World Journal of Cardiovascular Diseases
Vol.09 No.01(2019), Article ID:90235,9 pages
10.4236/wjcd.2019.91005
Prognostic Factors for Acute Heart Failure (AHF) in the Cardiology Intensive Care Unit (ICU) of the University Hospital Point G (UH Pt G)
Camara Youssouf1*, Ba Hamidou Oumar2, Sangare Ibrahima2, Toure Karamba1, Coulibaly Souleymane3, Sacko Abdoul Karim3, Coulibaly Alfousseyni1, Diallo Nouhoum3, Sidibe Samba3, Daou Adama4, Menta Ichaka2, Diall Ilo Bella3, Diallo Boubakar Abdoulaye3
1University Hospital Sidy Bocar Sall, Kati, Mali
2University Hospital Gabriel Touré, Bamako, Mali
3University Hospital Point G, Bamako, Mali
4Disease Fighting Centers, Bamako, Mali
Copyright © 2019 by author(s) and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: January 2, 2019; Accepted: January 25, 2019; Published: January 28, 2019
ABSTRACT
Background and Aim: The absence of data in our context motivates this study aiming to determine the frequency of AHF at the ICU, assess the in-hospital evolution of the disease and to find out poor prognosis. Material and Methods: It was an observational and descriptive study covering the time from January 1, 2014 to March 30, 2017 involving all inpatient records in ICU. From January 2014 to December 2017, collected data included those on socio-demographic, history of diseases and physical examination, and some labor data including Pro BNP, serum creatinine, blood ionogram, cardiac enzymes and blood count. Also data electrocardiography, echocardiography and in-hospital evolution were collected. Statistical Analysis: Statistical analysis was performed using SPSS (IBM Inc) version 18. Results: AHF occured in 47.36% with a mean age of 58.74 ± 18.407 and extremes of 17 and 90 years, women representing 53.1% (sex ratio Male:Female = 0.88). Hypertension and diabetes were the predominant cardiovascular risk factors with respectively 67.4% and 18.4%. At admission 44%, 37.7% and 17.9% of patients were respectively hypertensive, normotensive and hypotensive. The clinical expression was mainly global heart failure with 42.6% followed by left heart failure and right heart failure with respectively 37% and 20.4%. The coronary syndromes (all forms) was the first cause of ICA with 34% of cases followed by pulmonary embolism and hypertension with respectively 25.3% and 24.1%. Mean hospital stay was 5.61 ± 3.527 days (1 to 25 days). Complications were recorded in 18.5% of patients with cardiogenic shock in half of all cases. In multi-variate analysis, only hypotension at admission was shown to be the independent factor of poor prognosis with p = 0.016 and OR = 4.453 (1.322 - 14.996). Conclusion: As a common manifestation heart failure can be rapidly fatal in presence of collapsus or hypotension at admission. These factors should be accurately managed to reduce mortality, which remains high in our context.
Keywords:
Acute Heart Failure, Prognostic Factors, Cardiology, Intensive Care Unit, Bamako

1. Introduction
Acute heart failure (AHF) refers to the rapid onset or worsening of symptoms or signs of heart failure [1] . It represents more than 20 million hospitalizations worldwide [2] and can be either “de novo” or most often due to the acute decompensation of chronic heart failure [1] . Heart failure can be classified in different ways, left or right sided, with altered or preserved ejection fraction, acute or chronic.
AHF accounts for 1 million hospitalizations in the United States [2] , 1876 hospitalizations in a study in Japan [3] and 67,000 hospitalizations in Great Britain and Wales [4] .
AHF also causes high morbidity and mortality. In-hospital mortality in Europe is estimated between 4% and 7% [5] , 45% and 13% for 95th percentile respectively in Senegal and Nigeria in 2001 [6] and the average survival rate at 5 years is 50% [4] .
There is an absence of published data in our context, motivating this study which aims to determine the frequency of AHF at the ICU, assess the in-hospital evolution of the disease and find out which factors lead to poor prognosis.
2. Material and Methods
It was an observational and descriptive study covering the time from January 01, 2014 to March 30, 2017 involving all inpatient records in ICU. The sampling was exhaustive, including all patients admitted for AHF in the ICU oft he UH Pt G and excluding those admitted in ICU for others conditions.
Collected data included those on:
- socio-demographic characteristics: age, sex, occupation, residence.
- past medical history and cardiovascular risk factors.
- history of the disease: onset of symptoms, functional signs (dyspnea stage III or IV NYHA, chest pain).
- physical examination: measures of blood pressure, search for clinical signs of heart failure (left, right).
- labor data: Pro BNP, serum creatinine, blood ionogram, cardiac enzymes, blood cell count.
- electrocardiography: presence of atrial fibrillation, high-grade atrioventricular block, signs of myocardial ischemia.
- echocardiography: measurement of chambers size, evaluation of wall motion, systolic function of both left and right ventricles, significant valvular diseases (at least grade III), evaluation of filling pressures of the Left ventricle, pulmonary arterial pressure, evaluation of pericardial effusion.
- chest computer tomogramm in cases of pulmonary embolism suspicion for occlusion of the pulmonary artery.
- in-hospital evolution.
These data were collected on an anonymous survey formulary and then inserted into an EPI INFO 7 (CDC Atlanta) database.
Ethical Consideration: confidentiality rules were respected throughout the study.
Statistical Analysis was performed using SPSS (IBM Inc) version 18. The chi-square and Fisher-tests for small numbers were the tests used for statistical analysis.
3. Results
Description of the Sample
During the study period 162 patients of 342 were admitted for AHF (47.36%) with an average age of 58.74 ± 18.407 ranging from 17 to 90 years. The modal class was 50 - 75 years with 51.23% (Table 1). A proportion of 76 men for 86 women constituted the sample, giving a sex ratio Male: Female of 0.88 (Table 1).
Heart failure was found in the past medical history in 16.7% and hypertenion was the most frequent cardiovascularrisk factor with 67.4%, followed by diabetes (18.4%) (Table 2).
Patients had hypotension at admission in 17.9%, hypertension in 44.4% and normal blood pressure in 37.7% of cases.
According to the location, global heart failure (GHF) (left + right sided) was the most frequent form with 42.6% followed by left heart failure (LHF) in 37% of cases and right heart failure (RHF) in 20.4% of patients (Diagram 1).
In echocardiography LVEF was normal in 43% and severely reduced in 24% of all cases (Diagram 2).
Acute coronary syndrome (ACS) was the leading cause of AHF with 34% of all cases followed by pulmonary embolism and hypertension with respectively 25.3% and 24.1% (Table 3).
Mean hospital stay was 5.61 ± 3.527 days ranging from 1 to 25 days. A proportion of 36.6% stayed more than 7 days.
Cardiogenic shock was the most common complication (9.25%) followed by electrolyte disorders (Table 4).
Mortality and factors of poor prognosis:
Table 1. Socio-demographic data in the sample of 162 patients admitted for AHF in the ICU of the UH Pt G.
Table 2. Medical history and cardiovascular risk factors in the sample of 162 patients admitted for AHF in the ICU of the UH Pt G.
Table 3. Distribtion of etiologies in the sample of 162 patients admitted for AHF in the ICU of the UH Pt G.
Table 4. In-hospital evolution in the sample of 162 patients admitted for AHF in the ICU of the UH Pt G.
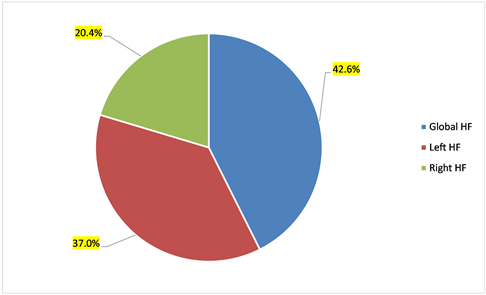
Diagram 1. Type of heart failure in the sample of 162 patients admitted for AHF in the ICU of the UH Pt G.

Diagram 2. Répartition of left ventricular fonction at admission in the sample of 79 patients admitted for AHF in the ICU of the UH Pt G.
Overall in-hospital mortality was 32.09%. Female mortality appeared to be higher than that of men (33.7% versus 30.3% ) but without statistical difference, p = 0.63. Patients over 75 years and under 50 years had the highest in-hospital mortality rate but without any statistical difference, p = 0.70 (Table 5).
Having a history of heart failure was statistically (p = 0.02) associated with high mortality with 51.9% specific mortality. The GHF mortality (39.1%) was statistically higher than that of RHF (p = 0.01) and also higher than that of LHF (p = 0.03). Mortality due to the presence of arterial hypotension or cardiogenic shock (67.85%) at admission was statistically higher compared with normal or elevated blood pressure, p < 0.0001. The existence of a severely impaired left ventricular ejection fraction was a poor prognostic factor with a mortality of 63.2%; p = 0.002 (Table 5).
The most fatal complication was cardiogenic shock with a specific mortality of 93.33%, p = 0.008.
ACS was the most fatal etiology with 38.46% (p = 0.12) (Table 5).
In logistic regression, only a state of collapse or arterial hypotension at admission was found to be the independent poor prognostic factor with p = 0.016 and OR = 4.453 (1.322 - 14.996) (Table 6).
The level of the systolic ejection fraction could not be analyzed in logistic regression because of the low proportion (48.8%) of patients who received echocardiography.
Table 5. Distribution of mortality according to various pronostic factors in the sample of 162 patients admitted for AHF in the ICU of the UH Pt G.
Table 6. Prognostic factors of AHF in the ICU of the UH Pt G.
4. Discussion
4.1. Age
The mean age in our study was 58.73 ± 18.407, less than the 69.9 ± 12.5 of the EHF-II [5] [7] study and the 72 ± 14.1 of ADHERE [5] [8] . This could be explained by the fact that the African population is much younger than the European and American population. However, we found higher mean age compared to DAMASCENO (52.3 ± 18.3) [9] . This difference could be explained by the small size of our sample.
4.2. Sex
In our serie, females predominated with 53.1% in agreement with Damasceno [9] , prasart [10] and the adhere study [5] [7] [8] with respectively 52%, 50.8% and 50.4%. in contrary there were less female as reported by the EHFS-II study [5] [7] where women accounted for only 39%, possibly related to the post-surgical nature of this study.
4.3. Past Medical History and Cardiovascular Risk Factors
Only 16.7% of our patients had already heart failure compared to 66.5% for prasart [10] , 75% for dimitrios [7] and 63% for Nieminen [5] . This could be explained by the difference in level of health education of the population on the one hand and the performance of health systems in these countries on the other.
Hypertension with 67.4% was the most cardiovascular risk factor found in our study as reported in the literature [5] [7] [8] [9] [10] .
4.4. Etiology
As found in the literature [6] - [12] , coronary syndrome and arterial hypertension were the leading causes of AHF with respectively 41.5% and 17.3%.
4.5. Evolution and In-Hospital Mortality
In our serie, the in-hospital mortality of 32.1% was significantly higher than that found in the literature [5] [7] [8] [10] [11] [12] [13] , due in part to a situation with less equipment/less financial resources also for patients leading to long delay before starting management.
4.6. Factors of Poor Prognostic
Many factors have been identified as prognostic factors such: BUN (cutoff value of 43 mg/dl), systolic blood pressure (cutoff value of 115 mmHg and serum creatinine (cutoff value of 2.75 mg/dl) in ADHERE registry [14] or patient age, systolic blood pressure, respiratory rate, serum sodium, hemoglobin, BUN and medical history of cerebrovascular disease, dementia, liver cirrhosis or cancer [15] .
In bivariate analysis, we were able to identify factors with high mortality/poor prognostic: a past history of heart failure, GHF, collapse or hypotension at admission, severely impaired left ventricular ejection fraction and finally, the occurrence during the hospitalization of a cardiogenic shock.
After logistic regression, only collapse/hypotension at admission was the independent factor of poor prognostic with p = 0.016 and OR = 4.453 (1.322 - 14.996).
4.7. Limits of the Study
Main limit was the availability of echocardiography for all patients. We further were not able to check all patients for labor data such as Pro-BNP, then we know from the literature that there are some biological marker for prognotic. Despite these limits our study provides valueble informations about AHF in a ressource limited environment.
5. Conclusion
AHF is a common manifestation of heart failure that can be rapidly fatal. The clinical manifestation is noisy but quickly resolute under the adapted treatment. Identifying poor prognostic factors like collapse/hypotension in our study is essential to reduce mortality.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
Cite this paper
Youssouf, C., Oumar, B.H., Ibrahima, S., Karamba, T., Souleymane, C., Karim, S.A., Alfousseyni, C., Nouhoum, D., Samba, S., Adama, D., Ichaka, M., Bella, D.I. and Abdoulaye, D.B. (2019) Prognostic Factors for Acute Heart Failure (AHF) in the Cardiology Intensive Care Unit (ICU) of the University Hospital Point G (UH Pt G). World Journal of Cardiovascular Diseases, 9, 42-50. https://doi.org/10.4236/wjcd.2019.91005
References
- 1. Ponikowski, P., Voors, A.A., Anker, S.D., et al. (2016) ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. European Heart Journal, 37, 2129-2200. https://doi.org/10.1093/eurheartj/ehw128
- 2. Ziaeian, B., Sharma, P.P., et al. (2015) Factors Associated with Heart Rate Changes in the United States. American Heart Journal, 169, 282-289. https://doi.org/10.1016/j.ahj.2014.11.007
- 3. Shiraishi, Y., Kohsaka, A., Abe, T., et al. (2014) Validation of the Patient with the Guideline Heart Failure Risk in Japanese Patients and the Potential for Improvement of Its Discrimination by the Inclusion of B-Type Natriuretic Peptide Level. Heart, 100, 115-125.
- 4. National Institute for Health and Care Excellence (2014) Acute Heart Failure: Diagnosing and Managing. Heart Failure in Adults (Clinical Guideline CG187). https://www.nice.org.uk/guidance/cg187
- 5. Nieminen, M.S., Brutsaert, D., Dickstein, K., et al. (2006) EuroHeart Failure Survey II (EHFS II): A Survey on Hospitalized Acute Heart Failure Patients: Description of Population. European Heart Journal, 27, 2725-2736. https://doi.org/10.1093/eurheartj/ehl193
- 6. Callender, T., Woodward, M., Roth, G., Farzadfar, F., Lemarie, J.-C., et al. (2014) Heart Failure Care in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. PLoS Medicine, 11, e1001699.
- 7. Farmakis, D., Parissis, J., Lekakis, J. and Filippatos, G. (2015) Acute Heart Failure: Epidemiology, Risk Factors, and Prevention. Revista Espanola de Cardiología, 68, 245-248. https://doi.org/10.1016/j.recesp.2014.11.009
- 8. Adams, K.F., Fonarow, G.C., Emerman, C.L., LeJemtel, T.H., Costanzo, M.R., Abraham, W.T., et al., ADHERE Scientific Advisory Committee and Investigators (2005) Characteristics and Outcomes of Patients Hospitalized for Heart Failure in the United States: Rationale, Design, and Preliminary Observations from the First 100,000 Cases in the Acute Decompensated Heart Failure National Registry (ADHERE). American Heart Journal, 149, 209-216.
- 9. Damasceno, A., Mayosi, B.M., et al. (2012) The Causes, Treatment, and Outcome of Acute Heart Failure in 1006 Africans From 9 Countries. Archives of Internal Medicine, 172, 1386-1394. https://doi.org/10.1001/archinternmed.2012.3310
- 10. Laothavorn, P., Hengrussamee, K. and Kanjanavanit, R. (2010) Thai Acute Decompensated Heart Failure Registry (Thai ADHERE). CVD Prevention and Control, 5, 89-95. https://doi.org/10.1016/j.cvdpc.2010.06.001
- 11. Farmakis, D., Parissis, J., Lekakis, J. and Filippatos, G. (2015) Acute Heart Failure: Epidemiology, Risk Factors, and Prevention. Revista Espanola de Cardiología, 68, 245-248. https://doi.org/10.1016/j.recesp.2014.11.009
- 12. Dang, D., Delmas, C., Espinasseau, G., Huo Yung Kai, S., Milhau-Bacharach, S., Beddok, R. and Elbaz, M. (2016) Epidemiology of Acute Cardiac Failure in Cahors (ICAhors) with Analysis of Predictive Factors for a New Hospitalization in the Year for Acute Heart Failure. Annals of Cardiology and Angiology, 65, 375-381.
- 13. Ray, P., Bennaceur, M., Zhao, Y. and Riou, B. (2004) Acute Heart Failure (ICA) of the Elderly Subject in Emergencies. European Journal of Emergencies, 17, 128-131.
- 14. Fonarow, G.C., Adams, K.F., Abraham, W.T., et al. (2005) Risk Stratification for In-Hospital Mortality in Acutcly Decompcnsated Heart Failure Classification and Regression Tree Analysis. JAMA, 293, 572-580. https://doi.org/10.1001/jama.293.5.572
- 15. Lee, D.S., Austin, P.C., Rouleau, J.L., et al. (2003) Predictlng Mortality among Patients Hospitalized for Heart Failure: Derivation and Validation of a Clinical Model. JAMA, 290, 2581-2587. https://doi.org/10.1001/jama.290.19.2581


