Open Journal of Stomatology
Vol.3 No.1(2013), Article ID:28734,3 pages DOI:10.4236/ojst.2013.31005
Oral manifestations of acute promyelocytic leukemia: A case report
![]()
1Division of Reconstructive Surgery for Oral and Maxillofacial Region, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan
2Division of Oral and Maxillofacial Surgery, Yukiguni Yamato Hospital, Minamiuonuma City, Japan
Email: tadaharu@dent.niigata-u.ac.jp
Received 18 January 2013; revised 20 February 2013; accepted 28 February 2013
Keywords: Acute Promyelocytic Leukemia; Oral Manifestations; Oral Care
ABSTRACT
Acute leukemia is often associated with oral manifestations. We report an acute promyelocytic leukemia (APL) case with oral manifestations leading to the diagnosis. A 21-year-old female visited our hospital with complaints of gingival bleeding and swelling of the left lower wisdom tooth. The patient’s complete blood count revealed a marked increase in white blood cells and a decrease in red blood cells and an abnormal leukocyte differential, and APL was diagnosed on the basis of bone marrow samples in the internal medicine department. The patient was treated with all-trans-retinoic acid combined with chemotherapy and has maintained clinical and molecular complete remission at 12 months of follow-up. Dental professionals should be aware of clinical manifestations and complications associated with these malignnant neoplastic diseases to aid in diagnosis and subsequent treatment and management.
1. INTRODUCTION
Leukemia is a hematological disorder that is caused by an abnormal increase of immature white blood cells and is often associated with oral manifestations such as mucosal pallor, ecchymoses, bleeding, ulceration, gingival enlargement, trismus, mental nerve neuropathy, facial palsy, and infections [1-12]. Acute promyelocytic leukemia (APL) is a subtype of acute myeloid leukemia (AML), and early detectionof APL is important because of the high risk of early death due to severe hemorrhagic events [13].
In this paper, an APL case with gingival bleeding and pericoronitis as initial manifestations leading to the diagnosis is described.
2. CASE REPORT
A 21-year-old female visited our hospital with the complaint of gingival bleeding when tooth brushing over the past several weeks and complaints of pain and swelling of the left lower wisdom tooth over the past few days. She had previously undergone ventricular shunting and midfacial and orbital advancement procedures for Crouzon disease.
Physical examination revealed that the patient had pallor, fatigue, body temperature of 37.9 degrees C, swelling of the lower left cheek, ecchymoses of the forearm and lower leg (Figure 1(a)), and trismus and pericoronitis of the left lower wisdom tooth (Figure 1(b)). There was no gingival enlarge mentor local abnormal color.
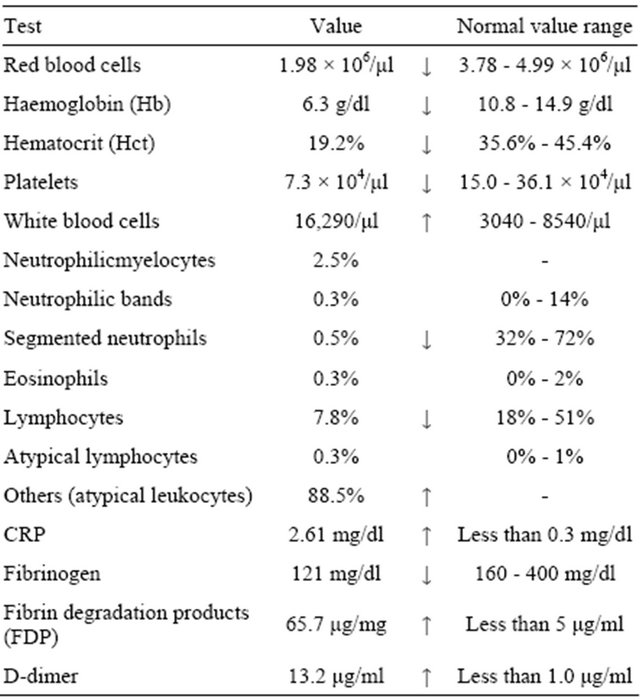
The patient’s complete blood count (CBC) (Table 1) revealed a marked increase in white blood cells and a decrease in red blood cells with anisocytosis, poikilocytes and erythroblasts and lowered hematocrit, hemoglobin and platelet count. The abnormal leukocyte differential displayed 2.5% neutrophilicmyelocytes, 0.3% neutrophilic bands, 0.5% segmented neutrophils, 0.3% eosinophils, 7.8% lymphocytes, 0.3% atypical lymphocytes and 88.5% others (atypical leukocytes). The patient was referred to internal medicine, where M3-APL according to the FAB criteria was diagnosed on the basis of bone marrow samples that showed hypercellularity with abnormal promyelocytes (Figure 2) and chromosomal translocation t(15,17) confirmed by fluorescence in situ hybridization (FISH). Moreover, the patient was diagnosed as having disseminated intravascular coagulation (DIC) from lowered fibrinogen and raised fibrin degradation products (FDP) and D-dimer (Table 1).
The patient was treated with all-trans-retinoic acid (ATRA) at 45 mg/m2/day per oral as differentiation- inducing therapy and intravenous nafamostatmesilate for DIC starting on day 2. Cytarabine (Ara-C, 100 mg/m2/day × 7 days) and daunorubicin (DNR, 50 mg/m2/day × 5 days) were administered intravenouslyas induction therapy from day 4. She had three courses of consolidation
 (a)
(a) (b)
(b)
Figure 1. Clinical findings: (a) Ecchymoses of the lower leg; (b) Trismus and pericoronitis of the left lower wisdom tooth.
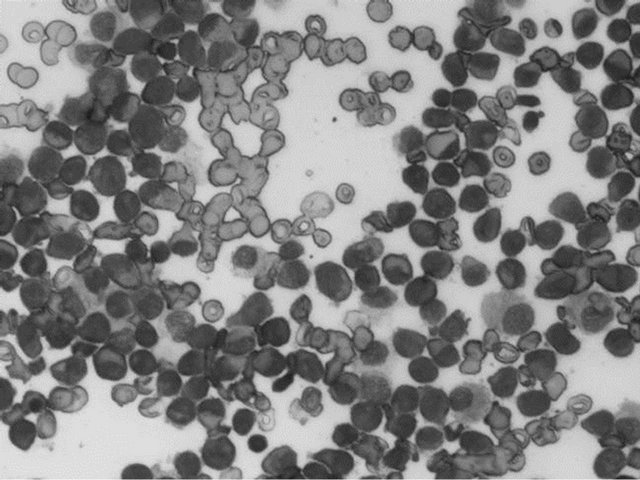
Figure 2. Histopathological findings of bone marrow aspiration shows neoplastic promyelocytes (original magnification ×40).
chemotherapyat monthly intervals. Ara-C (200 mg/m2/day × 5 days) and mitoxantrone (MIT, 7 mg/m2/day × 3 days) were administered intravenously at the first consolidation chemotherapy, Ara-C (200 mg/m2/day × 5 days) and DNR (50 mg/m2/day × 3 days) were administered at the second consolidation chemotherapy, and high-dose Ara-C (4000 mg/m2/day × 5 days) was administered at the last consolidation chemotherapy. The patient’s symptoms improved dramatically and bone marrow examination
Table 1. Hematological findings.
showed that the patient was in complete remission (CR). Maintenance therapy with at ATRA 45 mg/m2/day × 14 days per oral has been performed every three months. We performed frequent oral care of the patient and pericoronitis could be managed with local debridement. The patient has maintained clinical and molecular CR and a healthy oral cavity at 12 months of follow-up.
3. DISCUSSION
APL is a subtype of acute myeloid leukemia (AML) characterized by infiltration of bone marrow by dysplastic promyelocytes, a unique t(15;17) chromosomal translocation that generates a fusion transcript joining the PML (promyelocyte) and RAR-α (retinoic acid receptor-α) genes, and frequent association with bleeding disorders secondary to DIC [13]. Early detection of APL is important because of the high risk of early death due to severe hemorrhagic events, but current therapy with ATRA, which is a form of vitamin A, combined with chemotherapy results in 70% to 90% survival and disease-free outcome after five years [11,13].
We have described an APL case with gingival bleeding and pericoronitis leading to the diagnosis. Oral manifestations of APL are clinically similar to those in other types of acute leukemia and usually arise from underlying thrombocytopenia, neutropenia, or impaired function. Various leukemia-induced oral changes, including mucosal pallor, ecchymoses, bleeding, ulceration, gingival enlargement, trismus, mental nerve neuropathy, facial palsy, and infections, have been reported [1-12]. Proliferation of the atypical white blood cells which do not have a normal function might cause the immunocompromised conditions with decrease of normal leukocytesand become a contributing factor for some oral manifestations. Mechanism for the development of neuropathy is not well understood, but direct nerve invasion of tumor cells is thought to be a possible cause. The incidence of oral manifestations in leukemias has been reported to vary from 18% to 80% [12]. Therefore, dentists can sometimes play an important as being the first to identify the symptoms of acute leukemia and to record systemic disease-oriented information leading to diagnosis, and they should be aware of the clinical manifestations of acute leukemia [11]. Early recognition of clinical findings in the oral cavity and investigation into potential systemic causes may reveal an underlying systemic disease and lead to its timely diagnosis and management [10]. Moreover, dentists should be familiar with the therapeutic interventions for these malignant neoplastic diseases and the treatment-related oral complications. In this case, frequent oral care was performed during and after treatment, and a healthy oral cavity was maintained at 12 months of follow-up. Dental professionals have a role in the comprehensive management of patients with these malignant neoplastic diseases before, during and after treatment [5,9,10].
4. CONCLUSION
Oral manifestations of acute leukemia are often the first indications of disease. Dental professionals should be aware of clinical manifestations and complications associated with these malignant neoplastic diseases to aid in diagnosis and subsequent treatment and management.
REFERENCES
- Takagi, M., Sakota, Y., Ishikawa, G., et al. (1978) Oral manifestations of acute promyelocytic leukemia. Journal of Oral Surgery, 36, 589-593.
- Bressman, E., Decter, J.A., Chasens, A.I., et al. (1982) Acute myeloblastic leukemia with oral manifestations. Report of a case. Oral Surgery, Oral Medicine, Oral Pathology, 54, 401-403. doi:10.1016/0030-4220(82)90386-3
- Vinckier, F. and Declerck, D. (1989) Oral manifestationsin leukemic children and theirdiagnostic value. Acta Stomatologica Belgica, 86, 219-226.
- Weckx, L.L., Hidal, L.B. and Marcucci, G. (1990) Oral manifestations of leukemia. Ear, Nose & Throat Journal, 69, 341-346.
- Nikoui, M. and Lalonde, B. (1996) Oro-dental manifestations of leukemia in children. Journal of the Canadian Dental Association, 62, 443-450.
- Hiraki, A., Nakamura, S., Abe, K., et al. (1997) Numb chin syndrome as an initial symptom of acute lymphocytic leukemia: Report of three cases. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 83, 555-561. doi:10.1016/S1079-2104(97)90120-7
- Cooper, C.L., Loewen, R. and Shore, T. (2000) Gingival hyperplasia complicating acute myelomonocyticleukemia. Journal of the Canadian Dental Association, 66, 78-79.
- Katz, J. and Peretz, B. (2002) Trismus in a 6-year-old child: A manifestation of leukemia? Journal of Clinical Pediatric Dentistry, 26, 337-339.
- Demirer, S., Ozdemir, H., Sencan, M., et al. (2007) Gingival hyperplasia as an early diagnostic oral manifestation in acute monocytic leukemia: A case report. European Journal of Dentistry, 1, 111-114.
- Fatahzadeh, M. and Krakow, A.M. (2008) Manifestation of acute monocytic leukemia in the oral cavity: A case report. Special Care in Dentistry, 28, 190-194. doi:10.1111/j.1754-4505.2008.00039.x
- Suárez-Cuenca, J.A., Arellano-Sánchez, J.L., ScherlingOcampo, A.A., et al. (2009) Rapidly progressing, fatal and acute promyelocyticleukaemia that initially manifested as a painful third molar: A case report. Journal of Medical Case Reports, 3, 102. doi:10.1186/1752-1947-3-102
- Adeyemo, T.A., Adeyemo, W.L., Adediran, A., et al. (2011) Orofacial manifestation of hematological disorders: Hemato-oncologic and immuno-deficiency disorders. Indian Journal of Dental Research, 22, 688-697. doi:10.4103/0970-9290.93458
- Bassi, S.C. and Rego, E.M. (2012) Molecular basis for the diagnosis and treatment of acute promyelocytic leukemia. Revista Brasileira de Hematologia e Hemoterapia, 34, 134-139.

