Open Journal of Orthopedics
Vol.3 No.2(2013), Article ID:32710,2 pages DOI:10.4236/ojo.2013.32015
Transmedullary Decompression for Humeral Diaphysis Solitary Bone Cysts
![]()
Department of Orthopaedic Surgery, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan.
Email: akio@med.kyushu-u.ac.jp
Copyright © 2013 Akio Sakamoto. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 23rd, 2013; revised May 2nd, 2013; accepted May 20th, 2013
Keywords: Transmedullary; Treatment; Humerus; Solitary Bone Cyst
ABSTRACT
Solitary bone cysts are benign, fluid-filled cavities that most often occur in childhood. Several minimally invasive decompression methods have been proposed; however, performing a surgical procedure through the thinned overlying cortex raises the risk of pathological fracture and neurovascular damage, especially in lesions located in the bone diaphysis. We describe a new technique that circumvents these problems: tunneling through the normal cortex and medullary space with a flexible reamer, placing a retrograde medullary nail for cyst decompression.
1. Summary
Solitary bone cysts are benign, fluid-filled cavities that most often occur in childhood. Several minimally invasive decompression methods have been proposed; however, performing a surgical procedure through the thinned overlying cortex raises the risk of pathological fracture and neurovascular damage, especially in lesions located in the bone diaphysis. We describe a new technique that circumvents these problems: tunneling through the normal cortex and medullary space with a flexible reamer, placing a retrograde medullary nail for cyst decompression.
2. Introduction
Solitary bone cysts occur most often in childhood, and these fluid-filled lesions are benign [1]. When located in the long bones, solitary bone cysts appear on radiography as radiolucent lesions with a thinned overlying cortex (Figure 1(a)); this thinned cortex can result in subsequent pathologic fracture [2]. Magnetic resonance imaging with gadolinium enhancement confirms the cystic nature of the lesion (Figures 1(b)-(d)). The etiology of solitary bone cysts is unknown, but one hypothesis purports that the mechanism involves venous obstruction with subsequent elevated intra-osseous pressure, leading to cyst formation [3]. These cysts commonly occur in the metaphyseal regions of the long bones, particularly in the proximal femur and the proximal humerus [2]. The activity of a solitary bone cyst can be predicted by its distance from the growth plate. A cyst, which is distant from the growth plate and is the so-called latent type, is assumed to have a lower rate of recurrence after treatment than active-type cysts which are closer to the epiphyseal plate. Because the development of the cyst is faster than the growth of the bone [4,5], solitary bone cysts seldom heal without treatment [4]. Over the course of long-bone development, persistent cystic lesions come to be located at the diaphysis in young adults.
Several minimally invasive methods for the treatment of solitary bone cysts have been proposed, including cortical decompression, percutaneous medicalgrade calcium sulfate grafting, autogenous bone marrow injection, and steroid injection [6,7]. Cortical decompression consists of inserting a screw, or performing an injection, through the thinned cortex; it carries the risk of pathological fracture and refraining from sporting activity is necessary after this procedure. The surgical approach to a solitary bone cyst in the diaphysis of the humerus also risks causing neurovascular damage. To avoid the potential complications of fracture and neurovascular damage, we propose the technique of performing decompression via the normal cortex at the distal humerus, using a flexible reamer for placement of a retrograde medullary nail into the cyst (Figure 1(e)).
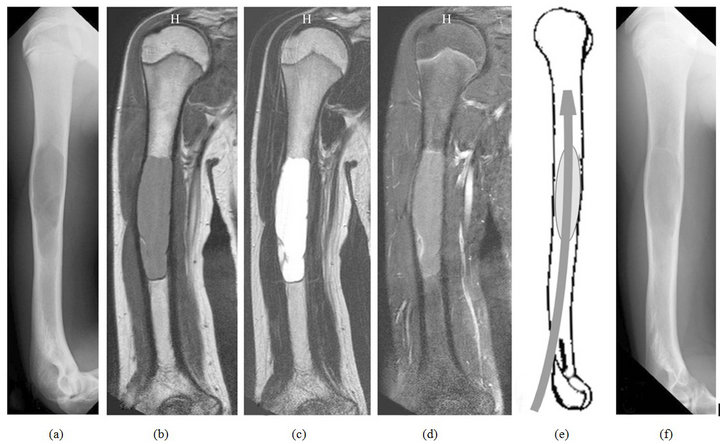
Figure 1. Solitary bone cyst of the humerus in a 15-year-old boy. A plain radiography shows a radiolucent lesion with a thinned cortex in the diaphysis of the humerus (a); Magnetic resonance imaging shows a medullary lesion with low signal intensity on T1-weighted images (b); and high signal intensity on T2-weighted images (c); Gadolinium enhancement is seen at the periphery of the lesion on T1-weighted fat-suppression imaging (d); Schematic of transmedullary cyst drainage (e); A plain radiopraph 3 months after the procedure shows bone formation (f).
3. Technique and Discussion
The ligamentous portion of the distal triceps muscle is split. A hole is drilled in the bone cortex and a 6 mm flexible reamer is used to tunnel through the medullary space until the cyst is reached; this is performed under roentgenoscopic guidance. The diagnosis is confirmed by the drainage of serous liquid. Sporting activities can be resumed after the elbow pain resolved. This technique provides continuity of the cyst with the adjacent bone marrow space, allowing bone marrow cells to enter the cyst and resulting in the accelerated bone incorporation. In addition, the reamed bone marrow space adjacent to the cyst allows for cyst decompression (Figure 1(f)).
4. Acknowledgements
The author declares no competing interests.
REFERENCES
- A. R. Goel, J. Kriger, R. Bronfman and E. Lauf, “Unicameralbone Cysts: Treatment with Methylprednisone Acetate
- Injections,” Journal of Foot and Ankle Surgery, Vol. 33, No. 1, 1994, pp. 6-15.
- H. D. Dorfman and B. Czerniak, “Bone Tumors,” Mosby St Louis, 1998.
- J. Cohen, “Etiology of Simple Bone Cyst,” The Journal of Bone & Joint Surgery, Vol. 52, No. 7, 1970, pp. 1493- 1497.
- C. S. Neer 2nd, K. C. Francis, R. C. Marcove, J. Terz and P. N. Carbonara, “Treatment of Unicameral Bone Cyst. A Follow-Up Study of One Hundred Seventy-Five Cases,” The Journal of Bone & Joint Surgery, Vol. 48, No. 4, 1966, pp. 731-745.
- P. L. Docquier and C. Delloye, “Treatment of Simple Bone Cysts with Aspiration and a Single Bone Marrow Injection,” Journal of Pediatric Orthopaedics, Vol. 23, No. 6, 2003, pp. 766-773. doi:10.1097/01241398-200311000-00015
- H. S. Cho, J. H. Oh, H. S. Kim, H. G. Kang and S. H. Lee, “Unicameral Bone Cysts: A Comparison of Injection of Steroid and Grafting with Autologous Bone Marrow,” The Journal of Bone & Joint Surgery, Vol. 89, No. 2, 2007, pp. 222-226. doi:10.1302/0301-620X.89B2.18116
- J. G. Wright, S. Yandow, S. Donaldson and L. Marley (Simple Bone Cyst Trial Group), “A Randomized Clinical Trial Comparing Intralesional Bone Marrow and Steroid Injections for Simple Bone Cysts,” The Journal of Bone & Joint Surgery, Vol. 90, No. 4, 2008, pp. 722-730. doi:10.2106/JBJS.G.00620

