H. KAKIZAKI ET AL. 149
tended to the inferior orbital rim through the retro-septal
plane. The periosteum was then incised. Malleable re-
tracto r was used to expo se the surgical field. The inferior
and lateral orbital rims, orbital floor, lateral orbital wall,
zygomatic arch and the zygomatic pr ocess of the maxilla
were sufficiently exposed (Figure 2(b)). We pulled up
the concaved zygomatic arch and reduced the zygomatic
bone (Figure 2(c)). The bone was fixed with absorbable
plates (Super FIXORB®, Takiron Co., LTD. Osaka, Ja-
pan) (Figure 2(d)). The lateral canthal band was the re-
approximated and the skin was closed (Figure 2(e)).
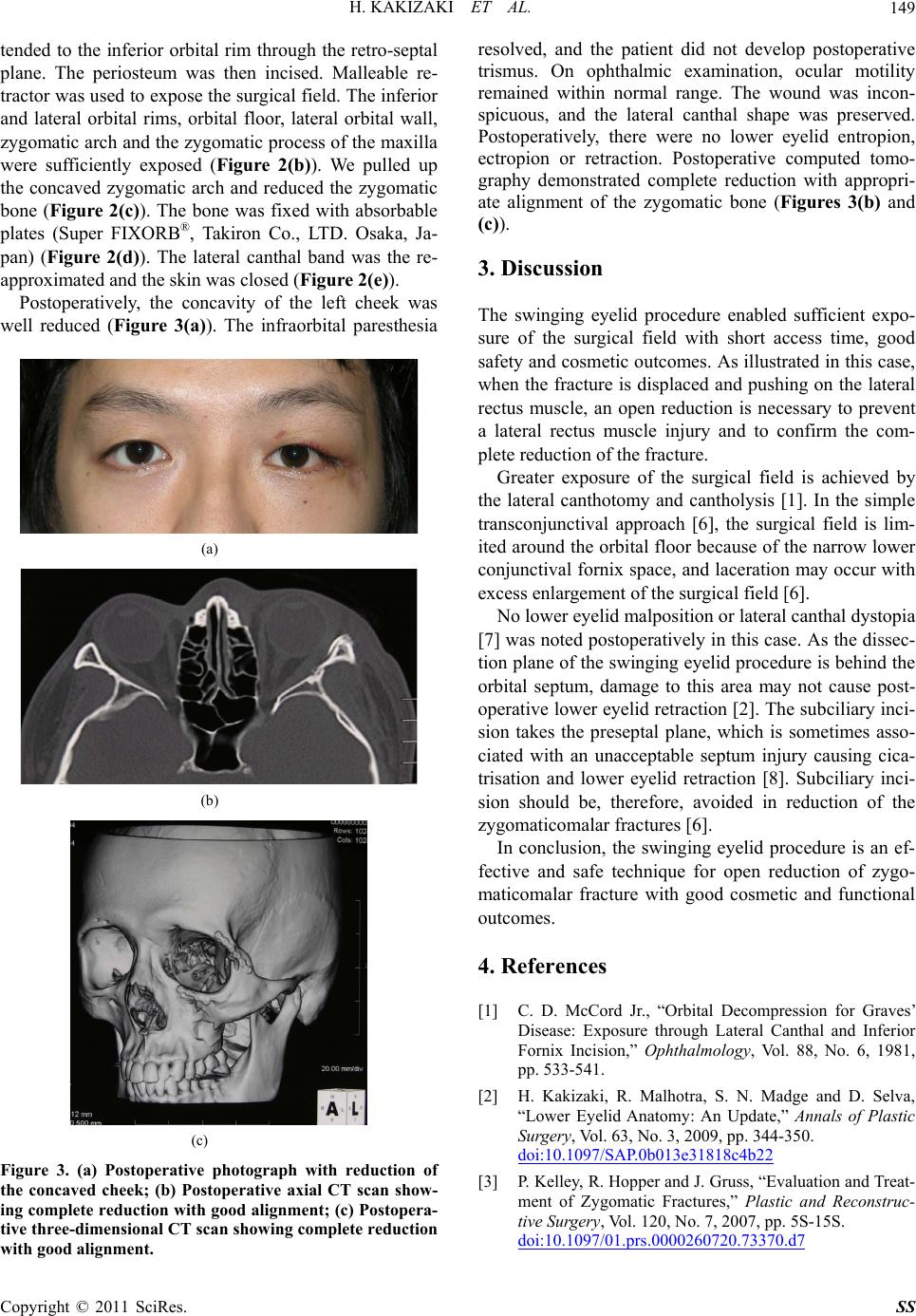
Postoperatively, the concavity of the left cheek was
well reduced (Figure 3(a)). The infraorbital paresthesia
(a)
(b)
(c)
Figure 3. (a) Postoperative photograph with reduction of
the concaved cheek; (b) Postoperative axial CT scan show-
ing complete reduction with good alignment; (c) Postopera-
tive three-dimensional CT scan showing complete reduction
with good alignment.
resolved, and the patient did not develop postoperative
trismus. On ophthalmic examination, ocular motility
remained within normal range. The wound was incon-
spicuous, and the lateral canthal shape was preserved.
Postoperatively, there were no lower eyelid entropion,
ectropion or retraction. Postoperative computed tomo-
graphy demonstrated complete reduction with appropri-
ate alignment of the zygomatic bone (Figures 3(b) and
(c)).
3. Discussion
The swinging eyelid procedure enabled sufficient expo-
sure of the surgical field with short access time, good
safety and cosmetic ou tcomes. As illustrated in this case,
when the fracture is displaced and pushing on the lateral
rectus muscle, an open reduction is necessary to prevent
a lateral rectus muscle injury and to confirm the com-
plete reduction of the fracture.
Greater exposure of the surgical field is achieved by
the lateral canthotomy and cantholysis [1]. In the simple
transconjunctival approach [6], the surgical field is lim-
ited around the orbital floor because of the narrow lower
conjunctival fornix space, and laceration may occur with
excess enlargement of the surgical field [6].
No lower eyelid malposition or lateral canthal dystopia
[7] was noted postoperatively in this case. As the dissec-
tion plane of the swinging eyelid procedure is behind the
orbital septum, damage to this area may not cause post-
operative lower eyelid retraction [2]. The subciliary inci-
sion takes the preseptal plane, which is sometimes asso-
ciated with an unacceptable septum injury causing cica-
trisation and lower eyelid retraction [8]. Subciliary inci-
sion should be, therefore, avoided in reduction of the
zygomaticomalar fractures [6].
In conclusion, the swinging eyelid procedure is an ef-
fective and safe technique for open reduction of zygo-
maticomalar fracture with good cosmetic and functional
outcomes.
4. References
[1] C. D. McCord Jr., “Orbital Decompression for Graves’
Disease: Exposure through Lateral Canthal and Inferior
Fornix Incision,” Ophthalmology, Vol. 88, No. 6, 1981,
pp. 533-541.
[2] H. Kakizaki, R. Malhotra, S. N. Madge and D. Selva,
“Lower Eyelid Anatomy: An Update,” Annals of Plastic
Surgery, Vol. 63, No. 3, 2009, pp. 344-350.
doi:10.1097/SAP.0b013e31818c4b22
[3] P. Kelley, R. Hopper and J. Gruss, “Evaluation and Treat-
ment of Zygomatic Fractures,” Plastic and Reconstruc-
tive Surgery, Vol. 120, No. 7, 2007, pp. 5S-15S.
doi:10.1097/01.prs.0000260720.73370.d7
C
opyright © 2011 SciRes. SS