the initial report of lumbar discectomy by Mixter and Barr in 1934 [11] .
Lumbar discectomy is the traditional and most common surgical procedure performed in the United States for a ruptured or herniated lumbar disc in the lumbar spine; it is the most performed spinal surgical procedure worldwide [12] [13] . More than 435,000 herniated lumbar discs in the U.S. receive a discectomy annually [14] .
2. Patients & Methods
2.1. Patients
A prospective study carried out in Shar and Al-Sulaimaniyah Teaching hospitals in Sulaimaniyah city for period from 1st of February, 2013 to end of June, 2014 on sample of 30 patients with lumbar disc prolapse admitted to orthopedic units.
2.1.1. Inclusion Criteria
Patients with lumbar disc herniation (single level) visualized on MRI. (As single level disc prolapse is much more common than multiple level prolapses) with signs and symptoms consistent with symptomatic involvement of the nerve root exiting the adjacent neural foramen, including radicular leg pain (unilateral or bilateral).
2.1.2. Exclusion Criteria
Disc herniation with multiple levels.
Spondylodiskitis.
Segmental instability with disc prolapsed.
Psychogenic disorders.
Previous lumbar surgery.
2.2. Methods
All patients has been notified about their inclusion in this research and also informed consent has been taken from them that they will be included in this desretation.
2.2.1. Data Collection
The data were collected by the researcher through direct interview and filling a prepared questionnaire including the following information:
-Demographic: age, gender and occupation.
-Disc level.
-Preoperative symptoms: like leg pain, leg parathesia, back pain, muscle weakness and duration of these symptoms.
-Intraoperative complications: bleeding, dural tear, and nerve root injury.
-Postoperative symptoms: Leg pain, leg parathesia, back pain and infection.
-Telephone number.
The outcome of surgery was evaluated by comparing the symptoms (back pain, leg pain, and leg parathesia) and muscle power grading (EHL & FHL) of the patients pre and post-operatively.
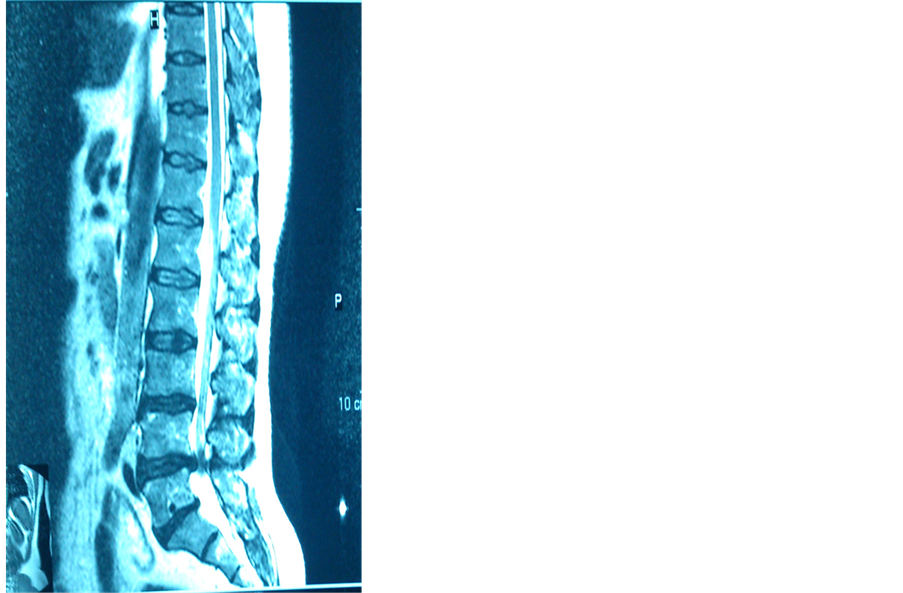
The preoperative diagnosis was made by history, examination, plain radiographs, and MRI (Figure 1).
2.2.2. Muscle Strength
Muscle power was assessed using the Medical Research Council grading system―MRC scale [15] . Extensor hallucis longus (mainly L5) and flexor hallucis longus (mainly S1) muscles power grading was used to assess muscle power of studied patients pre and post-operatively. We test the strength of each muscle and record it in a systematic fashion. We conducted testing each muscle immediately with testing of its contralateral counterpart to enhance detection of any asymmetries [15] . Muscle strength is often rated on a scale of 0/5 to 5/5 as follows:
・ 0/5: no contraction.
・ 1/5: muscle flicker, but no movement.
・ 2/5: movement possible, but not against gravity.
・ 3/5: movement possible against gravity, but not against resistance.
・ 4/5: movement possible against some resistance.
・ 5/5: normal strength.
To assess the strength of the EHL, we (right-handed surgeon), stood on the patient's right side, resisting foot dorsiflexion with the dorsum of the right hand, and tested extension of the big toe with the left middle finger, or both the index and middle finger, placed at the level of the distal phalanx of the big toe. This maneuver allows the EHL to exert its maximal strength in isolation. To assess the strength of the FHL, the patient was in supine position with the ankle in 30˚ planter flexion, the metatarsophalangeal joint was stabilized by one hand (left hand) and holding the proximal phalanx of the big toe in neutral position, the distal phalanx of the big toe was placed in extention by the other hand (right hand) and then we instruct the patient to do big toe flexion [16] .
Figure 1. Shows the one of MRI scan of studied patients.
2.2.3. Operative Technique
MID with loupe was performed under spinal anesthesia. The patient was placed prone or (knee chest position) on a radiolucent frame suitable for fluoroscopy. Placement of the initial intravenous cannula was confirmed with a lateral fluoroscope. An incision of 2 cm was done over the underlying level of disc Prolapse (Figure 2). The Para spinal muscles where released by blunt dissection and a modified mini Taylor retractor with micro discectomy retractor was used to sweep the Para spinal musculature off the lamina edge. The loupe was then put on and adjusted such that the surgeon can used it to monitor the operation. A flavectomy was performed using a knife and a nerve hook with an upwards angle and a Kerrison punch. The dura and traversing nerve root were then identified. Subsequently, the nerve root was retracted medially to expose the herniated disc. The herniated disc was then removed with a pituitary rongeur. Following nerve root decompression, the retractor was removed and the fascia and 2-cm incision wound was closed.
2.2.4. Follow Up
All patients were examined 6 hours after the operation and the day after operation and after an interval of one month after surgery. Each follow-up examination was carried out by the researcher for back pain, leg pain and parathesia, and for muscle power.
3. Results
A total 30 patients with disc prolapse were undergone minimally invasive discectomy and included in this study. Mean age of studied patients was 39.1 ± 9.3 years, 60% of them were ≥40 years age and 40% of them were <40 years age. Nineteen (63.3%) patients were males and 11 (36.7%) were females. Half of studied patients were self-employed, 11 (36.7%) patients were housewives and 4 (13.3%) were public servants, Table 1.
Disc prolapse level was L4-L5 among 17 (56.7%) and L5-S1 among 13 (43.3%), Table 2.
Mean duration of disc prolapse symptoms preoperatively was 10 ± 9 weeks. Two thirds (70%) of studied patients had right leg pain, right leg parasthesia and right muscle weakness, on other hand, 9 (30%) patients had left leg pain, left leg parasthesia and left muscle weakness. Back pain was present among all patients (100%), Table 3.
EHL grade 4 was present preoperatively among 40% of studied patients, grade 3 (36.7%), grade 2 (13.3%), grade 5 (6.7%) and grade 1 (3.3%). FHL grade 3 was present among 33.3% of studied patients, grade 4 (30%), grade 5 (23.3%) and grade 2 (13.4%), Table 4.
4. Statistical Analysis
All patients’ data entered using computerized statistical software; Statistical Package for Social Sciences (SPSS) version 17 was used. In all statistical analysis, level of significance (p value) set at ≤0.05 and the results
Figure 2. Incision for minimal invasive discectomy.
Table 1. Demographic characteristics of patients.
Table 2. Site of disc prolapse among studied patients.
Table 3. Preoperative symptoms of disc prolapse patients.
Table 4. Preoperative EHL & FHL grading for muscles of patients.
presented as tables and or graphs. Descriptive statistics presented as (mean ± standard deviation), frequencies and percentages. Multiple contingency tables conducted and appropriate statistical tests performed, Chi-square used for categorical variables. Fishers exact test used when more than 20% of expected variables less than 5. Statistical analysis of the study was done by the specialist in community medicine.
One month postoperatively, leg pain was absent among 25 (83.3%) patients and present among 5 (16.7%) patients. Leg parasthesia was absent among all the patients postoperatively. Nineteen (63.3%) patients had back pain postoperatively and 11 (36.7%) had no back pain. all the studied patients had no infection postoperatively, Table 5.
One month postoperatively, EHL grade 5 was present among 17 (56.7%), grade 4 (36.7%), grade 3 (6.7%) and no patients with grades 1, 2. FHL grade 5 was present among 17 (56.7%), grade 4 (43.3%) and no patients in grades 1-3. All these findings were shown in Table 6.
Studying the symptoms pre and post-operatively revealed significant decrease in leg pain, leg parasthesia and back pain post-operatively (p < 0.001), Table 7.
Studying EHL & FHL grading pre and post-operatively revealed significant increase in grade 4 and grade 5 postoperatively (p < 0.001), Table 8.
Intraoperative complications were present among 4 (13.3%) patients and 26 (86.7%) patients had no complications. bleeding was the intra-operative complication for 4 patients, Table 9.
We have no postoperative complications.
5. Discussion
Minimally invasive techniques have the theoretical advantage of less tissue scarring and better visualization of the dura, roots and disc space (as they are done under magnification of operating loupes microscopes), and hence are expected to have better postoperative outcomes [17] .
Mean age of our patients with lumbar disc prolapse was 39.1 ± 9.3 years and more than half of them were ≥ 40 years age, this is goes with Grag B, et al. study in India (2011) [10] whom report mean age of patients with lumbar disc prolapse as 38.7 ± 8 and Lee YG, et al. study in South Korea (2010) [18] reported that high proportion of patients with lumbar disc prolapse tend to occur after 40 years of age. Males with lumbar disc prolapse in present study were more than females (63.3% vs. 36.7%). This finding is close to results of Hardenbrook M, et al. study in USA (2013) [19] (60% vs. 40%).
Table 5. Postoperative symptoms.
Table 6. Postoperative EHL & FHL grading of muscles for patients.
Table 7. Distribution of patients symptoms pre and post-operatively.
Table 8. Distribution of EHL & FHL grading pre and post-operatively.
*Fishers exact test.
Table 9. Intraoperative complications.
Half of patients in this study were self-employed with history of heavy works. This result agreed with results of Seidler A, et al. study in Germany (2003) [20] which reported a statistically significant relation between cumulative exposures to weight lifting or carrying and lumbar disc herniation.
The level of lumbar disc prolapse was at L4-L5 for more than half of studied patients (56.7%). This finding is close to results of Musharbash A, et al. study in Jordan (2009) [21] which recorded that common level lumbar disc prolapse were at L4-L5 (54.6%). The L4-L5 and L5-S1 are the two lowest levels in the lumbar spine, and together with the attached disc, joints, nerves and soft tissues, it provides a variety of functions, including supporting the upper body and allowing motion in multiple directions. However, with its heavy load and range of flexibility, these segments are also prone to developing pain from injury and/or from degenerative changes.
The main symptoms of studied patients pre-operatively were leg pain, leg parathesia, back pain and muscle weakness with mean duration of symptoms as 10 ± 9 weeks. Khattak AU, et al. study in Pakistan (2009) [22] reported duration of symptom as 6 weeks - 1 year. This difference might be attributed to that our patients have less tolerance for pain. Pre-operatively two thirds (76.7%) of the lumbar disc prolapse patients were at grade 3 and 4 of EHL grading but with better FHL grading (63.3%). Postacchini F, et al. study in Italy (2002) reported close findings to our study regarding pre-operative symptoms and EHL grading for Lumbar disc prolapse patients (80%) undergoing Minimal Invasive Discectomy (MID) [23] .
The intra-operative complication for studied patients was epidural bleeding only for four patients. No dural tear and nerve root injury detected for patients undergone MID in our study. This finding is consistent with results of Grag B, et al. study in India (2011) [10] and Lee YG, et al. study in South Korea (2010) [24] which reported the epidural bleeding as intraoperative complication of MID. On other hand, Chang SS, et al. study in Taiwan (2009) [25] and Khattak AU, et al. study in Pakistan (2009) [22] reported cases with dural tear and nerve root injuries as intraoperative complications.
One month post-operatively, twenty five patients had no leg pain, no patients had leg parathesia and infection except back pain as it was present among 63.3% of them. These results are close to results of Dasenbrock HH, et al. study in USA (2012) [26] which concluded that MID for patients with lumbar disc prolapse led to improvement in leg pain and parathesia. Lumbar disc herniation associated with back pain is often related to disc degeneration and back pain after minimal invasive discectomy often persists [26] . Our results reported reduction of patients with back pain (36.7%) that is close to results of Maida G, et al. study in Italy (2014) [27] which concluded that 44.4% of the patient undergoing MID had improvement in back pain.
Post-operatively majority of the studied patient were at grade 4 and 5 for muscle strength grading (EHL & FHL). This finding is consistent with results of Postacchini F, et al. study in Italy (2002) [23] which concluded a complete recovery of muscle strength in 91% (106) of the patients.
The present study revealed significant improvement in symptoms (leg pain, leg parathesia and back pain) and muscle strength (EHL & FHL grading) of lumbar disc prolapse patients two months after Minimal Invasive discectomy (p < 0.001). This finding is consistent with results of Gibson AJN, et al. study in Netherlands (2012) [15] , Blamoutier A study in France (2013) [16] and Majeed SA, et al. in India (2013) [18] .
6. Conclusions
・ Minimal invasive discectomy is a good treatment option for lumbar disc prolapse.
・ Minimal invasive discectomy is associated with low rate of complications, and a little tissue damage.
・ Although significant reduction of back pain after MID, more than half of patients still present back pain post-operatively.
7. Recommendations
・ Encouraging and supporting treatment of lumbar disc prolapse patients with minimal invasive discectomy.
・ Emphasis on training courses of MID on animals and cadavers for spinal and orthopedic surgeons.
・ Further large sized studies on efficacy and safety of MID should be supported.
Cite this paper
Hamid A. Jaff,Bakhtyar Rasul M. Amin,Rebar M. Noori Fatah,Hosam H. Husein, (2016) The Outcome of Minimally Invasive Discectomy in Single Level Lumbar Disc Prolapse. Open Journal of Orthopedics,06,211-220. doi: 10.4236/ojo.2016.67028
References
- 1. Chang, S.S., Fu, T.S., Liang, Y.C., Lai, P.L., Niu, C.C., Chen, L.H., et al. (2009) Results of Microendoscopic Discectomy Performed in the 26 Cases with a Minimum 3 Years Follow-Up. Chang Gung Medical Journal, 32, 89-97.
- 2. Dasenbrock, H.H., Witham, T.F., Juraschek, S.P., Sciubba, D.M., Schultz, L.R., Wolinsky, J.P., et al. (2012) The Efficacy of Minimally Invasive Discectomy Compared with Open Discectomy: A Meta-Analysis of Prospective Randomized Controlled Trials. Journal of Neurosurgery: Spine, 16, 452-462.
http://dx.doi.org/10.3171/2012.1.SPINE11404 - 3. Maida, G., Altruda, C., Gatti, M., Saletti, A., Borrelli, M. and Sarubbo, S. (2014) Two-Year Follow-Up after Microsurgical Discectomy and Dynamic Percutaneous Stabilization in Degenerate and Herniated Lumbar Disc: Clinical and Neuroradiological Outcome. Journal of Neurosurgical Sciences, 58, 95-102.
- 4. Lee, Y.G., Cha, J.H. and Park, J.S. (2010) Clinical Outcome of Minimally Invasive Tubular Retractor Assisted Microscopic Discectomy in Far Lateral Lumbar Disc Herniation. Korean Journal of Spine, 7, 155-160.
- 5. Postacchini, F., Giannicola, G. and Cinotti, G. (2002) Recovery of Motor Deficits after Microdiscectomy for Lumbar Disc Herniation. Journal of Bone and Joint Surgery [Br], 84, 1040-1045.
http://dx.doi.org/10.1302/0301-620X.84B7.12948 - 6. Khattak, A.U., Haider, A., Rehman, L. and Mushtaq, I. (2009) Surgical Outcome of Recurrent Lumbar Disc Herniation: Experience with 30 Patients. JPMI, 23, 86-89.
- 7. Musharbash, A., Saleh, Q., Abo-Elrub, M. and Maani, W. (2009) Management of Lumbar Far Lateral Disc Herniation: Clinical Study. Pan Arab Journal of Neurosurgery, 13, 28-30.
- 8. Seidler, A., Bolm-Audorff, U., Siol, T., Fuchs, C., Henkel, N., Schug, H., et al. (2003) Occupational Risk Factors for Symptomatic Lumbar Disc Herniation: A Case-Control Study. Occupational and Environmental Medicine, 60, 821-830.
http://dx.doi.org/10.1136/oem.60.11.821 - 9. German, J.W., Adamo, M.A., Hoppenot, R.G., et al. (2008) Perioperative Results Following Lumbar Discectomy: Comparison of Minimally Invasive Discectomy and Standard Microdiscectomy. Neurosurgical Focus, 25, E20.
http://dx.doi.org/10.3171/foc/2008/25/8/e20 - 10. Majeed, S.A., Vikraman, C.S., Mathew, V. and Anish, T.S. (2013) Comparison of Outcomes between Conventional Lumbar Fenestration Discectomy and Minimally Invasive Lumbar Discectomy: An Observational Study with a Minimum 2-Year Follow-Up. Journal of Orthopaedic Surgery and Research, 8, 34.
http://www.josr-online.com/content/8/1/34
http://dx.doi.org/10.1186/1749-799X-8-34 - 11. Vigasio, A., Marcoccio, I., Patelli, A., Mattiuzzo, V. and Prestini, G. (2008) New Tendon Transfer for Correction of Drop-Foot in Common Peroneal Nerve Palsy. Clinical Orthopaedics and Related Research, 466, 1454-1466.
http://dx.doi.org/10.1007/s11999-008-0249-9 - 12. Blamoutier, A. (2013) Surgical Discectomy for Lumbar Disc Herniation: Surgical Techniques. Orthopaedics & Traumatology: Surgery & Research, 99, S187-S196.
http://dx.doi.org/10.1016/j.otsr.2012.11.005 - 13. Gibson, J. and Waddell, G. (2007) Surgical Interventions for Lumbar Disc Prolapse. Cochrane Database of Systematic Reviews, 2007, CD001350.
http://dx.doi.org/10.1097/brs.0b013e3180bc2431 - 14. Osterman, H., Seitsalo, S., Karppinen, J., et al. (2006) Effectiveness of Microdiscectomy for Lumbar Disc Herniation: A Randomized Controlled Trial with 2 Years of Follow-Up. Spine (Phila Pa 1976), 31, 2409-2414.
http://dx.doi.org/10.1097/01.brs.0000239178.08796.52 - 15. McGirt, M.J. (2009) A Prospective Cohort Study of Close Interval Computed Tomography and Magnetic Resonance Imaging after Primary Lumbar Discectomy: Factors Associated with Recurrent Disc Herniation and Disc Height Loss. Spine, 34, 2044-2051.
http://dx.doi.org/10.1097/BRS.0b013e3181b34a9a - 16. Porchet, F., Bartanusz, V. and Kleinstueck, F.S. (2009) Microdiscectomy Compared with Standard Discectomy: An Old Problem Revisited with New Outcome Measures within the Framework of a Spine Surgical Registry. European Spine Journal, 3, 360-366.
http://dx.doi.org/10.1007/s00586-009-0917-9 - 17. Ranjan, A. and Lath, R. (2006) Microendoscopic Discectomy for Prolapsed Lumbar Intervertebral Disc. Neurology India, 54, 190-194.
- 18. Garg, B., Nagraja, U.B. and Jayaswal, A. (2011) Microendoscopic versus Open Discectomy for Lumbar Disc Herniation: A Prospective Randomised Study. Journal of Orthopaedic Surgery, 19, 30-34.
- 19. Righesso, O., Falavigna, A. and Avanzi, O. (2007) Comparison of Open Discectomy with Microendoscopic Discectomy in Lumbar Disc Herniations: Results of a Randomized Controlled Trial. Neurosurgery, 61, 545-549.
http://dx.doi.org/10.1227/01.NEU.0000290901.00320.F5 - 20. Chi, J.H., Dhall, S.S., Kanter, A.S., et al. (2008) The Mini-Open Transpedicular Thoracic Discectomy: Surgical Technique and Assessment. Neurosurgical Focus, 25, E5.
http://dx.doi.org/10.3171/FOC/2008/25/8/E5 - 21. German, J.W., Adamo, M.A., Hoppenot, R.G., et al. (2008) Perioperative Results Following Lumbar Discectomy: Comparison of Minimally Invasive Discectomy and Standard Microdiscectomy. Neurosurgical Focus, 25, E20.
http://dx.doi.org/10.3171/foc/2008/25/8/e20 - 22. Osterman, H., Seitsalo, S., Karppinen, J., et al. (2006) Effectiveness of Microdiscectomy for Lumbar Disc Herniation: A Randomized Controlled Trial with 2 Years of Follow-Up. Spine (Phila Pa 1976), 31, 2409-2414.
http://dx.doi.org/10.1097/01.brs.0000239178.08796.52 - 23. Peul, W.C., van Houwelingen, H.C., van den Hout, W.B., et al. (2007) Surgery versus Prolonged Conservative Treatment for Sciatica. New England Journal of Medicine, 356, 2245-2256.
http://dx.doi.org/10.1056/NEJMoa064039 - 24. Arts, M.P. and Peul, W.C. (2011) Leiden—The Hague Spine Intervention Prognostic Study Group (SIPS). Timing and Minimal Access Surgery for Sciatica: A Summary of Two Randomized Trials. Acta Neurochirurgica, 153, 967-974.
http://dx.doi.org/10.1007/s00701-011-0983-8 - 25. Konstantinou, K. and Dunn, K.M. (2008) Sciatica: Review of Epidemiological Studies and Prevalence Estimates. Spine, 33, 2464-2472.
http://dx.doi.org/10.1097/BRS.0b013e318183a4a2 - 26. Weinstein, J.N., Lurie, J.D., Tosteson, T.D., Tosteson, A.N., Blood, E.A., Abdu, W.A., et al. (2008) Surgical versus Nonoperative Treatment for Lumbar Disc Herniation: Four-Year Results for the Spine Patient Outcomes Research Trial (SPORT). Spine, 33, 2789-2800.
http://dx.doi.org/10.1097/BRS.0b013e31818ed8f4 - 27. Katz, J.N. (2006) Lumbar Disc Disorders and Low-Back Pain: Socioeconomic Factors and Consequences. Journal of Bone and Joint Surgery, 88, 21-24.
http://dx.doi.org/10.2106/JBJS.E.01273