S. PIPARSALIYA ET AL.
136
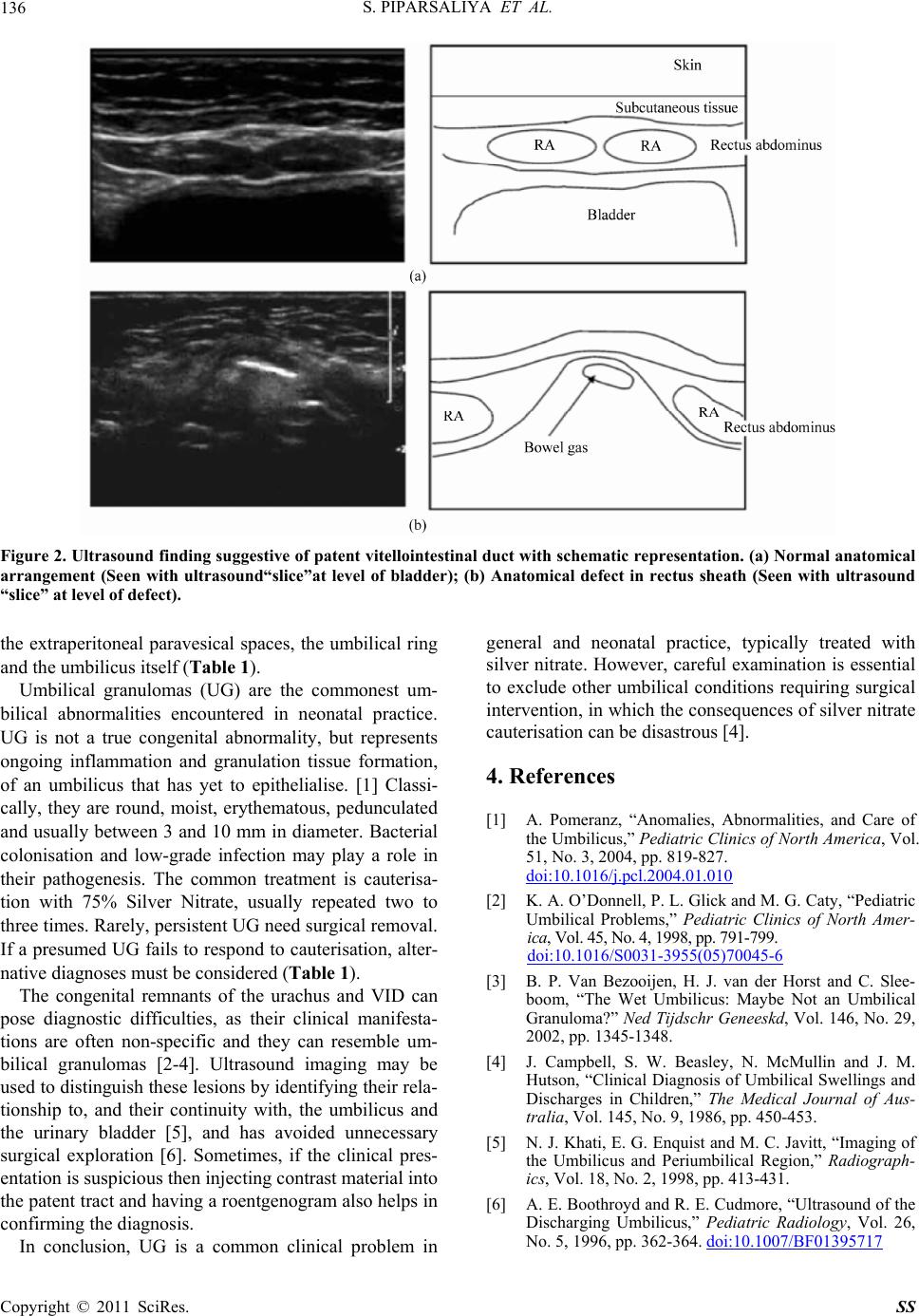
Figure 2. Ultrasound finding suggestive of patent vitellointestinal duct with schematic repr esentation. (a) Normal anatomical
arrangement (Seen with ultrasound“slice”at level of bladder); (b) Anatomical defect in rectus sheath (Seen with ultrasound
“slice” at level of defec t) .
the extraperitoneal paravesical spaces, the umbilical ring
and the umbilicus itself (Table 1).
Umbilical granulomas (UG) are the commonest um-
bilical abnormalities encountered in neonatal practice.
UG is not a true congenital abnormality, but represents
ongoing inflammation and granulation tissue formation,
of an umbilicus that has yet to epithelialise. [1] Classi-
cally, they are round, moist, erythematous, pedunculated
and usually between 3 and 10 mm in diameter. Bacterial
colonisation and low-grade infection may play a role in
their pathogenesis. The common treatment is cauterisa-
tion with 75% Silver Nitrate, usually repeated two to
three times. Rarely, persistent UG need surgical removal.
If a presumed UG fails to respond to cauterisation, alter-
native diagnoses must be considered (Table 1).
The congenital remnants of the urachus and VID can
pose diagnostic difficulties, as their clinical manifesta-
tions are often non-specific and they can resemble um-
bilical granulomas [2-4]. Ultrasound imaging may be
used to distinguish these lesions by identifying their rela-
tionship to, and their continuity with, the umbilicus and
the urinary bladder [5], and has avoided unnecessary
surgical exploration [6]. Sometimes, if the clinical pres-
entation is susp icious then injecting contrast material into
the patent tract and having a roentgenogram also helps in
confirming the diagnosis.
In conclusion, UG is a common clinical problem in
general and neonatal practice, typically treated with
silver nitrate. However, careful examination is essential
to exclude other umbilical conditions requiring surgical
intervention, in wh ich the consequences of silver nitrate
cauterisation ca n be di sast r ous [4] .
4. References
[1] A. Pomeranz, “Anomalies, Abnormalities, and Care of
the Umbilicus,” Pediatric Clinics of North America, Vol.
51, No. 3, 2004, pp. 819-827.
doi:10.1016/j.pcl.2004.01.010
[2] K. A. O’Donnell, P. L. Glick and M. G. Caty, “Pediatric
Umbilical Problems,” Pediatric Clinics of North Amer-
ica, Vol. 4 5, N o. 4, 1 998, p p. 791 -799.
doi:10.1016/S0031-3955(05)70045-6
[3] B. P. Van Bezooijen, H. J. van der Horst and C. Slee-
boom, “The Wet Umbilicus: Maybe Not an Umbilical
Granuloma?” Ned Tijdschr Geneeskd, Vol. 146, No. 29,
2002, pp. 1345-1348.
[4] J. Campbell, S. W. Beasley, N. McMullin and J. M.
Hutson, “Clinical Diagnosis of Umbilical Swellings and
Discharges in Children,” The Medical Journal of Aus-
tralia, Vol. 145, No. 9, 1986, pp. 450-453.
[5] N. J. Khati, E. G. Enquist and M. C. Javitt, “Imaging of
the Umbilicus and Periumbilical Region,” Radiograph-
ics, Vol. 18, No. 2, 1998, pp. 413-431.
[6] A. E. Boothroyd and R. E. Cudmore, “Ultrasound of the
Discharging Umbilicus,” Pediatric Radiology, Vol. 26,
No. 5, 1996, pp. 362-364. doi:10.1007/BF01395717
Copyright © 2011 SciRes. SS